Abstract
Extra-intestinal manifestations (EIMs) of the eyes are found in IBD patients, but the underlying pathogenesis remains unknown. To investigate the pathogenesis of IBD-associated retinal dysfunction, chronic colitis was induced in mice by oral administration of dextran sodium sulfate (DSS). Electroretinography (ERG) was performed to evaluate retinal function. Retinal neuron degeneration was analyzed by immunohistochemistry. Colitic mice displayed aberrant amplitudes of ERG a-, b-wave and oscillatory potentials (OP). Importantly, we observed severe degeneration of bipolar and ganglion cells. In contrast, outer retinal neurons (mainly photoreceptor cells) are mildly affected by colitis. Moreover, retinal inflammatory responses were significantly upregulated during colitis, including microglia activation, lymphocyte infiltration and cytokine/chemokine production. Notably, mucosal addressin cell adhesion molecule 1 (MAdCAM-1) was upregulated in retinal microvessels, especially the superficial and deep plexuses, and recruited gut-homing CD4+ T cells to be co-localized with bipolar and ganglion cells during colitis. Expectedly, in vivo depletion of CD4+ T cells or blockade of MAdCAM-1 greatly alleviated colitis-induced retinal inflammatory responses and neuron degeneration. Therefore, our data provide novel insight into the pathogenesis of IBD-associated retinal dysfunction, and targeted immune therapy directly against MAdCAM-1 might provide a novel approach in the management of eye EIM of IBD.
Similar content being viewed by others
Introduction
Crohn’s disease (CD) and ulcerative colitis (UC) are the two major subtypes of inflammatory bowel disease (IBD), known as a chronic, relapse and inflammatory disorder of the gastrointestinal tract. Emerging evidences have demonstrated that IBD frequently leads to extra-intestinal injury, and over a half of IBD patient present extra-intestinal manifestations (EIMs), including the liver, joints, the skin, and the eyes.1,2 Although several recent studies have suggested that the immune responses involved in EIMs can be extended or translocated from the gut, or independent of but perpetuated by IBD,1 the exact pathogenesis remains to be elusive.
A number of studies have implicated that intestinal mucosal immunity plays a crucial role in the pathogenesis of inflammatory injury at extra-intestinal sites in IBD. For example, primary sclerosing cholangitis (PSC) is a long-term progressive fibroinflammatory liver/gallbladder disease, which has been known as an extra-intestinal disorder and potently indicated to be associated with intestinal mucosal immune responses. T lymphocytes isolated from PSC liver show a “gut-homing” phenotype, characterized by aberrant expression of CCR9 and α4β7, both of which known as markers of “gut-homing T cells”.3 Meanwhile, mucosal addressin cell adhesion molecule 1 (MAdCAM-1), which binds to α4β7 in T cells and constitutively expressed on mucosal vessels,4 is significantly upregulated on hepatic endothelium in PSC, as well as the gut-specific chemokine CCL25, which interacts with CCR9.5 Uveitis is one of the common eye EIMs, which has been well-documented as a T-cell-mediated autoimmune disease, and autoreactive T cells, especially Th17 lineage, play an essential part in the pathogenesis. Recently, it was revealed that signals derived from gut microbiota could activate T cells specific for interphotoreceptor retinoid binding protein (IRBP, a retinal autoantigen) and these T cells contributed to triggering experimental autoimmune uveitis (EAU).6 These findings prompt us to reason that T cells originally activated in the gut might be the essential player in the development of extra-intestinal complications of IBD.
Conventionally, central nervous system (CNS) and retina (actually brain tissue and the only part of the CNS that can be visualized non-invasively) are known as “immune-privileged” sites.7,8 However, great progresses have been made to understand the function of immune cells in the pathogenesis of CNS and retina diseases. Multiple sclerosis (MS) and its animal model, experimental autoimmune encephalomyelitis (EAE), are considered as myelin oligodendrocyte glycoprotein (MOG)-specific T-cell-driven CNS inflammation, and infiltration of IL-17A-secreting T cells was found in the CNS during EAE.9 Glaucoma, a common neurodegenerative disease, usually arises from elevated intraocular pressure (IOP), but a recent study has shown that IOP could not induce glaucomatous neurodegeneration in the absence of CD4+ T cells or intestinal microbiota, strongly suggesting that T cells (especially those pre-sensitized by gut microbiota) might be involved in retinal neurodegenerative diseases.10 These studies unveil an unappreciated role of T cells in retina diseases and the mechanisms whereby they regulate the induction and development of retinopathy are mostly unknown.
To varying degrees, retina dysfunction has been observed in patients with IBD and experimental colitic mice. Mice with dextran sodium sulfate (DSS)-induced colitis displayed abnormal electroretinography (ERG).11 Posterior segment signs were reported in IBD subjects, including retinal pigment epithelium disturbance, serous retinal detachment, and central retinal vein occlusion.12,13 Notably, a theory underlying the ocular involvement in IBD proposed by Das14 suggested that there might be autoantigens shared by the gut and eyes, and immunopathogenetic autoantibodies against these antigens might contribute to the injury in extra-intestinal sites. However, whether neuroretina injury exists in IBD patients and the exquisite immunological pathogenesis of retinal complications remains largely unclear.
Here, we found experimental colitis resulted in severe damage of inner retinal neurons (bipolar and ganglion cells), providing an explanation of the abnormal ERG detected in mice with experimental colitis. Importantly, we found significantly increased infiltration of α4β7-expressing CD4+ T cells into the retina during colitis, which were co-localized with inner retinal neurons. In addition, we revealed that MAdCAM-1 was aberrantly expressed on retinal microvascular endothelial cells, and intravitreal injection of anti-MAdCAM-1 antibody in mice remarkably alleviated colitis-induced degeneration of inner retinal neurons. To our knowledge, this is the first study revealing intestinal inflammation leads to loss of inner retinal neurons, which was at least partly depending on MAdCAM-1-mediated gut-homing CD4+ T-cell recruitment. These data suggest that targeted immune therapy directed against MAdCAM-1 might provide a novel approach in the management of eye EIM of IBD.
