Abstract
Introduction
The advent of peroral endoscopic myotomy (POEM) shed some light on the role of the current standards in the treatment of idiopathic achalasia, namely endoscopic pneumatic dilatation (PD) and laparoscopic Heller myotomy (LHM). We analyzed the quality of the current evidence comparing LHM and PD.
Methods
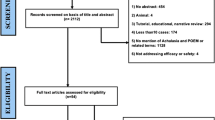
A systematic literature search was performed in Pubmed/Medline, Web of Science, Google Scholar and Cochrane for meta-analyses/systematic reviews comparing PD and LHM or open surgery, limited to English language full-text articles. After a detailed review of these meta-analyses, all studies included were analyzed further in depth with respect to treatment protocol, assessment of success, complications and sequelae such as gastroesophageal reflux (GER), as well as follow-up details.
Results
Six randomized controlled trials (RCT), 5 with LHM and 1 with open surgery, were found, published in 10 papers. In contrast to a rather homogeneous LHM technique, PD regimens as well as the clinical dysphagia scores were different in every RCT; most RCTs also showed methodological limitations. There were nine meta-analyses which included a variable number of these RCTs or other cohort studies. Meta-analyses between 2009 and 2013 favored surgery, while the 4 most recent ones reached divergent conclusions. The main difference might have been whether repeated dilatation was regarded as part of the PD protocol or as failure.
Conclusions
The variability in PD techniques and in definition of clinical success utilized in the achalasia RCTs on PD versus LHM render the conclusions of meta-analyses unreliable. Further randomized studies should be based on uniform criteria; in the meantime, publication of even more meta-analyses should be avoided.

Similar content being viewed by others
References
Markar SR, Mackenzie H, Askari A et al (2018) Population-based cohort study of surgical myotomy and pneumatic dilatation as primary interventions for oesophageal achalasia. Br J Surg 105:1028–1035
Boeckxstaens GE, Annese V, des Varannes SB, et al. Pneumatic dilation versus laparoscopic Heller's myotomy for idiopathic achalasia. N Engl J Med 2011;364:1807–16.
Moonen A, Annese V, Belmans A et al (2016) Long-term results of the European achalasia trial: a multicentre randomised controlled trial comparing pneumatic dilation versus laparoscopic Heller myotomy. Gut 65:732–739
Bonifacio P, de Moura DTH, Bernardo WM, et al. Pneumatic dilation versus laparoscopic heller's myotomy in the treatment of achalasia: systematic review and meta-analysis based on randomized controlled trials. Dis Esophagus 2019;32–34.
Baniya R, Upadhaya S, Khan J et al (2017) Laparoscopic esophageal myotomy versus pneumatic dilation in the treatment of idiopathic achalasia: a meta-analysis of randomized controlled trials. Clin Exp Gastroenterol 10:241–248
Illes A, Farkas N, Hegyi P et al 2017 Is Heller myotomy better than balloon dilation? A meta-analysis. J Gastrointestin Liver Dis 26:121–127
Cheng JW, Li Y, Xing WQ et al (2017) Laparoscopic Heller myotomy is not superior to pneumatic dilation in the management of primary achalasia: Conclusions of a systematic review and meta-analysis of randomized controlled trials. Medicine (Baltimore) 96:e5525
Yaghoobi M, Mayrand S, Martel M et al (2013) Laparoscopic Heller's myotomy versus pneumatic dilation in the treatment of idiopathic achalasia: a meta-analysis of randomized, controlled trials. Gastrointest Endosc 78:468–475
Schoenberg MB, Marx S, Kersten JF et al (2013) Laparoscopic Heller myotomy versus endoscopic balloon dilatation for the treatment of achalasia: a network meta-analysis. Ann Surg 258:943–952
Weber CE, Davis CS, Kramer HJ et al (2012) Medium and long-term outcomes after pneumatic dilation or laparoscopic Heller myotomy for achalasia: a meta-analysis. Surg Laparosc Endosc Percutan Tech 22:289–296
Wang L, Li YM, Li L (2009) Meta-analysis of randomized and controlled treatment trials for achalasia. Dig Dis Sci 54:2303–2311
Campos GM, Vittinghoff E, Rabl C et al (2009) Endoscopic and surgical treatments for achalasia: a systematic review and meta-analysis. Ann Surg 249:45–57
Chrystoja CC, Darling GE, Diamant NE et al (2016) Achalasia-specific quality of life after pneumatic dilation or laparoscopic heller myotomy with partial fundoplication: a multicenter randomized clinical trial. Am J Gastroenterol 111:1536–1545
