Abstract
Background
Pediatric inflammatory bowel disease (IBD) presents with extensive phenotype. The aim of this study was to determine the phenotype of pediatric IBD patients in Croatia at diagnosis and follow-up.
Methods
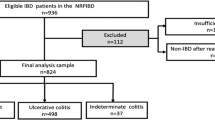
Children were prospectively recruited into Croatian IBD national registry. Data on diagnostic evaluation, therapy and 1-year follow-up were collected.
Results
A total of 51 newly diagnosed patients were recruited (19 Crohn’s disease (CD), 28 ulcerative colitis (UC) and 4 IBD-unclassified (IBD-U)). Most common location in CD was ileocolonic disease (52.6%), and pancolitis in UC (53.6%). The recommended complete diagnostic algorithm was performed only in 29.4% of patients. First-line therapy used in CD was exclusive enteral nutrition for remission induction (84.2%) and azathioprine for maintenance (73.7%). In patients with UC, aminosalicylates were the most common drug used (89.3%). By the end of the first year 41.2% of CD and 53.9% of UC patients had one or more relapses and required treatment escalation.
Conclusion
Our data confirm extensive intestinal involvement in pediatric IBD and relatively high relapse rate during the first year of follow-up. More effort should be invested on the national level to implement more stringent adherence to the current European guidelines.
Impact
-
The key message of our article is that pediatric IBD in Croatia shows extensive intestinal involvement with high relapse rates in first year of follow-up.
-
It is the first cohort study reporting on the phenotype of pediatric IBD in Croatia, but also investigates adherence to diagnostic and therapeutic European guidelines which is not commonly reported.
-
The study is national based, thus having the greatest impact on Croatian health care,stressing out that more effort should be invested on the national level to implement more stringent adherence to the current European guidelines.
Similar content being viewed by others
Introduction
Inflammatory bowel disease (IBD), comprising of Crohn’s disease (CD), ulcerative colitis (UC) and IBD-unclassified (IBD-U), is a chronic inflammatory disorder of the gastrointestinal (GI) tract with rising incidence in the pediatric population.1 Approximately 15–25% of all IBD present during childhood,2 with a more extensive disease phenotype and more severe clinical course than in adult-onset disease.3,4 Furthermore, disease management should enable optimal growth and psychosocial development.
Given specific features of pediatric inflammatory bowel disease (PIBD), accurate disease classification is necessary. Thus, in 2011, Paris Classification,5 a pediatric modification of the Montreal classification,6 was adopted. It contains more detailed subgroups related to age at diagnosis, location and severity of disease and existence of growth retardation,5 which enabled detection of phenomena typical for pediatric population.7
According to the Paris Classification,5 the most common CD phenotype in children is ileocolonic disease (L3) with higher proportion of colonic involvement (L2) in younger children, whereas inflammation in adolescents is mainly limited to the terminal ileum (L1).3 Upper GI tract involvement is found in one third of the children, which is more common than in adults.3 Children with UC also mostly present with extensive disease form—pancolitis (E4),8,9 though in 5–10% of the patients with extensive disease, rectum can macroscopically seem spared.7,8 Unlike adults, the disease in children has shown tendency to spread over time, and recurrent exacerbations in CD change the disease behavior from inflammatory to stricturing and penetrating form.10,11
The aim of therapy in IBD is not only the induction and maintenance of remission, but also supporting adequate growth, especially in patients with CD. Evidence-based guidelines on the diagnostic algorithms, treatment and surveillance of PIBD have been developed and are regularly updated,12,13,14 but the question remains whether clinicians adhere to these guidelines and to which extent. It is well known that mild disease at diagnosis, early diagnosis and timely initiated disease-stage adapted management improve the ultimate prognosis for both CD15,16 and UC.17,18 This is of particular importance in view of the latest data on mortality of childhood onset IBD, with IBD, in general, carrying three times higher mortality risk (hazard ratio (HR) 3.2), and the UC being addressed as the most serious threat increasing mortality risk four times (HR 4.0).19
Epidemiological data on PIBD in Croatia are available only since 2016, when a Croatian national registry for PIBD was established. Data from the registry enabled determining national incidence of PIBD, and noted regional differences in incidence rates, thus confirming the existence of a north to south decreasing gradient in Croatia (unpublished data).