Results
Retinal function is impaired in mice with DSS-induced colitis
Previous studies have demonstrated that retinal function was impaired in mouse with experimental colitis, which was measured by ERG, known as the most effective and common way to assess retinal function.11,15 To further explore the aberration of retina structure and function, we established chronic colitis induced by DSS in mice (Fig. 1a, Supplementary Fig. 2), and analyzed the alteration of ERG waves. A mild decrease of ERG a-wave amplitudes was observed in DSS-treated mice only at the flash intensities of 2 and 50 cd•s/m2 (Fig. 1b, c, Supplementary Fig. 3a, b). Notably, delayed implicit times of a-wave only occurred at 50 cd•s/m2 (Supplementary Fig. 3c). In addition, colitis led to significantly decreased ERG b-wave amplitudes (Fig. 1b, c, Supplementary Fig. 3d, e) and oscillatory potentials (OP) amplitudes (Fig. 1d, e) in DSS-treated mice at all indicated flash intensities. We also observed delayed b-wave implicit times at all indicated flash intensities, except for 0.002 cd•s/m2 (Supplementary Fig. 3f). These data imply that retinal inner neurons might suffer from severe degeneration. Moreover, we found that the thickness of outer nuclear layer (ONL) was not changed, but an apparently thinner inner nuclear layer (INL) was seen in the retina of DSS-treated mice than control mice (Fig. 1f, g, Supplementary Fig. 4), in concert with changes of ERG described above, supporting our speculations that inner retinal neurons might be badly damaged.
a Experimental colitis was induced in male C57BL/6J mice (8–10 weeks old) as indicated in Methods. b Electroretinography (ERG) was measured in DSS-treated and untreated control mice under scotopic conditions at indicated flash intensities (n = 5 mice in each group), and c represented by histogram, as well as d, e oscillatory potentials (OP). f Retina sections from control and DSS-treated mice were analyzed by hematoxylin-eosin (HE) staining (5 retinas collected from different mice in each group). Original magnification, ×20 (upper panel); ×200 (lower panel). g Thickness of retinal outer nuclear layer (ONL, left panel) and inner nuclear layer (INL, right panel) from control and DSS-treated mice were evaluated. *p < 0.05; **p < 0.01 compared with the control groups. Statistical comparisons between groups were performed using paired Student’s t test (two-tailed). The data are represented as means ± SEM. Representative results from one of three independent experiments are shown. RPE retinal pigment epithelium, OS outer segment, IS inner segment, ONL outer nuclear layer, OPL outer plexiform layer, INL inner nuclear layer, IPL inner plexiform layer, GCL retinal ganglion cell layer.
Colitis leads to severe degeneration of inner retinal neurons
As a part of the CNS, the retina has an integrate nerve conduction structure. BPC, the most important interneuron, transmit signals from photoreceptor cells (rods and cones) to amacrine and ganglion cells in the inner retina. The degeneration of inner retinal neurons, including BPC, might be mirrored by the alteration of ERG b-wave. As presented in Supplementary Fig. 4, we found that significantly thinner INL in the center and the periphery of the retina, where BPC were located, in DSS-treated mice. Of note, we performed immunofluorescent staining for protein kinase C alpha (PKCα), a marker for BPC, and observed a decrease in BPC number and their dendritic fibers became shorter, looser, and more irregular in colitic mice than controls, indicative of loss and dysfunction of BPC during colitis (Fig. 2a). Since BPC are responsible for transmitting signals from photoreceptor cells to retinal ganglion cells (RGC),16,17 synaptic connections between BPC and RGC or photoreceptor cells were analyzed. In DSS-treated mice, synaptic connections between BPC and RGC (Fig. 2b) or photoreceptor cells (Fig. 2c) were markedly compromised. As the output element of retina, RGC form the optic nerve, firing and transmitting the visual nerve impulse to the brain, and their degeneration result in impairment of vision. We performed staining for β III tubulin to quantify RGC and axon loss during colitis and observed significant apoptosis and loss of RGC compared with controls (Fig. 2d). Moreover, DSS-treated mice exhibited remarkably upregulated expression of Nestin (Fig. 2e), a marker of neural stem cells, indicative of the degeneration of RGC.18 Since optic nerve was derived from RGC nerve fibers, we explore whether intestinal inflammation affected the demyelination. As expected, DSS insults resulted in reduced myelin basic protein 1 (MBP-1) expression in both RGC (Fig. 2f) and the optic nerve (Fig. 2g), suggesting that colitis could aggravate the demyelination.
Colitis was induced in male C57BL/6J mice (8–10 weeks old) as indicated, and retinas were collected for immunofluorescent analysis. a Bipolar cells (BPC) were analyzed by immunofluorescent staining for PKCα (left panel), and the number of BPC and their axons was presented in histogram (right panel). b The connection between BPC and retinal ganglion cells (RGC) was analyzed by co-staining for PKCα and β III tubulin (left panel), and abnormal BPC-RGC synaptic connection was calculated in histogram (right panel). c PSD95, a typical marker of photoreceptor cell (PRC) synapses, together with PKCα was used to identify the connection between PRC and BPC (left panel) and abnormal BPC-PRC synaptic connection was calculated in histogram (right panel). d The apoptosis of RGC was analyzed by immunofluorescent staining for TdT-mediated dUTP nick-end labeling (TUNEL) (left panel), and the apoptotic RGC and the average axonal length of RGC was calculated in histogram (right panel). e RGC stemness was detected by immunofluorescent staining for Nestin. The demyelination was analyzed using anti-MBP-1 (myelin basic protein 1) in the f retina and g optic nerve. Five retinas from different mice in each group were collected for analysis. **p < 0.01; ***p < 0.001 compared with control groups. Statistical comparisons between groups were performed using paired Student’s t test (two-tailed). The data are represented as means ± SEM. Representative results from one of three independent experiments are shown.
To confirm that experimental colitis indeed induced inner retinal neuron degeneration, we employed IL-10−/− mice, which develop spontaneous enterocolitis 6–8 weeks after birth (Supplementary Fig. 5a), thus being well-known as a mouse model of human IBD.19 Similarly, IL-10−/− mice suffered from severe degeneration of inner retinal neurons at the age of 12 weeks (Supplementary Fig. 5b, c). To exclude the possibility that IL-10 deficiency directly affected retinal neurons, retinas were collected from 4 to 6-week-old IL-10−/− mice, which did not not or only develop mild intestinal inflammation, and we did not observe detectable degeneration of inner retinal neurons (data not shown). Collectively, these data suggest that experimental colitis induces nonnegligible inner retinal neuron degeneration characterized by abnormal morphology, loss of RGC and BPC, and disrupted connection of neuron fibers.
Outer retinal neurons are mildly affected during colitis
Since we found slightly aberrant ERG a-waves in DSS-treated mice, we next sought to investigate whether outer retinal neurons also affected by colitis. Given a-waves were mainly derived from photoreceptor cells, we examined the architecture and apoptosis of photoreceptors, both of which were not significantly altered (Fig. 3a, b). However, abnormal photoreceptor cell sproutings were found (Fig. 3c), which were supposed to connect with BPC. We also found that DSS retinas displayed markedly upregulated expression of Rhodopsin in the outer segment (OS), whose accumulation was reported to accelerate photoreceptor cell degeneration,20 and an increase in the thickness of OS than controls (Fig. 3h). The photoreceptor inner segment (IS) did not display significant changes (Fig. 3e). Taken together, photoreceptors were slightly affected by colitis, which was different from the significant neurodegeneration of RGC.