Felix VN, Cecconello I, Zilberstein B et al (1998) Achalasia: a prospective study comparing the results of dilatation and myotomy. Hepatogastroenterology 45:97–108
Csendes A, Velasco N, Braghetto I et al (1981) A prospective randomized study comparing forceful dilatation and esophagomyotomy in patients with achalasia of the esophagus. Gastroenterology 80:789–795
Csendes A, Braghetto I, Henriquez A et al (1989) Late results of a prospective randomised study comparing forceful dilatation and oesophagomyotomy in patients with achalasia. Gut 30:299–304
Kostic S, Kjellin A, Ruth M et al (2007) Pneumatic dilatation or laparoscopic cardiomyotomy in the management of newly diagnosed idiopathic achalasia, results of a randomized controlled trial. World J Surg 31:470–478
Persson J, Johnsson E, Kostic S et al (2015) Treatment of achalasia with laparoscopic myotomy or pneumatic dilatation: long-term results of a prospective, randomized study. World J Surg 39:713–720
Borges AA, Lemme EM, Abrahao LJ Jr et al (2014) Pneumatic dilation versus laparoscopic Heller myotomy for the treatment of achalasia: variables related to a good response. Dis Esophagus 27:18–23
Novais PA, Lemme EM (2010) 24-h pH monitoring patterns and clinical response after achalasia treatment with pneumatic dilation or laparoscopic Heller myotomy. Aliment Pharmacol Ther 32:1257–1265
Hamdy E, El Nakeeb A, El Hanfy E et al (2015) Comparative study between laparoscopic heller myotomy versus pneumatic dilatation for treatment of early achalasia: a prospective randomized study. J Laparoendosc Adv Surg Tech A 25:460–464
Kummerow Broman K, Phillips SE, Faqih A et al (2018) Heller myotomy versus Heller myotomy with Dor fundoplication for achalasia: long-term symptomatic follow-up of a prospective randomized controlled trial. Surg Endosc 32:1668–1674
Wang HM, Tai WC, Chuah SK et al (2015) Comparison of treatment outcomes of endoscope-guided pneumatic dilation and laparoscopic Heller myotomy. Kaohsiung J Med Sci 31:639–643
Tabola R, Grabowski K, Lewandowski A et al (2013) Achalasia–balloon dilation or surgery? Med Sci Monit 19:1089–1094
Suarez J, Mearin F, Boque R et al (2002) Laparoscopic myotomy vs endoscopic dilation in the treatment of achalasia. Surg Endosc 16:75–77
Gockel I, Junginger T, Bernhard G et al (2004) Heller myotomy for failed pneumatic dilation in achalasia: how effective is it? Ann Surg 239:371–377
Rodriguez E de Santiago, Mohammed N, Manolakis A et al (2019) Anterior versus posterior myotomy during poem for the treatment of achalasia: systematic review and meta-analysis of randomized clinical trials. J Gastrointestin Liver Dis 28:107–115
Li H, Peng W, Huang S et al (2019) The 2 years' long-term efficacy and safety of peroral endoscopic myotomy for the treatment of achalasia: a systematic review. J Cardiothorac Surg 14:1
Lee Y, Brar K, Doumouras AG et al (2019) Peroral endoscopic myotomy (POEM) for the treatment of pediatric achalasia: a systematic review and meta-analysis. Surg Endosc 33:1710–1720
Evensen H, Kristensen V, Larssen L et al (2019) Outcome of peroral endoscopic myotomy (POEM) in treatment-naive patients A systematic review. Scand J Gastroenterol 54:1–7
Chandan S, Mohan BP, Chandan OC et al (2019) Clinical efficacy of per-oral endoscopic myotomy (POEM) for spastic esophageal disorders: a systematic review and meta-analysis. Surg Endosc 34:707–718
Schlottmann F, Luckett DJ, Fine J et al (2018) Laparoscopic Heller Myotomy Versus Peroral Endoscopic Myotomy (POEM) for Achalasia: A Systematic Review and Meta-analysis. Ann Surg 267:451–460
Repici A, Fuccio L, Maselli R et al (2018) GERD after per-oral endoscopic myotomy as compared with Heller's myotomy with fundoplication: a systematic review with meta-analysis. Gastrointest Endosc 87(934–943):e18
Fernandez-Ananin S, Fernandez AF, Balague C et al (2018) What to do when Heller's myotomy fails? Pneumatic dilatation, laparoscopic remyotomy or peroral endoscopic myotomy: a systematic review. J Minim Access Surg 14:177–184
Khan MA, Kumbhari V, Ngamruengphong S et al (2017) Is POEM the answer for management of spastic esophageal disorders? A systematic review and meta-analysis. Dig Dis Sci 62:35–44
Crespin OM, Liu LWC, Parmar A et al (2017) Safety and efficacy of POEM for treatment of achalasia: a systematic review of the literature. Surg Endosc 31:2187–2201