The aim of the registry was also to investigate, for the first time, data on phenotype of PIBD in Croatia, as well as national diagnostic and therapeutic approaches. Therefore, the primary aim of this study was to describe prevailing disease phenotype for CD and UC in children in our country. The secondary aims were to investigate diagnostic and therapeutic approaches in Croatia in view of the current European guidelines,12,13,14 and to describe early disease-course through 1-year follow-up data.
Materials and methods
Study design
This was a prospective study recruiting children (age 0–18 years) with newly diagnosed IBD, from June 1, 2016 to May 31, 2017, into a newly developed Croatian national pediatric IBD registry. The registry was established in 2016 as an online database, collecting required data from all Croatian centers that diagnose and treat pediatric patients with IBD. A detailed description of the registry establishment, its layout and the process of data collecting are presented elsewhere (unpublished data).
The IBD diagnosis was made according to the revised Porto criteria.14 Location and phenotype of the disease were based on the Paris classification.5 The nutritional status was determined at the time of diagnosis based on the Z-score of body mass index (BMI) for the age, which is a deviation of BMI from the population mean according to the World Health Organization (WHO) 2007 standards (https://www.who.int/growthref/who2007_bmi_for_age/en/). Stunted growth was defined as a Z-score of height for age more than two standard deviations below the WHO 2007 standards. Disease relapse was determined by the assigning physician based on relevant clinical data—child’s clinical condition, need for the introduction of remission induction therapy or need for the escalation in maintenance therapy, activity index scores showing active disease,20,21,22 and increased inflammatory markers.
Statistical analysis
Statistica software version 13.4 (TIBCO Software Inc. (2018)) was used for the required analysis. An analysis of the normality of data distribution was performed with the Kolmogorov−Smirnov test, and appropriate parametric or nonparametric tests were selected based on the analysis. Age at diagnosis (years) and time elapsed between symptoms occurrence and diagnosis (months) were presented as the median with the range. χ2 test was used for category data and comparison of continuous variables was analyzed by Student’s t, Mann−Whitney, Kruskal−Wallis, ANOVA test and Spearman correlation. All p values < 0.05 were determined to be statistically significant.
The study was approved by the Ethics Committee of the Children’s Hospital Zagreb (02-26/10-4-15).
Results
Clinical presentation
A total of 51 children with newly diagnosed IBD were identified; 19 (37.3%) of them with CD, 28 (54.9%) with UC and four (7.8%) had IBD-U. Median age at diagnosis was 14.8 (5.4–17.8) years. Median duration of symptoms before diagnosis was 2 (0.2–24) months but differed in respect to the IBD type; 5 (1–14) months for CD and 2 (0.2–24) months for UC, without statistically significant difference (p = 0.253). Symptoms at diagnosis in respect to IBD type are presented in Fig. 1. Bloody stools occurred significantly more frequent in patients with UC (UC 92.6% vs. CD 31.6%, p < 0.001), while weight loss was more common in patients with CD (CD 68.4% vs. UC 32.1%, p = 0.006). Extraintestinal manifestations (EIM) were found in 25% (N = 13) of our patients, equally emerging in CD (21.5%) and UC (21%), and in three out of four patients with IBD-U. Overall 6/51 (11.8%) patients—five with UC and one with IBD-U had liver disease (three had unspecified liver lesion, two had autoimmune hepatitis, and one autoimmune sclerosing cholangitis). Arthritis was found in five (9.8%) patients, two with CD, two with UC and one with IBD-U. Erythema nodosum was found in two (3.9%) patients, one of them had CD and the other IBD-U. Aphthous stomatitis was found in one (1.9%) patient with CD. Nutritional status in respect to IBD type, according to WHO’s growth reference (https://www.who.int/growthref/who2007_bmi_for_age/en/), is presented in Fig. 2. Z-score BMI for age did not differ significantly in respect to IBD type (p = 0.238), gender (p = 0.942) or age (p = 0.706).
Diagnostic procedure
Complete diagnostic procedure following the current European guidelines14 was performed only in 15 (29.4%) patients. Lower GI endoscopy was performed in all subjects, however, without terminal ileum intubation in 12 (23.5%) patients. Esophagogastroduodenoscopy (EGD) was performed in 42 (82.4%) patients. Biopsy specimens were not collected from all parts of GI tract during 50% of EGDs, and 17.9% of total colonoscopies. Abdominal ultrasound was done in as much as 27 (52.9%) patients. MR-enterography was performed in 19 (37.2%) patients, more frequently in CD (52.36%), as opposed to UC (25%) (p = 0.135). Small bowel follow-through (SBFT) was not performed in any of our patients and capsule endoscopy was performed in two.