Colitis was induced in male C57BL/6J mice (8–10 weeks old) as indicated, and retinas were collected for immunofluorescent analysis. a, b DSS-treated mice did not show significant alteration of the architecture and apoptosis of photoreceptor cells (PRC). c PRC sprouts were shown using anti-PSD95. d Retinal outer segment (OS) and e inner segment (IS) were identified using anti-Rho (Rhodopsin) and anti-NaK (Na+/K+-ATPase), respectively. The average thickness of d OS (Rho+ cell layer) and e IS (NaK+ cell layer) was shown in bar charts. Five retinas from different mice in each group were collected for analysis. *p < 0.05; ***p < 0.001 compared with controls. Statistical comparisons between groups were performed using paired Student’s t test (two-tailed). The data are represented as means ± SEM. Representative results from one of three independent experiments are shown. ONL outer nuclear layer.
Experimental colitis alters retinal microglia/macrophage proliferation and activation
It has been well-documented that microglia activation is intimately associated with retinal inflammation and degeneration. We next investigate whether microglia activation in the retina were affected by colitis. Circulating macrophages infiltrating into the retina are commonly identified as CD45high CD11b+ and retinal microglia as CD45mid CD11b+.21,22 We first performed flow cytometric staining for CD11b and CD45 to analyze retinal microglia and found a significant increase in the number of microglia (Fig. 4a). In addition, immunofluorescence staining for ionized calcium binding adapter molecule 1 (Iba1) and found remarkable increased infiltration of Iba1+ microglia/macrophages (Fig. 4b), and a greater abundance of retinal transmembrane protein 119 (Tmem119, a lineage marker distinguishing microglia from peripheral macrophages) positive microglia were observed in in DSS retinas (Fig. 4c).23 We also found increased Nestin expression in Iba1+ cells in DSS retinas (Fig. 4d), indicative of upregulated proliferation of retinal microglia/macrophages during colitis. These data suggest that colitis promotes the proliferation of retinal microglia/macrophages. Since microglia act as neuropathological sensors and the first line of defense to degeneration in the retina and CNS, dysregulation of their activation could compromise the neural homeostasis and result in neural tissue damage. Therefore, we investigated whether DSS-induced colitis affected microglia activation. Flow cytometry showed increased expression of microglia-derived CD86,22 a marker of microglia/macrophage activation in DSS retinas than controls (Fig. 4e). Immunofluorescent staining showed Iba1+ ameboid cells exhibited shorter processes in colitic mice, compared with the resting ramified microglia in control mice (Fig. 4f). Moreover, upregulated expression level of MHC II was detected in Iba1+ cells (Fig. 4g), further verifying that colitis could enhance retinal microglia/macrophage activation. Consistently, IL-10−/− mice displayed increase number of retinal microglia/macrophages, exhibiting an “ameboid” status and shorter processes, compared with the resting ramified microglia/macrophages in control mice (Supplementary Fig. 5d).
Colitis was induced in male C57BL/6J mice (8–10 weeks old) as indicated, and retinas were collected for further analysis. a Flow cytometric staining for CD45 and CD11b was performed to identify microglia (CD45mid CD11b+) and macrophages (CD45hi CD11b+) in DSS and control retinas, and their frequencies were represented by histogram. Immunofluorescent staining for b ionized calcium binding adapter molecule 1 (Iba1) and c Transmembrane protein 119 (Tmem119) was performed to identify microglia/macrophages or microglia, respectively. The absolute cell number was shown in histogram. d Immunofluorescent co-staining for Nestin and Iba1 was used to indicate proliferative microglia/macrophages in the retina. e Mean fluorescence intensity (MFI) of CD86 in retinal CD45mid CD11b+ microglia showing a significant increase in DSS mice compared with controls. f Mice with DSS showed increased morphologic changes of microglia/macrophages from ramified cells to ameboid cells than control mice. Higher-magnification images were displayed in the right panel. g MHC II was used as a maker of microglia/macrophage activation and mice with DSS showed increased expression of MHC II than controls. Sixteen retinas from each group were collected for flow cytometric analysis (a, e). Five retinas from different mice in each group were collected for immunofluorescent analysis (b–d, f, g). *p < 0.05; ***p < 0.001. Statistical comparisons between groups were performed using paired Student’s t test (two-tailed). The data are represented as means ± SEM. Representative results from one of three independent experiments were shown.
CD4+ T cells were recruited into the retina during colitis
Based on findings above, we questioned how intestinal inflammation regulated retinal damage “in distance”. Given CD4+ T cells play an essential role in regulating IBD, we asked whether colitis-associated retina damage was mediated by T cells. Interestingly, we found significantly increased infiltration of CD4+ T cells in DSS retinas than controls (Fig. 5a). Furthermore, we found that CD4+ T cells were mainly localized in the OPL and co-localization of CD4+ T cells and BPC was observed in DSS retinas (Fig. 5b). Importantly, we did not observe any leakage of retinal vessels during colitis (Supplementary Fig. 6), suggesting that T-cell infiltration did not result from vascular rupture. In addition, we found a significant increase of pro-inflammatory cytokine expression, including TNF-α, IL-1β, and IFN-γ (Supplementary Fig. 7a), which were reported to be closely involved in the CD4+ T-cell differentiation and development of DSS-induced colitis.24 Next, we aimed to confirm the pathogenic role of CD4+ T cells in the retina during colitis. We depleted CD4+ T cells in mice by intraperitoneal injection of anti-CD4 antibody, which remarkably reduced the number of systemic CD4+ T cells (Fig. 5c). As expected, ERG showed significantly less impairment of retinal functions (Fig. 5d), and immunofluorescent staining showed anti-CD4 treatment markedly relieved colitis-associated retinal inner neuron degeneration (Fig. 5e). In addition, flow cytometry demonstrated reduced retinal CD4+ T-cell infiltration (Fig. 5f) and microglia activation (Fig. 5g, h) in DSS mice with CD4+ T-cell depletion than those with isotype controls.
a, b Colitis was induced in male C57BL/6J mice (8–10 weeks old) as indicated. a CD4+ T-cell infiltration in the retina during DSS-induced colitis was determined by flow cytometry. b The location of CD4+ T cells was analyzed by immunofluorescent staining and arrows indicated their contact with BPC (PKCα+) in the retina. c–h CD4+ T-cell depletion and colitis induction was performed in male C57BL/6J mice (8–10 weeks old) as indicated. c Anti-CD4 antibody potently decreased the number of splenic CD4+ T cells during colitis (n = 10 mice), and d improved retinal function measured by ERG (n = 10 mice). e BPC and RGC loss was analyzed by immunofluorescent staining for PKCα and β III tubulin, respectively, and calculated in histogram. f Retinal CD4+ T-cell and g microglia infiltration was analyzed by flow cytometry. h CD45mid CD11b+ microglia activation was examined by flow cytometric staining for CD86. Sixteen retinas from each group were collected for flow cytometric analysis (a–h). Five retinas from different mice in each group were collected for immunofluorescent analysis (b–e). *p < 0.05; **p < 0.01, ***p < 0.001. Statistical comparisons between groups were performed using paired Student’s t test (two-tailed) (a) or one-way ANOVA followed by Tukey’s multiple comparisons test (c–h). The data are represented as means ± SEM. Representative results from one of three independent experiments are shown.
