Abstract
Objective
Determine whether management of neonatal hyperbilirubinemia differs if one used end-tidal carbon monoxide (CO) corrected for ambient CO (ETCOc) measurements instead of direct antiglobulin test (DAT) results to assess the severity of hemolysis.
Study design
Retrospective chart review of infants with total bilirubin and ETCOc levels measured from July 2016 to August 2018. The reported treatment is the hypothetical management infants might have received had there been strict adherence to American Academy of Pediatrics guidelines, rather than the actual management they received.
Result
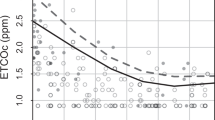
Only 27.2% of 191 DAT(+) infants were hemolyzing based on ETCOc, while 29.1% of DAT (−) infants were hemolyzing based on ETCOc. Management of 18 (9.4%) infants differed depending if ETCOc or DAT were used to determine hemolysis. Eight fewer infants would have received phototherapy if ETCOc was used.
Conclusions
ETCOc is a more accurate determinant of hemolysis in the newborn, and its use can lead to less phototherapy.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Delaney M, Matthews DC. Hemolytic disease of the fetus and newborn: managing the mother, fetus, and newborn. Hematol Am Soc Hematol Educ Program. 2015;1:146–51.
Moise KJ. Hemolytic disease of the fetus and newborn. In: Creasy RK, Resnik R, editors. Maternal-fetal medicine: principles and practice. 6th ed. Philadelphia: WB Saunders; 2008, p. 477–503.
Maisels MJ, Bhutani VK, Bogen D, Newman TB, Stark AR, Watchko JF. Hyperbilirubinemia in the newborn infant > or =35 weeks’ gestation: an update with clarifications. Pediatrics. 2009;124:1193–8.
Johnson L, Bhutani VK. The clinical syndrome of bilirubin induced neurologic dysfunction. Semin Perinatol. 2011;35:101–13.
Blanchette V, Dror Y, Chan A. Hematology. In: MacDonald MG, Mullett MD, Seschia MMK, editors. Avery’s neonatology: pathophysiology and management of the newborn. Philadelphia: Lippincott, Wiliams and Wilkins; 2005, p. 1169–234.
Nilsen ST, Finne PH, Bergesjo P, Stamnes O. Males with neonatal hyperbilirubinemia examined at 18 years of age. Acta Paediatr Scand. 1984;73:176–80.
Christensen RD, Henry E, Bennett ST, Yaishi HM. Reference interval for reticulcyte parameters of infants during their first 90 days after birth. J Perinatol. 2016;36:61–6.
Schutzman DL, Gatien E, Ajayi S, Wong RJ. Carboxyhemoglobin levels as a predictor of risk for significant hyperbilirubinemia in African American DAT+ infants. J Perinatol. 2016;36:386–8.
Mentzer WC, Glader BE. Erythrocyte disorders in infancy. In: Taeusch HW, Ballard RA, editors. Avery’s diseases of the newborn. 8th ed. Philadelphia: Elsevier Saunders; 2005, p. 1180–214.
Gozzelino R, Jeney V, Soares MP. Mechanisms of cell protection by heme oxygenase-1. Annu Rev Pharm Toxicol. 2010;50:323–54.
Coburn RF, Williams WJ, Kahn SB. Endogenous carbon monoxide production in patients with hemolytic anemia. J Clin Inves. 1966;45:460–8.
Wong RJ, Bhutani VK, Stevenson DK. The importance of hemolysis and its clinical detection in neonates with hyperbilirubinemia. Curr Pediatr Rev. 2017;13:193–8.
Stevenson DK, Vreman HJ. Carbon monoxide and bilirubin production in neonates. Pediatrics. 1997;100:252–9.
American Academy of Pediatrics Subcommittee on Hyperbilirubinemia. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics. 2004;114:297–316.
Bhutani VK, Srinivas S, Castillo Cuadrado ME, Aby JL, Wong RJ, Stevenson DK. Identification of neonatal haemolysis: an approach to predischarge management of neonatal hyperbilirubinemia. Acta Paediatr. 2016;105:e189–94.
Christensen RD, Malleske DT, Lambert DK, Baer VL, Prchal JT, Denson LE, et al. Measuring end tidal carbon monoxide of jaundiced neonates in the birth hospital to identify those with hemolysis. Neonatology. 2016;109:1–5.
Bhutani VK, Maisels MJ, Schutzman DL, Cuadrado MEC, Aby J, Bogen DL, et al. Identification of risk for neonatal hemolysis. Acta Paediatr. 2018;107:1350–6.
Bhutani VK, Johnson L, Sivieri EM. Predictive ability of a predischarge hour-specific serum bilirubin for subsequent significant hyperbilirubinemia in healthy term and near-term newborns. Pediatrics. 1999;103:6–14.
Vreman HJ, Kwong LK, Stevenson DK. Carbon monoxide in blood: an improved microliter blood sample collection system, with rapid analysis by gas chromatography. Clin Chem. 1984;30:1382–6.
Herschel M, Karrison T, Wen M, Calderelli L, Baron B. Evaluation of the direct antiglobulin (Coombs) test for identifying newborns at risk for hemolysis as determined by end-tidal carbon monoxide concentration (ETCOc); and comparison of the Coombs test with ETCOc for detecting significant jaundice. J Perinatol. 2002;22:341–7.
Ramy N, Ghany EA, Alsharany W, Nada A, Darwish RK, Rabie WA, et al. Jaundice phototherapy and DNA damage in full-term neonates. J Perinatol. 2016;36:132–6.
Newman TB, Wu YW, Kuzniewicz MW, Grimes BA, McCulloch CE. Childhood seizures after phototherapy. Pediatrics. 2018;142:32.
Johnson L, Bhutani VK, Karp K, Sivieri EM, Shapiro SM. Clinical report from the pilot USA kernicterus registry (1992 to 2004). J Perinatol. 2009;29:S25–45.
Maisels MJ, Kring E. The contribution of hemolysis to early jaundice in normal newborns. Pediatrics. 2006;118:276–9.
Acknowledgements
The authors would like to acknowledge Andrew Paoletti for his assistance with statistics.
Author information
Authors and Affiliations
Contributions
DLS was responsible for the study concept, design, data interpretation, and preparation of the manuscript. ALE and MT were responsible for the study design, data collection and interpretation, and critical review of the manuscript. AN, AZ, MEP, and KN were responsible for data collection, interpretation, and critical review of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Elsaie, A.L., Taleb, M., Nicosia, A. et al. Comparison of end-tidal carbon monoxide measurements with direct antiglobulin tests in the management of neonatal hyperbilirubinemia. J Perinatol 40, 1513–1517 (2020). https://doi.org/10.1038/s41372-020-0652-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-020-0652-y
This article is cited by
-
Alloimmune hemolytic disease of the fetus and newborn: genetics, structure, and function of the commonly involved erythrocyte antigens
Journal of Perinatology (2023)
-
A “Gold Standard” Test for Diagnosing and Quantifying Hemolysis in Neonates and Infants
Journal of Perinatology (2023)
-
ABO hemolytic disease of the newborn: a need for clarity and consistency in diagnosis
Journal of Perinatology (2023)
-
History and current standard of postnatal management in hemolytic disease of the fetus and newborn
European Journal of Pediatrics (2022)
-
Stannsoporfin with phototherapy to treat hyperbilirubinemia in newborn hemolytic disease
Journal of Perinatology (2022)