Disease classification
Crohn’s disease
Most patients (12/19) diagnosed with CD were in the age group between 10 and 17 years of age (Table 1). The most frequent location was ileocolonic disease (L3) found in ten (52.6%) patients. The form of disease was inflammatory (B1) in 13 (68.4%) patients and four (21.1%) had stricturing disease (B2), while the data for two patients were not available. Upper GI abnormalities were common—present at diagnosis in eight (42.1%) CD patients, with one patient (5.3%) having isolated upper GI disease. Perianal disease was present in seven (36.8%) children. Growth delay, based on the assessment of the attending physician, was recorded in three (15.8%) patients with CD. However, stunted growth based on anthropometric measures at the time of diagnosis was found overall in only one (1.96%) patient with CD.
Ulcerative colitis
Seventeen patients had extensive disease (E3 + E4) (61.7%) with 15 (53.6%) of them presenting with pancolitis (E4), and two (7.1%) had severe form of UC (S1) (Table 2).
Therapy
Majority of patients with CD received EEN as a first remission induction therapy (N = 16, 84.2%), other patients received corticosteroids. EEN failure was noted in four (25%) patients who were additionally treated with steroids. In 14 (73.7%) CD patients, azathioprine was used as a first maintenance therapy.
In patients with UC, peroral mesalazine was most commonly administered as the first remission induction therapy at diagnosis (N = 25, 89.3%), and in ten (39.2%) patients it was combined with topical preparation. Corticosteroids were used as a first remission induction therapy in eight (28.6%) patients with concomitant administration of systemic mesalazine.
One-year follow-up
In comparison to initial data, which were available for 51 patients, the follow-up data were available for 46 (90.2%) patients (17 with CD, 26 with UC, and 3 with IBD-U). At the end of the first year 7/17 (41.2%) patients with CD had one or more relapse, four (23.5%) patients with CD had one and three (17.7%) patients had two relapses each. Median time to the first relapse was 5 (0.5–10) months. Two (10.5%) patients required surgical treatment of gluteal and perianal abscess. Three (17.6%) patients required escalation of treatment to biological therapy.
In the UC cohort, 14/26 (53.8%) patients had one or more relapse, 12 (46.2%) of them had one and two (7.6%) of them had three relapses each, with the remaining 12 (46.2%) being in remission by the end of the follow-up. Median time to the first relapse was 5 (2–11) months. None of the patients with UC needed surgical treatment. Biologic therapy was administered to two (7.7%) patients. Comparison between initial maintenance therapy and therapy after 1-year follow-up for CD and UC is presented in Fig. 3. Logistic regression model was used to examine the potential risk factors for relapse. The following parameters were included: age (p = 0.769), gender (p = 0.091), Z-score BMI for age (p = 0.914), Z-score height for age (p = 0.087), Pediatric Crohn’s Disease Activity Index (PCDAI) (p = 0.947), Pediatric Ulcerative Colitis Activity Index (PUCAI) (p = 0.245), EEN (p = 0.605). None of the examined parameters was statistically significant, although gender and Z-score height for age reached the borderline statistical significance.
Discussion
This is the first study to investigate a disease phenotype of PIBD in Croatia, as well as to show data on the adherence to the European guidelines on disease diagnosis and treatment.12,13,14
Clinical presentation of our patients at diagnosis was similar to previously published data.10 CD patients most commonly presented with abdominal pain, diarrhea and weight loss, while UC patients most often presented with bloody diarrhea. Occurrence of nonspecific symptoms in CD, such as weight loss, fever and nonspecific periumbilical, can be a reason for longer diagnostic delays, while presence of blood in the stool and painful tenesmus, typical of UC, led to prompt medical intervention.23,24 The same has been observed in our cohort, since the median time from the symptom onset to the diagnosis was 5 months for CD and only 2 months for UC, although not statistically significant.