A great body of evidence have demonstrated an essential role of chemokines in guiding leukocyte/lymphocyte migration and inducing IBD.25,26 We next analyzed retinal chemokine expression in colitic mice, and found that the expression levels of CXCL9, CXCL10, CXCL11, and their shared receptor CXCR3 were remarkably increased by colitis (Supplementary Fig. 7b), which were reported to mediate T-cell migration.25,27 In addition, we observed CXCR3 blockade relieved colitis-associated retinal dysfunction and neuron injury (Supplementary Fig. 8).
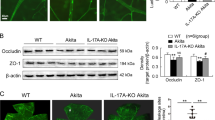
Retinal MAdCAM-1 is upregulated during colitis
We then sought to explore how T cells migrated into the retina during colitis. It has been suggested that gut-homing CD4+ T cells contribute to the induction of EIMs of IBD, and MAdCAM-1 plays a crucial role in leukocyte transendothelial migration into inflamed tissues in IBD.3,28,29 We then performed immunofluorescence staining for MAdCAM-1 in the retina and showed that colitic mice displayed significantly increased expression of MAdCAM-1 in the retinal microvessels compared with control mice (Fig. 6a). Since the intraretinal vasculature consists of three interconnected parallel vascular plexus layers in the plexiform layers of the retina (Fig. 6b),30 we asked whether MAdCAM-1 expression was different among the three layers of vascular plexus. We performed the whole-mount preparations from colitic and control mice, and staining for MAdCAM-1 revealed that three plexus layers all exhibited increased number of MAdCAM-1-expressing vessels in DSS retinas (Fig. 6c). In addition, we also observed upregulated MAdCAM-1 expression and CD4+ T-cell infiltration in the retina of IL-10−/− mice (Supplementary Fig. 9). We also used rd1 mice as a well-established retinal neurodegeneration model of human retinitis pigmentosa (RP).31,32 Since neuroinflammation has been considered as one of the major mechanisms and contribute to the pathological retinal neurodegeneration in RP,33 we asked whether up-regulation of retinal MAdCAM-1 was also involved in rd1 mice. As demonstrated in Supplementary Fig. 10a, b, 1- and 2-month aged rd1 mice suffered from severe loss of photoreceptor cells, and we did not observe detectable MAdCAM-1+ vessels in rd1 retinas. qRT-PCR also did not show any significant differences in retinal MAdCAM-1 transcript expression between rd1 mice and their WT littermates (Supplementary Fig. 10c). Because MAdCAM-1 could bind to α4β7 expressed on lymphocytes and mediate their transendothelial migration, we performed detection for α4β7 and found increased retinal infiltrating CD4+ T cells co-expressed α4β7 in colitic mice (Fig. 6d), indicative of a “gut-homing” nature.29 Meanwhile, qRT-PCR assay confirmed the increased expression of MAdCAM-1 (Fig. 6e) and α4β7 (Fig. 6f) in the retina of colitic mice.
Colitis was induced in male C57BL/6J mice (8–10 weeks old) as indicated. a Confocal image of retinal flat-mounts stained with anti-MAdCAM-1 and anti-CD4. Isolectin was used to label blood vessels. MAdCAM-1+ vessels were calculated in histogram. b Schematic diagram illustrating the three vascular plexus layers in the murine retina. c Shown was MAdCAM-1 expression in the three vascular plexuses and MAdCAM-1+ vessels were calculated in each plexus. In (a) and (c), five retinas from different mice in each group were collected for flat-mount preparation. @@@p < 0.0001, ###p < 0.0001, &&&p < 0.0001 compared with the same vessel layer in the control group. Statistical comparisons between groups were performed using paired Student’s t test (two-tailed). d Colitic mice exhibited an increased amount of retinal infiltrating α4β7+ CD4+ T cells (arrows) than controls. Five retinas from different mice in each group were collected for immunofluorescent analysis. The mRNA expression of e MAdCAM-1 and f α4β7 in retinas was examined using qRT-PCR (12 retinas were analyzed in each group). *p < 0.05, ***p < 0.001. Statistical comparisons between groups were performed using paired Student’s t test (two-tailed). The data are represented as means ± SEM. Representative results from one of three independent experiments are shown. GCL retinal ganglion cell layer, IPL inner plexiform layer, INL inner nuclear layer, OPL outer plexiform layer, ONL outer nuclear layer.
Next, we aimed to investigate the potential mechanism of mice with experimental colitis exhibited upregulated expression of MAdCAM-1. Previous studies show that TNF-α induced MAdCAM-1 expression in the endothelial cell lines via NF-κB activation.34,35 Therefore, we cultured mRMECs, a mouse retinal microvessel cell line, under stimulation of TNF-α, which was upregulated in the retina of colitic mice (Supplementary Fig. 7), and found significantly increased expression of MAdCAM-1 (Supplementary Figs. 11, 12), indicative of a potential role of TNF-α pathway in the expression of retinal MAdCAM-1.
Inhibition of MAdCAM-1 significantly reduces loss of retinal inner neurons during colitis
To further confirm whether MAdCAM-1 indeed regulated colitis-associated retinal neuron damage, we performed intravitreal injection of anti-MAdCAM-1 antibody in mice treated with DSS to block the binding between MAdCAM-1 and α4β7. First, we examined the neutralizing effect of anti-MAdCAM-1 in vitro. We induced MAdCAM-1 expression in mRMECs by TNF-α and observed anti-MAdCAM-1 indeed exert a significant neutralizing effect (Supplementary Fig. 12). For in vivo neutralization, intravitreal injection of anti-MAdCAM-1 antibody was performed in mice during the DSS insults. As shown in Supplementary Fig. 13, anti-MAdCAM-1 treatment effectively reduced the number of MAdCAM-1+ retinal vessels, and improved the retinal functions measured by ERG (Fig. 7a, b). Expectedly, after intravitreal administration of anti-MAdCAM-1, the degeneration of inner retinal neurons was remarkably alleviated (Fig. 7c, d) and retinal infiltration of T cells was markedly downregulated (Fig. 7e). Moreover, anti-MAdCAM-1 potently suppressed the activation of retinal microglia during colitis (Fig. 7f, g). The expression of pro-inflammatory cytokines was also measured and the levels of TNF-α, IL-1β, and IFN-γ expression were significantly reduced (Fig. 7h). Collectively, the data confirm the role of MAdCAM-1 in mediating colitis-induced retinal neuron degeneration.
