Abstract
Objectives
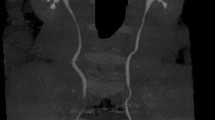
To retrospectively evaluate the efficacy and safety of super-mini percutaneous nephrolithotomy (SMP) and retrograde intrarenal surgery (RIRS) for children with upper urinary tract calculus (1–2 cm).
Patients and methods
Children with upper urinary tract calculus (1–2 cm) who underwent the SMP or RIRS were enrolled in this study. Patients were divided into two groups: group SMP, 36 patients; and group RIRS, 25 patients. Patients were evaluated with KUB radiography or CT after 1 month. The collected data were analyzed.
Results
The mean stone size was 14.18 mm in group SMP, and 14.00 mm in group RIRS (p = 0.812). Group RIRS compared to group SMP showed longer operating time [76.3 vs 53.9 min (p = 0.002)], and postoperative hospital stay [4.2 vs 2.9 days (p = 0.011)]. The overall stone-free rate (SFR) was 94.4% for group SMP, and 60.0% for group RIRS in 1 month after operation (p = 0.001). The re-treatment rate was significantly higher in group RIRS compared to group SMP [20.0% vs 0.0% (p = 0.009)]. The complication rate was 5.6%, and 24.0% for groups SMP, and RIRS, respectively (p = 0.036).
Conclusions
SMP was more effective than RIRS to obtain a better SFR, less re-treatment rate, and complication rate in children with upper urinary tract calculus (1–2 cm).
Similar content being viewed by others
References
Lu P, Wang Z, Song R et al (2015) The clinical efficacy of extracorporeal shock wave lithotripsy in pediatric urolithiasis:a systematic review and meta-analysis. Urolithiasis 43(3):199–206. https://doi.org/10.1007/s00240-015-0757-5
Resorlu B, Kara C, Resorlu EB et al (2011) Effectiveness of ultrasonography in the postoperative follow-up of pediatric patients undergoing ureteroscopic stone manipulation. Pediatr Surg Int 27(12):1337–1341. https://doi.org/10.1007/s00383-011-2979-0
Guven S, Istanbulluoglu O, Gul U et al (2011) Successful percutaneous nephrolithotomy in children:multicenter study on current status of its use, efficacy and complications using Clavien classification. J Urol 185(4):1419–1424. https://doi.org/10.1016/j.juro.2010.11.055
Yuruk E, Tuken M, Gonultas S et al (2017) Retrograde intrarenal surgery in the management of pediatric cystine stones. J Pediatr Urol 13(5):487.e1–487.e5. https://doi.org/10.1016/j.jpurol.2017.01.015
Erkurt B, Caskurlu T, Atis G et al (2014) Treatment of renal stones with flexible ureteroscopy in preschool age children. Urolithiasis 42(3):241–245. https://doi.org/10.1007/s00240-013-0636-x
PalmeroJ L, Durán-Rivera AJ, Miralles J et al (2016) Comparative study for the efficacy and safety of percutaneous nefhrolithotomy (PCNL) and retrograde intrarenal surgery (RIRS) for the treatment of 2–3,5 cm kidney stones. Arch Esp Urol 69(2):67–72
Zhao Z, Tuerxu A, Liu Y et al (2017) Super-mini PCNL (SMP): material, indications, technique, advantages and results. Arch Esp Urol 70(1):211–216
Al Busaidy SS, Kurukkal SN, Al Hooti QM et al (2016) Is RIRS emerging as the preferred option for the management of 2–4 cm renal stones: our experience. Can J Urol 23(4):8364–8367
Liu Y, Wu W, Tuerxun A et al (2016) Super-mini percutaneous nephrolithotomy in the treatment of pediatric nephrolithiasis: evaluation of the initial results. J Endourol 31(S1):S38–S42. https://doi.org/10.1089/end.2016.0572
Pelit ES, Atis G, Kati B et al (2017) Comparison of mini-percutaneous nephrolithotomy and retrograde intrarenal surgery in preschool-aged children. Urology 101:21–25. https://doi.org/10.1016/j.urology.2016.10.039
Baş O, Dede O, Aydogmus Y et al (2016) Comparison of retrograde intrarenal surgery and micro-percutaneous nephrolithotomy in moderately sized pediatric kidney stones. J Endourol 30(7):765–770. https://doi.org/10.1089/end.2016.0043
Zeng G, Wan S, Zhao Z et al (2016) Super-mini percutaneous nephrolithotomy (SMP): a new concept in technique and instrumentation. BJU Int 117(4):655–661. https://doi.org/10.1111/bju.13242
Liu Y, Wu W, Tuerxun A et al (2017) Super-mini percutaneous nephrolithotomy in the treatment of pediatric nephrolithiasis: evaluation of the initial results. J Endourol 31(S1):S38–S42. https://doi.org/10.1089/end.2016.0572
Opondo D, Gravas S, Joyce A et al (2014) Standardization of patient outcomes reporting in percutaneous nephrolithotomy. J Endourol 28(7):767–774. https://doi.org/10.1089/end.2014.0057
Bozzini G, Verze P, Arcaniolo D et al (2017) A prospective randomized comparison among SWL, PCNL and RIRS for lower calyceal stones less than 2 cm:a multicenter experience: a better understanding on the treatment options for lower pole stones. World J Urol 35(4):1967–1975. https://doi.org/10.1016/j.juro.2016.02.1377
Liu Y, Yasheng A, Chen K et al (2016) Difference in urinary stone composition between Uyghur and Han children with urolithiasis. Urolithiasis 45(5):435–440. https://doi.org/10.1007/s00240-016-0931-4
Lipkin ME, Preminger GM (2012) Risk reduction strategy for radiation exposure during percutaneous nephrolithotomy. Curr Opin Urol 22(2):139–143. https://doi.org/10.1097/MOU.0b013e32834fc36a
Wang HH, Wiener JS, Lipkin ME et al (2015) Estimating the nationwide, hospital based economic impact of pediatric urolithiasis. J Urol 193(5 Suppl):1855–1859. https://doi.org/10.1016/j.juro.2014.09.116
Simayi A, Liu Y, Yiming M et al (2019) Clinical application of super-mini PCNL (SMP) in the treatment of upper urinary tract stones under ultrasound guidance. World J Urol 37(5):943–950. https://doi.org/10.1007/s00345-018-2465-6
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
JL, BW: project development. BL, PZ, WD, XL, CP: data collection or management. YN, SW: data analysis. HJ: manuscript writing. AY manuscript editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were obtained from the institutional Ethics committee of People’s Hospital of Xinjiang Uygur Autonomous Region, Xinjiang, China.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Jia, H., Li, J., Liu, B. et al. Comparison of super-mini-PCNL and flexible ureteroscopy for the management of upper urinary tract calculus (1–2 cm) in children. World J Urol 39, 195–200 (2021). https://doi.org/10.1007/s00345-020-03150-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-020-03150-x