Regarding disease phenotype, children with CD in our study presented with extensive disease form, affecting small and large intestine. This is typical for pediatric onset CD, while in adult patients CD most commonly affects terminal ileum only, and very occasionally the upper GI tract.3 More than half of our subjects had ileocolonic disease (L3), and 42.1% of them had the upper GI tract involvement which is very similar to data obtained from the EUROKIDS registry.3 Our patients initially presented with nonstricturing and nonpenetrating form (B1) in more than two thirds while the others recorded had a stricturing disease (B2). The data on disease form were not available for two patients. Unlike EUROKIDS registry that reported occurrence of penetrating (B3, 5%) and both stricturing and penetrating disease (B2B3, 2%) at diagnosis, those phenotypes were not found in our patients, which could probably be explained by a relatively small sample size. Our data revealed significantly higher rates of perianal disease than earlier reported (36.8% vs. 9%),3 but fistulae and abscesses were found in only four (21.1%) patients. Stunted growth was found only in one (1.96%) patient, which is less than recently reported in the literature (9–24%).11 In previous decades, growth retardation and delayed puberty were typical features of Crohn’s disease, diagnosed on average in every third child,25 and in 50% of them even before occurrence of any other symptom of CD.26 However, recent data are more favorable.3,11 In our cohort 24% of patients were malnourished (18% mildly, 2% moderately, and 4% severely), similar to a recent study from the Netherlands.27 Although malnutrition is considered a greater problem in children with CD,28 even when the disease is in remission,29 our results did not show significant differences in respect to IBD type, gender or age. These results could be at least partially explained by short time interval from symptoms’ onset to diagnosis.
As for the UC, pancolitis at diagnosis was present in more than half of our patients (E4). Although this was the commonest phenotype in our cohort, some studies reported occurrence of pancolitis in up to 80–90% of their pediatric patients.8,9 This difference could be ascribed to the very short delay from the symptoms’ onset to the diagnosis in our patients with UC.
Extraintestinal manifestations were found in 25% of our patients, which is slightly higher than previously reported.3,24,30 Erythema nodosum and aphthous stomatitis were typically found only in patients with CD,30 whereas liver involvement24,30 was found in almost all of our UC patients with EIM (5 out of 6). Unlike previous studies that showed higher prevalence of arthritis in CD,30 it equally affected our patients with CD and UC. However, number of patients with EIMs was small, and should be interpreted with caution.
The most disappointing finding from our registry is that the proposed diagnostic algorithms were not adequately followed in Croatia. The most important part of the diagnostic procedure in establishing the diagnosis of IBD is the endoscopy of both upper and lower GI tract with histological analysis of the biopsy specimens from each GI segment, even if there are no macroscopically visible lesions, followed by the radiologic imaging of the small bowel, which can be omitted only in case of a typical UC.14 The recommended diagnostic algorithm was consistently applied only in 15 of our patients (29.4%). Although our result is not encouraging, other studies have suggested inconsistencies in adherence to current diagnostic guidelines and protocols as well, although not to such an extent.31,32 Esophagogastroduodenoscopy, similar to the data obtained from the EUROKIDS registry,31 was performed in more than 4/5 of our patients. It was not done in nine patients whose colonoscopy results indicated thorough suspicion of UC. All of our patients had total colonoscopy done, but in 23.5% terminal ileum was not intubated. Although a histological examination of biopsy specimens from every segment of GI tract is recommended, it was not done properly in half of the patients during EGD and 17.9% during colonoscopy. Unlike our relatively poor results, according to EUROKIDS registry, biopsy specimens from all parts of the digestive system were taken in more than 80% of subjects.31 Possible reasons for the poor adherence to the existing guidelines could be lack of adequate equipment, lack of skills required to intubate terminal ileum, and difficulties in organizing general anesthesia, required particularly in younger children.