Colitis was induced in male C57BL/6J mice (8–10 weeks old), which were intravitreally injected with anti-MAdCAM-1 as described in Methods. a, b Retinal function was measured by ERG (n = 5 mice in each group). c BPC and RGC loss was analyzed by immunofluorescent staining for PKCα and β III tubulin, respectively, and d calculated in histogram. Five retinas from different mice in each group were analyzed. e Retinal CD4+ T-cell and f microglia infiltration was analyzed by flow cytometry. g CD45mid CD11b+ microglia activation was examined by flow cytometric staining for CD86. h qRT-PCR was performed to investigate the expression of TNF-α, IL-1β, and IFN-γ. Sixteen retinas from each group were collected for flow cytometric analysis (e–g). Five retinas from different mice in each group were collected for immunofluorescent analysis (c, d). Twelve retinas from in each group were collected for mRNA analysis (h). *p < 0.05, **p < 0.01, ***p < 0.001. Statistical comparisons between groups were performed using one-way ANOVA followed by Tukey’s multiple comparisons test. The data are represented as means ± SEM. Representative results from one of three independent experiments are shown.
Discussion
Almost half of patients with IBD suffer from EIMs, which could occur in various organs, such as the liver, joints, the skin, and the eyes. Evidences have demonstrated that anterior uveitis and episcleritis are the most common EIMs of the eyes in patients with IBD, which might lead to impaired vision.36,37 Besides, retinal dysfunction in IBD patients and mice with experimental colitis has been sporadically reported where aberrant ERG, occluded retinal vessel, and reduced retinal blood flow was observed.11,13,15 However, little is known on the pathogenesis of eye EIMs especially how retinal neurons were damaged and the potential immunologic mechanisms have not been investigated. In the current study, we found that mice with experimental colitis displayed aberrant amplitudes of ERG a-, b-wave and OP, which was consistent with previous studies.11,15 We further identified significant loss of bipolar and ganglion cells during intestinal inflammation, which might be responsible for the alteration of ERG b-waves. Of note, we found that CD4+ T cells with a “gut-homing” nature infiltrated into the retina, which were mediated by upregulated MAdCAM-1 expression on retinal microvessels. Our findings reveal an unappreciated mechanism of how MAdCAM-1 contributed to inducing retinal neuron degeneration in IBD.
It has been well-established that IBD is regulated by the combination of environment, genetic, and immunological factors, and CD4+ T-cell-mediated immune responses play a central role in the pathogenesis.24 Therefore, to understand how CD4+ T cells exert their function in the disease is necessary for the treatment and prognosis. In the past few years, several research teams proposed mechanisms to explain how intestinal inflammation led to injury in extra-intestinal sites. For example, PSC has been known as a common liver EIM of IBD. About 5% of IBD patients develop PSC and over a half of PSC patients eventually suffer from IBD. The idea that PSC is an extension of intestinal inflammation cannot fully explain the fact that colectomy does not change the occurance and severity of the disease in IBD patients.38 Adams and the colleagues showed that PSC portal vein/sinusoidal endothelium expressed high level of MAdCAM-1, which was a mucosal-specific adhesion molecule and played a key part in T-cell homing to the gut, and MAdCAM-1 could recruit α4β7-expressing T cells to mediate liver inflammation.28,29 It has been proposed that lymphocytes accumulated in extra-intestinal sites might be originally primed in the gut and then aberrantly migrated to induce tissue-specific injury, which prompted us to question whether retinal infiltration of T cells during colitis was dependent on MAdCAM-1/α4β7 axis. As we presented in this study, we found retinal vessels expressed high levels of MAdCAM-1 during colitis, which enhanced the adhesion and transendothelial migration of α4β7-expressing T cells, demonstrating a previously unknown mechanism of how T cells regulated retinopathy.
Growing empirical evidence demonstrate that MAdCAM-1 might be indispensable in inducing autoimmune diseases in addition to IBD, confirming that effector T cell primarily activated in the gut play a key role in mediating inflammation in extra-intestinal sites.29 MS is a well-documented CNS autoimmune disease, characterized by dysregulated Th1/Th17 responses. Yamamura et al. recently found that a decrease in the frequency of gut-homing CD4+ T cells, in the peripheral blood of patients with secondary progressive MS (SPMS). Moreover, these cells in SPMS patients expressed higher levels of RORγt, IL-17A, and IFN-γ than those in healthy individuals, indicating an acquisition of pathogenic function. In EAE mouse mode, gut-homing CD4+ T cells were able to infiltrate into the CNS and anti-MAdCAM-1 treatment effectively alleviated the disease severity.39 In R161H mice, a spontaneous uveitis model, retina-specific T cells were originally activated in the gut, regulated by commensal microbiota, and these T cells were able to migrated into the eye and trigger autoimmune responses.6 In this study, our data demonstrated that MAdCAM-1 was upregulated in retinal vessels during colitis and anti-MAdCAM-1 treatment could significantly alleviated colitis-associated retinal neuron degeneration. Although our and other team’s findings suggested that TNF-α might induce MAdCAM-1 expression, the underlying mechanisms of how retinal MAdCAM-1 was upregulated during colitis was still mostly unknown. Numerous animal and human studies need to be performed to determine the mechanisms of aberrant MAdCAM-1 expression in the retina and develop suitable and effective therapeutic strategies. These data strongly suggest that gut-homing T cells might play an essential role in the gut-systemic immune axis, and targeted immune therapy directly against these cells might provide a novel approach in the management of autoimmune diseases.