Awaiz A, Yunus RM, Khan S et al (2017) Systematic review and meta-analysis of perioperative outcomes of peroral endoscopic myotomy (POEM) and laparoscopic heller myotomy (LHM) for achalasia. Surg Laparosc Endosc Percutan Tech 27:123–131
Zhang Y, Wang H, Chen X et al (2016) Per-oral endoscopic myotomy versus laparoscopic heller myotomy for achalasia: a meta-analysis of nonrandomized comparative studies. Medicine (Baltimore) 95:e2736
Patel K, Abbassi-Ghadi N, Markar S et al (2016) Peroral endoscopic myotomy for the treatment of esophageal achalasia: systematic review and pooled analysis. Dis Esophagus 29:807–819
Marano L, Pallabazzer G, Solito B et al (2016) Surgery or peroral Esophageal myotomy for achalasia: a systematic review and meta-analysis. Medicine (Baltimore) 95:e3001
Akintoye E, Kumar N, Obaitan I et al (2016) Peroral endoscopic myotomy: a meta-analysis. Endoscopy 48:1059–1068
Wei M, Yang T, Yang X et al (2015) Peroral esophageal myotomy versus laparoscopic Heller's myotomy for achalasia: a meta-analysis. J Laparoendosc Adv Surg Tech A 25:123–129
Talukdar R, Inoue H, Nageshwar RD (2015) Efficacy of peroral endoscopic myotomy (POEM) in the treatment of achalasia: a systematic review and meta-analysis. Surg Endosc 29:3030–3046
Minami H, Inoue H, Haji A et al (2015) Per-oral endoscopic myotomy: emerging indications and evolving techniques. Dig Endosc 27:175–181
Barbieri LA, Hassan C, Rosati R et al (2015) Systematic review and meta-analysis: efficacy and safety of POEM for achalasia. United European Gastroenterol J 3:325–334
Ponds FA, Fockens P, Lei A et al (2019) Effect of peroral endoscopic myotomy vs pneumatic dilation on symptom severity and treatment outcomes among treatment-naive patients with achalasia: a randomized clinical trial. JAMA 322:134–144
Werner YB, Hakanson B, Martinek J et al (2019) Endoscopic or surgical myotomy in patients with idiopathic achalasia. N Engl J Med 381:2219–2229
Vaezi MF, Pandolfino JE, Vela MF (2013) ACG clinical guideline: diagnosis and management of achalasia. Am J Gastroenterol 108:1238–1249; quiz 1250
Leyden JE, Moss AC, MacMathuna P. Endoscopic pneumatic dilation versus botulinum toxin injection in the management of primary achalasia. Cochrane Database Syst Rev 2014:Cd005046.
Zaninotto G, Bennett C, Boeckxstaens G, et al. The 2018 ISDE achalasia guidelines. Dis Esophagus 2018.
Inoue H, Shiwaku H, Iwakiri K et al (2018) Clinical practice guidelines for peroral endoscopic myotomy. Dig Endosc 30:563–579
Sami SS, Haboubi HN, Ang Y et al (2018) UK guidelines on oesophageal dilatation in clinical practice. Gut 67:1000–1023
Sawas T, Ravi K, Geno DM et al (2017) The course of achalasia one to four decades after initial treatment. Aliment Pharmacol Ther 45:553–560
Huelsen A, Oumer R, Ashcroft A et al (2016) Achalasia: a 13-year, single-centre experience comparing endoscopic balloon dilatation and laparoscopic Heller myotomy. N Z Med J 129:41–50
Ehlers AP, Oelschlager BK, Pellegrini CA et al (2017) Achalasia treatment, outcomes, utilization, and costs: a population-based study from the United States. J Am Coll Surg 225:380–386
Vanuytsel T, Lerut T, Coosemans W et al (2012) Conservative management of esophageal perforations during pneumatic dilation for idiopathic esophageal achalasia. Clin Gastroenterol Hepatol 10:142–149
Rosch T, Repici A, Boeckxstaens G (2017) Will Reflux Kill POEM? Endoscopy 49:625–628
Author information
Authors and Affiliations
Contributions
The study idea was developed by TR in discussion with JdH and GB. Paper search was done by MD, JdH and TR; data analysis by JdH and TR. All co-authors gave their input by reading, commenting and improving the manuscript written by JdH and TR, e.g., adding Fig. 1 (MD, PS, TR). All authors have seen and approved the manuscript.
Corresponding author
Ethics declarations
Disclosure
None of the authors has anything to disclose with regards to the contents of this paper which does not include any commercial products. In detail, Dr. Jocelyn de Heer, Dr. Madhav Desai, Dr. Guy Boeckxstaens, Dr. Giovanni Zaninotto, Dr. Karl-Hermann Fuchs, Dr. Prateek Sharma, Dr. Guido Schachschal, Dr. Oliver Mann, Dr. Thomas Rösch, and Dr. Yuki Werner have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
de Heer, J., Desai, M., Boeckxstaens, G. et al. Pneumatic balloon dilatation versus laparoscopic Heller myotomy for achalasia: a failed attempt at meta-analysis. Surg Endosc 35, 602–611 (2021). https://doi.org/10.1007/s00464-020-07421-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07421-x