Golden standard for small bowel imaging in the newly proposed diagnostic algorithm, MR-enterography,14 was performed in only 37.2% of our patients, although more often when CD was diagnosed. Reasons for the rare use of MR-enterography in diagnostic work-up may be the cost of examination, and the long waiting lists. In contrast to our data, in the EUROKIDS registry, adequate small bowel imaging was reported in 87% of respondents. MR-enterography was performed less often (29%), but other methods such as SBFT (58%)—which was not performed in any of our patients, abdominal computed tomography (CT), capsule endoscopy and enteroscopy were done. However, frequency of SBFT has decreased over the years due to radiation exposure31 and is therefore not proposed in the new guidelines.14
Unlike diagnostic procedure guidelines, guidelines for therapy were followed in the majority of cases. Regarding the first treatment option in CD, EEN was used as a first-line therapy in more than 4/5 of patients with CD as opposed to other studies where EEN was used much less frequently.33 Its efficacy was confirmed in our study as well, since remission was achieved in 75% of children. Consistent with the guidelines,13 azathioprine was most commonly used for the maintenance of remission (approximately 3/4 of patients). Methotrexate with folic acid was used in two of our patients and biological therapy was administered to subjects whose remission was not achieved by standard therapy. Regarding therapy for active UC, according to the recommendations,14 our patients were most often initially treated with aminosalicylates (mesalazine), while corticosteroid therapy had been used in just under a third of patients, which is less often than in other similar studies.34 Almost all subjects who received corticosteroid therapy had pancolitis, although only one of them had a severe acute form of the disease at presentation. Aminosalicylates were used to maintain remission in almost 90% of children, either as a monotherapy or in combination with topical preparation, which is consistent with the recommendations and results of similar studies, while other 10% of children required azathioprine.14,34
Early disease-course, in our study, was investigated through check-ups 6 and 12 months after establishing the diagnosis. Relapse and surgical treatment rates as well as alteration of maintenance therapy were recorded. Six months after the diagnosis, approximately one third of our patients (36.8% of children with CD, 35.7% with UC, and 1 of 4 patients diagnosed with IBD-U) had one or more relapses, which is a relatively high percentage. However, after 1-year follow-up, approximately 50% of them were in stable remission, without any relapse (CD 58.8%, UC 46.2%, IBD-U 33.3%). Reported 1-year relapse rates in pediatric CD vary from 28 to 70%, although longer sustained remission is found in patients who achieved mucosal healing.35 As for patients with UC, Italian study36 found 63% probability of developing relapse in the first year, which is similar to our results. Our study examined numerous risk factors for relapse, including EEN treatment in CD, which was earlier associated with the negative risk for relapse,37 but none of them was found significant. None of our patients required intestinal resection, although two patients with CD needed surgical treatment of disease complications (gluteal and perianal abscess). Over a course of 1 year, maintenance therapy was expectedly altered. Thus, in CD, azathioprine was in 23% of children replaced by methotrexate or biological therapy (infliximab). In UC patients, mesalazine use, which was administered initially in more than 3/4 of patients, insignificantly decreased (78.6% vs. 74.1%), while the administration of azathioprine increased (10.7% vs. 33.3%). 17.6% of our patients with CD and 7.7% of those with UC, at the end of the follow-up, received biologics, while its administration was reported in up to one third of patients in other studies.18
In respect to the strength of evidence, data obtained from the registries are usually rated as the second best (after double-blind randomized studies).38 Despite that, our study has several limitations: (a) the sample size is relatively small; (b) the follow-up of 1 year is not long enough to detect the natural history of the disease; (c) the poor adherence to the diagnostic algorithm could affect the results, particularly the number of CD vs. UC patients, and the phenotypic features. However, this is the first report on the PIBD phenotype in Croatian patients, which adds important data on the disease-course over the period of 1 year. Furthermore, data on the adherence to diagnostic and therapeutic protocols were presented, which is not frequently investigated even in developed countries.
In conclusion, there is a high prevalence of extensive disease phenotype and high relapse rate within the first 6 months from diagnosis, but growth retardation and undernutrition are uncommon in Croatian PIBD patients. Most discouraging result is the low adherence to the diagnostic guidelines. Therefore, more effort should be invested on the national level to implement more stringent adherence to the current European guidelines.
References
Sýkora, J. et al. Current global trends in the incidence of pediatric-onset inflammatory bowel disease. World J. Gastroenterol. 24, 2741–2763 (2018).
Dubinsky, M. Special issues in pediatric inflammatory bowel disease. World J. Gastroenterol. 14, 413–420 (2008).
de Bie, C. I. et al. Disease phenotype at diagnosis in pediatric Crohn’s disease: 5-year analyses of the EUROKIDS Registry. Inflamm. Bowel Dis. 19, 378–385 (2013).
Duricova, D. et al. Age-related differences in presentation and course of inflammatory bowel disease: an update on the population-based literature. J. Crohns Colitis 8, 1351–1361 (2014).