In the current study, we found retinal CXCL9, CXCL10, and CXCL11 were remarkably upregulated in mice with colitis than control mice, which was bound to their shared receptor CXCR3.27 Chemokine-mediated recruitment of immune cells is an indispensable step in the pathogenesis of numerous inflammatory diseases, including neuroinflammation. For instance, the process of activated CD4+ T cells entering into the CNS was modulated by both adhesion molecules and chemokines during EAE, and CXCL10 was demonstrated to facilitate the migration of effector CD4+ T cells into inflamed neural tissues. Administration of anti-CXCL10 mAb significantly suppressed the accumulation of encephalitogenic CD4+ T cells in the CNS.40 CXCL10/CXCR3 axis mediated the development of glaucoma and played a predominant role in retinal neuronal cell loss.41 Here, we found that anti-CXCR3 treatment relieved colitis-associated retina injury and presume that upregulated CXCR3 and its ligands in the retina during colitis might contribute to the accumulation and polarizing of effector CD4+ T cells.
Microglia serve as sentinels in the retina and are indispensable for maintaining local immune homeostasis. Moreover, microglia play a critical role in the pathogenesis of neurodegeneration, and their proliferation and activation have been recognized as one of the earliest events in retinal neurodegenerative diseases, such as glaucoma.42 Interestingly, the crosstalk between microglia and CD4+ T cells has been reported and they reciprocally shape the chronic neurodegenerative pathology, leading to a vicious cycle.43 In the current study, microglia activation was observed to be upregulated after the first cycle of DSS treatment, when retinal neurodegeneration and gut-homing CD4+ T cell or circulating macrophage infiltration were missing (data not shown), indicating that microglia might be able to sense inflammatory signals from the gut and play a role in initiating neuroinflammation in the early stage of colitis. Notably, depletion of CD4+ T cells or inhibition of their recruitment into the retina in the late stage of colitis significantly reduced microglia activation, suggesting that CD4+ T cells might be capable of maintaining or even exaggerating microglia activation. Thus, there might exist a positive feedback loop between microglia and CD4+ T cells, which might initiate inflammatory cascades. However, there remains mostly unknown about the interactions between CD4+ T cells and microglia in the retina, and in-depth investigations are needed to help understand the crosstalk.
Although several disorders have been identified as the eye EIMs of IBD, disrupted retinal function and the underlying mechanisms have yet been investigated. Our study detailedly demonstrated the phenotype of retina in an IBD mouse model, and found severe damage of inner retinal neurons during colitis. Gut-homing CD4+ T cells were found in the retina of colitic mice through binding to MAdCAM-1 expressed in the retinal microvessels. Inhibition of MAdCAM-1 potently alleviated retinal neuron damage and T-cell recruitment by colitis. Our study has shed a new light on understanding the “gut-retina axis” and pathogenesis of retina degeneration and visual impairment in IBD patients.
Methods
Mice
Wild type (WT) male C57BL/6J mice were purchased from the Beijing Vital River Laboratory Animal Technology Co., Ltd (Beijing, China). IL-10−/− mice on a C57BL/6J background were purchased from Shanghai Model Organisms Center, Inc. (Shanghai, China), and rd1 (retinal degeneration 1, Pde6brd1) mice on a C57BL/6N background were purchased from Cyagen Biosciences (Suzhou, China). All mice enrolled in this study were raised under specific pathogen-free conditions. All animals were treated with approved protocols by the Association for Research in Vision and Ophthalmology Statement for the Use of Animals in Ophthalmic and Vision Research, and all animal experiments were approved by the Animal Care and Use Committee at Sichuan Provincial People’s Hospital.
Induction of experimental colitis and in vivo antibody administration
Experimental colitis was induced according to our previous studies.44,45 Briefly, 8–10-week-old male mice were fed with 1.8% DSS (W/V, molecular weight, 36,000–50,000 Da, MP Biomedicals, LLC; Solon, OH, USA) dissolved in drinking water for a 7-day period, followed by 3-day fresh water period of recovery. This cycle was repeated five times and counterparts treated with tap water only were used as controls. All mice were sacrificed on day 50, and retinas were collected for further analysis. For MAdCAM-1 blockade, intravitreal injection of Purified Rat Anti-Mouse MAdCAM-1 (2 μg/eye, clone MECA-367, BD Biosciences, San Diego, CA, USA) or corresponding isotype antibody (V500 Rat IgG2a, κ Isotype Control, clone R35-95, 2 μg/eye, BD Biosciences) was performed in mice on Days 30 and 40 during the DSS insults. For CD4+ T-cell depletion, intraperitoneal injection of Ultra-LEAF™ Purified anti-mouse CD4 Antibody (10 μg/g, clone GK1.5, BioLegend, San Diego, CA, USA) or corresponding isotype antibody (Ultra-LEAF Purified Rat IgG2b, κ Isotype Ctrl Antibody, clone RTK4530, 10 μg/g, BioLegend) was performed in mice on Days 30 and 40 during DSS insults. For CXCR3 blockade, intraperitoneal injection of Ultra-LEAF™ Purified anti-mouse CD183 (CXCR3) antibody (10 μg/g, clone CXCR3-173, BioLegend) or corresponding isotype antibody (Armenian Hamster IgG, clone: HTK888, BioLegend) was performed in mice every 7 days from Day 30 to 50. Male IL-10−/− mice at their age of 12 weeks were also used for spontaneous chronic colitis model, and their gender- and age-matched WT littermates served as controls.
Isolation of retinal cells and flow cytometry
Eyes were removed after mice being sacrificed. Retinas were then freshly isolated and eight retinas were pooled for cell isolation. According to our previous report,46 retinas were incubated with 2% Collagenase (W/V, Sigma-Aldrich, St. Louis, MO, USA) in RPMI 1640 medium supplemented with fetal bovine serum (FBS, Invitrogen, Thermo Fisher Scientific, USA) at 37 °C for 30 min to obtain primary retinal cells. These cells were then purified by density gradient centrifugation of 30 and 70% percoll-RPMI solution. Retinal cells then were collected from the interphase. A Mouse BD Fc Block™ purified anti-mouse CD16/CD32 mAb was incubated with retinal cells, which were then labeled by fluorescein-conjugated antibodies. The information about fluorescein-conjugated antibodies used in this study was documented in Supplementary Table 1. Flow cytometric data were acquired on a BD FACSCanto II and analyzed using FlowJo software (Tree Star, Ashland, OR, USA).
Immunohistochemistry and quantitative analysis
As reported previously,47 enucleated eyes were fixed with 4% paraformaldehyde in PBS at 4 °C for 2 h and then cryoprotected in 30% sucrose. Eyes were then embedded in optimal cutting temperature (OCT) solution and sectioned at 10 μm thickness. To ensure all sections used for quantification analysis came from the same eccentricity, the eyeballs were embedded in the same direction. Sections showing the central position of the optic nerve (ON) for staining were chosen, and photos were taken at a distance of 500–1000 μm from the optic nerve. Sections were blocked in blocking buffer containing 10% donkey serum and 0.1% Triton X-100 in PBS for 2 h at room temperature, and then incubated with indicated primary antibodies at 4 °C over night. Investigators were blinded to the experimental groups. Proper corresponding isotype control antibodies were used to differentiate non-specific background signal from specific antibody signal (Supplementary Fig. 1). The information about primary/second antibodies and corresponding isotype controls used in this study were listed in Supplementary Table 3. Sections were washed with PBS for three times, and incubated with indicated secondary antibodies for 2 h at room temperature. Confocal images were acquired on a Zeiss LSM 800 scanning microscope. To quantify BPC (identified as PKCα+), we counted the number of PKCα+ cells in the inner nuclear layer (INL), where the BPC bodies were located. Similarly, PKCα+ BPC axons were analyzed to assess the process damage of BPC. βIII tubulin was used to identify RGC bodies and axons, and the number of TUNEL+ cells in the retinal ganglion cell layer (GCL) was counted to define retinal ganglion cell (RGC) loss. Axonal length of RGC was compared using βIII tubulin staining to estimate the damage of RGC. Nestin was used as a marker for neural cell stemness, indicative of cell injury. The synaptic connections between BPC and RGC were analyzed by co-staining with PKCα and βIII tubulin. The synapses between rod photoreceptor cells and BPC in the outer nuclear layer (OPL) were identified as PSD95+. Demyelination was analyzed by the MBP-1 staining intensities in both nerve fiber layer and optic nerve. To estimate the degeneration of photoreceptors, the thickness of rod outer segments (OS) and inner segments (IS) was measured by staining for Rhodopsin and Na+/K+-ATPase, respectively. Microglia/macrophage were identified as Iba1+ and microglia was identified as Tmem119+. Isolectin was used as a marker for vessel endothelial cells. Quantitative analysis was performed using ImageJ software (version 3.1, National Institutes of Health, Bethesda, Washington). Retina sections from at least five mice per group, and five fields of each section were examined for statistical analysis.
Statistical analysis
All statistical analysis was performed using Prism 7.0 software (GraphPad Software Inc., San Diego, CA). Comparisons between groups were analyzed using paired Student’s t test (two groups) or one-way ANOVA followed by Tukey’s multiple comparisons test (more than two groups) and data were presented as mean ± SEM. Statistical significance was set at p < 0.05.
See online supplementary methods for additional information.
References
Hedin, C. R. H. et al. The pathogenesis of extraintestinal manifestations: implications for IBD research, diagnosis and therapy. J. Crohns Colitis 13, 541–554 (2018).
Harbord, M. et al. The first European evidence-based consensus on extra-intestinal manifestations in inflammatory bowel disease. J. Crohns Colitis 10, 239–254 (2016).
Eksteen, B. et al. Hepatic endothelial CCL25 mediates the recruitment of CCR9+ gut-homing lymphocytes to the liver in primary sclerosing cholangitis. J. Exp. Med. 200, 1511–1517 (2004).
Pachynski, R. K., Wu, S. W., Gunn, M. D. & Erle, D. J. Secondary lymphoid-tissue chemokine (SLC) stimulates integrin alpha 4 beta 7-mediated adhesion of lymphocytes to mucosal addressin cell adhesion molecule-1 (MAdCAM-1) under flow. J. Immunol. 161, 952–956 (1998).
Zabel, B. A. et al. Human G protein-coupled receptor GPR-9-6/CC chemokine receptor 9 is selectively expressed on intestinal homing T lymphocytes, mucosal lymphocytes, and thymocytes and is required for thymus-expressed chemokine-mediated chemotaxis. J. Exp. Med. 190, 1241–1256 (1999).
Horai, R. et al. Microbiota-dependent activation of an autoreactive T cell receptor provokes autoimmunity in an immunologically privileged site. Immunity 43, 343–353 (2015).
Hoon, M., Okawa, H., Della Santina, L. & Wong, R. O. Functional architecture of the retina: development and disease. Prog. Retin Eye Res. 42, 44–84 (2014).
Hoshino, A. et al. Molecular anatomy of the developing human retina. Dev. Cell 43, 763–779 e764 (2017).
Langrish, C. L. et al. IL-23 drives a pathogenic T cell population that induces autoimmune inflammation. J. Exp. Med. 201, 233–240 (2005).
Chen, H. et al. Commensal microflora-induced T cell responses mediate progressive neurodegeneration in glaucoma. Nat. Commun. 9, 3209 (2018).
Watts, M. N. & Harris, N. R. Anemia and retinal function in a mouse model of acute colitis. Pathophysiology 21, 301–308 (2014).
Ernst, B. B., Lowder, C. Y., Meisler, D. M. & Gutman, F. A. Posterior segment manifestations of inflammatory bowel disease. Ophthalmology 98, 1272–1280 (1991).
Seo, Y., Kim, M., Kim, J. H., Park, J. J. & Lee, S. C. Central retinal vein occlusion associated with ulcerative colitis. Optom. Vis. Sci. 93, 1567–1570 (2016).
Das, K. M. Relationship of extraintestinal involvements in inflammatory bowel disease: new insights into autoimmune pathogenesis. Dig. Dis. Sci. 44, 1–13 (1999).
Watts, M. N. et al. Ocular dysfunction in a mouse model of chronic gut inflammation. Inflamm. Bowel Dis. 19, 2091–2097 (2013).
Schiller, P. H. The ON and OFF channels of the visual system. Trends Neurosci. 15, 86–92 (1992).
Wassle, H., Puller, C., Muller, F. & Haverkamp, S. Cone contacts, mosaics, and territories of bipolar cells in the mouse retina. J. Neurosci. 29, 106–117 (2009).
Moon, C. H., Cho, H., Kim, Y. K. & Park, T. K. Nestin expression in the adult mouse retina with pharmaceutically induced retinal degeneration. J. Korean Med. Sci. 32, 343–351 (2017).
Kuhn, R., Lohler, J., Rennick, D., Rajewsky, K. & Muller, W. Interleukin-10-deficient mice develop chronic enterocolitis. Cell 75, 263–274 (1993).
Deretic, D. A role for rhodopsin in a signal transduction cascade that regulates membrane trafficking and photoreceptor polarity. Vis. Res. 46, 4427–4433 (2006).
Ford, A. L., Goodsall, A. L., Hickey, W. F. & Sedgwick, J. D. Normal adult ramified microglia separated from other central nervous system macrophages by flow cytometric sorting. Phenotypic differences defined and direct ex vivo antigen presentation to myelin basic protein-reactive CD4+ T cells compared. J. Immunol. 154, 4309–4321 (1995).
Deliyanti, D. et al. Foxp3(+) Tregs are recruited to the retina to repair pathological angiogenesis. Nat. Commun. 8, 748 (2017).