Levine, A. et al. Pediatric modification of the Montreal classification for inflammatory bowel disease: the Paris classification. Inflamm. Bowel Dis. 17, 1314–1321 (2011).
Silverberg, M. S. et al. Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a Working Party of the 2005 Montreal World Congress of Gastroenterology. Can. J. Gastroenterol. 19(Suppl A), 5A–36A (2005).
Levine, A. et al. Atypical disease phenotypes in pediatric ulcerative colitis: 5-year analyses of the EUROKIDS Registry. Inflamm. Bowel Dis. 19, 370–377 (2013).
Heyman, M. B. et al. Children with early-onset inflammatory bowel disease (IBD): analysis of a pediatric IBD consortium registry. J. Pediatr. 146, 35–40 (2005).
Sawczenko, A. & Sandhu, B. K. Presenting features of inflammatory bowel disease in Great Britain and Ireland. Arch. Dis. Child. 88, 995–1000 (2003).
Malmborg, P. & Hildebrand, H. The emerging global epidemic of paediatric inflammatory bowel disease—causes and consequences. J. Intern. Med. 279, 241–258 (2016).
Duricova, D. et al. The natural history of Crohn’s disease in children: a review of population-based studies. Eur. J. Gastroenterol. 29, 125–134 (2017).
Ruemmele, F. M. et al. European Crohn’s and Colitis Organisation; European Society of Pediatric Gastroenterology, Hepatology and Nutrition. Consensus guidelines of ECCO/ESPGHAN on the medical management of pediatric Crohn’s disease. J. Crohns Colitis 8, 1179–1207 (2014).
Turner, D. et al. European Crohn’s and Colitis Organization; European Society for Paediatric Gastroenterology, Hepatology, and Nutrition. Management of pediatric ulcerative colitis: joint ECCO and ESPGHAN evidence-based consensus guidelines. J. Pediatr. Gastroenterol. Nutr. 55, 340–361 (2012).
Levine, A. et al. ESPGHAN revised porto criteria for the diagnosis of inflammatory bowel disease in children and adolescents. J. Pediatr. Gastroenterol. Nutr. 58, 795–806 (2014).
Cohen-Dolev, N. et al. Differences in outcomes over time with exclusive enteral nutrition compared with steroids in children with mild to moderate crohn’s disease: results from the GROWTH CD Study. J. Crohns Colitis 12, 306–312 (2018).
Guariso, G. & Gasparetto, M. Treating children with inflammatory bowel disease: current and new perspectives. World J. Gastroenterol. 23, 5469–5485 (2017).
Krauthammer, A. et al. Long-term outcomes of paediatric patients admitted with acute severe colitis—a multicentre study from the Paediatric IBD Porto Group of ESPGHAN. J. Crohns Colitis 13, 1518–1526 (2019).
Hyams, J. S. et al. Clinical and biological predictors of response to standardised paediatric colitis therapy (PROTECT): a multicentre inception cohort study. Lancet 393, 1708–1720 (2019).
Olén, O. et al. Increased mortality of patients with childhood-onset inflammatory bowel diseases, compared with the general population. Gastroenterology 156, 614–622 (2019).
Turner, D. et al. Development, validation, and evaluation of a pediatric ulcerative colitis activity index: a prospective multicenter study. Gastroenterology 133, 423–432 (2007).
Hyams, J. S. et al. Development and validation of a pediatric Crohn’s disease activity index. J. Pediatr. Gastroenterol. Nutr. 12, 439–447 (1991).
Leach, S. T., Nahidi, L., Tilakaratne, S., Day, A. S. & Lemberg, D. A. Development and assessment of a modified pediatric Crohn disease activity index. J. Pediatr. Gastroenterol. Nutr. 51, 232–236 (2010).
Ghione, S. et al. Dramatic increase in incidence of ulcerative colitis and Crohn’s disease (1988–2011): a population-based study of French adolescents. Am. J. Gastroenterol. 113, 265–272 (2018).
Castro, M. et al. Inflammatory bowel disease in children and adolescents in Italy: data from the pediatric national IBD register (1996–2003). Inflamm. Bowel Dis. 14, 1246–1252 (2008).
Sanderson, I. R. Growth problems in children with IBD. Nat. Rev. Gastroenterol. Hepatol. 11, 601–610 (2014).