Butovsky, O. et al. Identification of a unique TGF-beta-dependent molecular and functional signature in microglia. Nat. Neurosci. 17, 131–143 (2014).
Sun, M., He, C., Cong, Y. & Liu, Z. Regulatory immune cells in regulation of intestinal inflammatory response to microbiota. Mucosal Immunol. 8, 969–978 (2015).
Groom, J. R. & Luster, A. D. CXCR3 in T cell function. Exp. Cell Res. 317, 620–631 (2011).
Trivedi, P. J. & Adams, D. H. Chemokines and chemokine receptors as therapeutic targets in inflammatory bowel disease; pitfalls and promise. J. Crohns Colitis 12, S641–S652 (2018).
Koper, O. M., Kaminska, J., Sawicki, K. & Kemona, H. CXCL9, CXCL10, CXCL11, and their receptor (CXCR3) in neuroinflammation and neurodegeneration. Adv. Clin. Exp. Med. 27, 849–856 (2018).
Grant, A. J., Lalor, P. F., Hubscher, S. G., Briskin, M. & Adams, D. H. MAdCAM-1 expressed in chronic inflammatory liver disease supports mucosal lymphocyte adhesion to hepatic endothelium (MAdCAM-1 in chronic inflammatory liver disease). Hepatology 33, 1065–1072 (2001).
Adams, D. H. & Eksteen, B. Aberrant homing of mucosal T cells and extra-intestinal manifestations of inflammatory bowel disease. Nat. Rev. Immunol. 6, 244–251 (2006).
Usui, Y. et al. Neurovascular crosstalk between interneurons and capillaries is required for vision. J. Clin. Invest. 125, 2335–2346 (2015).
Bowes, C. et al. Retinal degeneration in the rd mouse is caused by a defect in the beta subunit of rod cGMP-phosphodiesterase. Nature 347, 677–680 (1990).
Wright, A. F., Chakarova, C. F., Abd El-Aziz, M. M. & Bhattacharya, S. S. Photoreceptor degeneration: genetic and mechanistic dissection of a complex trait. Nat. Rev. Genet. 11, 273–284 (2010).
Cooper, D. N., Krawczak, M., Polychronakos, C., Tyler-Smith, C. & Kehrer-Sawatzki, H. Where genotype is not predictive of phenotype: towards an understanding of the molecular basis of reduced penetrance in human inherited disease. Hum. Genet. 132, 1077–1130 (2013).
Takeuchi, M. & Baichwal, V. R. Induction of the gene encoding mucosal vascular addressin cell adhesion molecule 1 by tumor necrosis factor alpha is mediated by NF-kappa B proteins. Proc. Natl Acad. Sci. USA 92, 3561–3565 (1995).
Sonar, S. A., Shaikh, S., Joshi, N., Atre, A. N. & Lal, G. IFN-gamma promotes transendothelial migration of CD4(+) T cells across the blood-brain barrier. Immunol. Cell Biol. 95, 843–853 (2017).
Troncoso, L. L., Biancardi, A. L., de Moraes, H. V. Jr. & Zaltman, C. Ophthalmic manifestations in patients with inflammatory bowel disease: a review. World J. Gastroenterol. 23, 5836–5848 (2017).
Watson, P. G. & Young, R. D. Scleral structure, organisation and disease. A review. Exp. Eye Res. 78, 609–623 (2004).
Grant, A. J., Lalor, P. F., Salmi, M., Jalkanen, S. & Adams, D. H. Homing of mucosal lymphocytes to the liver in the pathogenesis of hepatic complications of inflammatory bowel disease. Lancet 359, 150–157 (2002).
Kadowaki, A., Saga, R., Lin, Y., Sato, W. & Yamamura, T. Gut microbiota-dependent CCR9+CD4+ T cells are altered in secondary progressive multiple sclerosis. Brain 142, 916–931 (2019).
Fife, B. T. et al. CXCL10 (IFN-gamma-inducible protein-10) control of encephalitogenic CD4+ T cell accumulation in the central nervous system during experimental autoimmune encephalomyelitis. J. Immunol. 166, 7617–7624 (2001).
Ha, Y. et al. Endoplasmic reticulum stress-regulated CXCR3 pathway mediates inflammation and neuronal injury in acute glaucoma. Cell Death Dis. 6, e1900 (2015).
Williams, P. A., Marsh-Armstrong, N., Howell, G. R., Lasker, I. Io. A. & Glaucomatous Neurodegeneration, P. Neuroinflammation in glaucoma: A new opportunity. Exp. Eye Res. 157, 20–27 (2017).
Schetters, S. T. T., Gomez-Nicola, D., Garcia-Vallejo, J. J. & Van Kooyk, Y. Neuroinflammation: microglia and T cells get ready to tango. Front Immunol. 8, 1905 (2017).
Shi, Y. et al. Smad nuclear interacting protein 1 (SNIP1) inhibits intestinal inflammation through regulation of epithelial barrier function. Mucosal Immunol. 11, 835–845 (2018).
He, C. et al. MicroRNA 301A promotes intestinal inflammation and colitis-associated cancer development by inhibiting BTG1. Gastroenterology 152, 1434–1448. e1415 (2017).
He, C. et al. miR-301a promotes intestinal mucosal inflammation through induction of IL-17A and TNF-alpha in IBD. Gut 65, 1938–1950 (2016).
Zhang, L. et al. Loss of Tmem30a leads to photoreceptor degeneration. Sci. Rep. 7, 9296 (2017).
Acknowledgements
This work is financially supported by grants from the National Natural Science Foundation of China (U19A2004, 81970803, 81600442) and Foundation of Sichuan Science and Technology Department (2019JDTD0014).
Author information
Authors and Affiliations
Contributions
Conceptualization, methodology, writing—review and editing, supervision, and funding acquisition, F.L. and C.H.; project administration, formal analysis, and writing—original draft preparation, K.P., J.X., and J.W.; data curation and validation, Y.S., L.W., W.X., Q.C., Y.C., and P.S.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Peng, K., Xiao, J., Wang, J. et al. MAdCAM-1 mediates retinal neuron degeneration in experimental colitis through recruiting gut-homing CD4+ T cells. Mucosal Immunol 14, 152–163 (2021). https://doi.org/10.1038/s41385-020-0282-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41385-020-0282-x
This article is cited by
-
Th1 cells contribute to retinal ganglion cell loss in glaucoma in a VCAM-1-dependent manner
Journal of Neuroinflammation (2024)
-
Transcriptome analysis of AAV-induced retinopathy models expressing human VEGF, TNF-α, and IL-6 in murine eyes
Scientific Reports (2022)