Aloi, M. & Cucchiara, S. Extradigestive manifestations of IBD in pediatrics. Eur. Rev. Med. Pharmacol. Sci. 13(Suppl 1), 23–32 (2009).
Diederen, K., Krom, H., Koole, J. C., Benninga, M. A. & Kindermann, A. Diet and anthropometrics of children with inflammatory bowel disease: a comparison with the general population. Inflamm. Bowel Dis. 24, 1632–1640 (2018).
Kugathasan, S. et al. Body mass index in children with newly diagnosed inflammatory bowel disease: observations from two multicenter North American inception cohorts. J. Pediatr. 151, 523–527 (2007).
Forbes, A. et al. ESPEN guideline: clinical nutrition in inflammatory bowel disease. Clin. Nutr. 36, 321–347 (2017).
Dotson, J. L. et al. Extraintestinal manifestations of pediatric inflammatory bowel disease and their relation to disease type and severity. J. Pediatr. Gastroenterol. Nutr. 51, 140–145 (2010).
De Bie, C. I. et al. Diagnostic workup of paediatric patients with inflammatory bowel disease in Europe: results of a 5-year audit of the EUROKIDS registry. J. Pediatr. Gastroenterol. Nutr. 54, 374–380 (2012).
Kovacs, M., Muller, K. E. & Arato, A., Hungarian IBD Registry Group (HUPIR). Diagnostic yield of upper endoscopy in paediatric patients with Crohn’s disease and ulcerative colitis. Subanalysis of the HUPIR registry. J. Crohns Colitis 6, 86–94 (2012).
Fumery, M. et al. Long-term outcome of pediatric-onset Crohn’s disease: a population-based cohort study. Dig. Liv. Dis. 51, 496–502 (2019).
Müller, K. E. et al. Incidence, Paris classification, and follow-up in a nationwide incident cohort of pediatric patients with inflammatory bowel disease. J. Pediatr. Gastroenterol. Nutr. 57, 576–582 (2013).
Ziv‐Baran, T. et al. Response to treatment is more important than disease severity at diagnosis for prediction of early relapse in new‐onset paediatric Crohn’s disease. Aliment. Pharmacol. Ther. 48, 1242–1250 (2018).
Martinelli, M. et al. The changing face of pediatric ulcerative colitis: a population-based cohort study. J. Pediatr. Gastroenterol. Nutr. 66, 903–908 (2018).
Hojsak, I., Pavić, A. M., Mišak, Z. & Kolaček, S. Risk factors for relapse and surgery rate in children with Crohn’s disease. Eur. J. Pediatr. 173, 617–621 (2014).
Gliklich, R. E., Dreyer, N. A. & Leavy, M. B. Registries for Evaluating Patient Outcomes: A User’s Guide, 3rd edn (Agency for Healthcare Research and Quality, US, Rockville, 2014).
Acknowledgements
This study was part of a research project IP-2014-09-3788 funded by the Croatian Science Foundation.
Author information
Authors and Affiliations
Contributions
I.H. and S.K. made the concept and design of the study. L.I., I.T., S.S., V.K., I.S.-Č., G.P., O.Ž., R.D. were included in acquisition of the data. L.I., P.H., I.T., S.S., V.K., I.S.-Č., G.P., O.Ž., R.D. analyzed the data. L.I., I.H. and S.K. did the interpretation of the data. L.I., I.T. and S.S. participated in manuscript drafting. I.H. and S.K. did the critical analysis of the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
I.H. received payment/honorarium for lectures or consultation from BioGaia, Nutricia, Nestle, Chr Hansen, Biocodex, Oktal Pharma; S.K. received fees for lectures from Abbott, AbbVie, Fresenius, Mead and Johnson, Nestle, Nutricia, Oktal Pharma, Sherring; L.I., I.T., S.S., P.H., V.K., I.S.-Č., G.P., R.D. and O.Ž. declare no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ivković, L., Hojsak, I., Trivić, I. et al. IBD phenotype at diagnosis, and early disease-course in pediatric patients in Croatia: data from the Croatian national registry. Pediatr Res 88, 950–956 (2020). https://doi.org/10.1038/s41390-020-0853-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-0853-2
This article is cited by
-
Diagnostic Delay in Pediatric Inflammatory Bowel Disease: A Systematic Review
Digestive Diseases and Sciences (2022)