Abstract
Imaging has not only an established role in screening and diagnosis of hepatocellular carcinoma (HCC) in patients with chronic liver inflammatory diseases, but also a crucial importance for patient stratification and treatment allocation, as well as for assessing treatment response. In the setting of increasing therapeutic options for HCC, the Barcelona Clinic Liver Cancer (BCLC) system still remains the most appropriate way to select candidate cohorts for best treatments. This classification takes into account the imaging information on tumor burden and extension, liver function, and cancer-related symptoms, stratifying patients in five risk categories (Stages 0, A, B, C and D) associated with different treatment options. Still now, there are no clear roles for biomarkers use in treatment allocation. The increasing use of locoregional non-surgical therapies in the different stages is highly dependent on reliable evaluation of treatment response, in particular when they are used with curative intention or for downstaging at liver transplantation re-assessment. Moreover, objective response (OR) has emerged as an important imaging biomarker, providing information on tumor biology, which can contribute for further prognostic assessment. Current guidelines for OR assessment recommend only the measurement of viable tumor according to mRECIST criteria, with further classification into complete response, partial response, stable disease or progressive disease. Either computed tomography (CT) or magnetic resonance (MR) imaging can be used for this purpose, and the Liver Imaging Reporting and Data System (LI-RADS) committee has recently provided some guidance for reporting after locoregional therapies. Nevertheless, imaging pitfalls resulting from treatment-related changes can impact with the correct evaluation of treatment response, especially after transarterial radioembolization (TARE). Volume criteria and emerging imaging techniques might also contribute for a better refinement in the assessment of treatment response and monitoring. As the role of imaging deeply expands in the multidisciplinary assessment of HCC, our main objective in this review is to discuss state-of-the-art decision-making aspects for treatment allocation and provide guidance for treatment response evaluation.








Similar content being viewed by others
Abbreviations
- AASLD:
-
American Association for the Study of Liver Diseases
- BCLC:
-
Barcelona Clinic Liver Cancer
- CEUS:
-
Contrast-enhanced ultrasound
- CR:
-
Complete response
- CT:
-
Computed tomography
- DCE-MR:
-
Dynamic contrast-enhanced magnetic resonance
- EASL:
-
European Association for the Study of the Liver
- HCC:
-
Hepatocellular carcinoma
- LI-RADS:
-
Liver Imaging Reporting and Data System
- LR-TR:
-
LI-RADS treatment response
- LT:
-
Liver transplantation
- MCA:
-
Microwave ablation
- MR:
-
Magnetic resonance
- mRECIST:
-
Modified Response Evaluation Criteria in Solid Tumors
- OR:
-
Objective response
- PD:
-
Progressive disease
- PR:
-
Partial response
- qEASL:
-
Quantitative European Association for the Study of the Liver
- RECIST:
-
Response Evaluation Criteria in Solid Tumors
- RFA:
-
Radiofrequency ablation
- SD:
-
Stable disease
- SIRT:
-
Systemic internal radiation therapy
- TACE:
-
Transarterial chemoembolization
- TARE:
-
Transarterial radioembolization
References
Fitzmaurice C, Akinyemiju T, Abera S, et al (2017). The burden of primary liver cancer and underlying etiologies from 1990 to 2015 at the global, regional, and national level results from the global burden of disease study 2015. JAMA Oncol. https://doi.org/10.1001/jamaoncol.2017.3055
Galle PR, Forner A, Llovet JM, et al (2018). EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J Hepatol. https://doi.org/10.1016/j.jhep.2018.03.019
Forner A, Reig M, Bruix J (2018). Hepatocellular carcinoma. Lancet. https://doi.org/10.1016/s0140-6736(18)30010-2
Marrero JA, Kulik LM, Sirlin CB, et al (2018). Diagnosis, Staging, and Management of Hepatocellular Carcinoma: 2018 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology. https://doi.org/10.1002/hep.29913
Llovet JM, Brú C, Bruix J (1999). Prognosis of hepatocellular carcinoma: The BCLC staging classification. Semin Liver Dis. https://doi.org/10.1055/s-2007-1007122
Yopp AC, Mansour JC, Beg MS, et al (2014). Establishment of a multidisciplinary hepatocellular carcinoma clinic is associated with improved clinical outcome. Ann Surg Oncol. https://doi.org/10.1245/s10434-013-3413-8
Darnell A, Forner A, Rimola J, et al (2015). Liver imaging reporting and data system with MR imaging: Evaluation in nodules 20 mm or smaller detected in cirrhosis at screening US. Radiology. https://doi.org/10.1148/radiol.15141132
Sala M, Fuster J, Llovet JM, et al (2004). High pathological risk of recurrence after surgical resection for hepatocellular carcinoma: An indication for salvage liver transplantation. Liver Transplant. https://doi.org/10.1002/lt.20202
Ferrer-Fàbrega J, Forner A, Liccioni A, et al (2016). Prospective validation of ab initio liver transplantation in hepatocellular carcinoma upon detection of risk factors for recurrence after resection. Hepatology. https://doi.org/10.1002/hep.28339
Germani G, Pleguezuelo M, Gurusamy K et al (2010). Clinical outcomes of radiofrequency ablation, percutaneous alcohol and acetic acid injection for hepatocellular carcinoma: A meta-analysis. J Hepatol. https://doi.org/10.1016/j.jhep.2009.12.004
Mazzaferro V, Regalia E, Doci R, et al (2002). Liver Transplantation for the Treatment of Small Hepatocellular Carcinomas in Patients with Cirrhosis. N Engl J Med. https://doi.org/10.1056/nejm199603143341104
Burra P, Burroughs A, Graziadei I, et al (2016). EASL Clinical Practice Guidelines: Liver transplantation. J Hepatol. https://doi.org/10.1016/j.jhep.2015.10.006
Raoul JL, Forner A, Bolondi L, Cheung TT, Kloeckner R, de Baere T (2019). Updated use of TACE for hepatocellular carcinoma treatment: How and when to use it based on clinical evidence. Cancer Treat Rev. https://doi.org/10.1016/j.ctrv.2018.11.002
Bolondi L, Burroughs A, Dufour JF, et al (2012). Heterogeneity of patients with intermediate (BCLC B) hepatocellular carcinoma: Proposal for a subclassification to facilitate treatment decisions. Semin Liver Dis. https://doi.org/10.1055/s-0032-1329906
Mazzaferro V, Llovet JM, Miceli R, et al (2009). Predicting survival after liver transplantation in patients with hepatocellular carcinoma beyond the Milan criteria: a retrospective, exploratory analysis. Lancet Oncol. https://doi.org/10.1016/s1470-2045(08)70284-5
Mazzaferro V (2016). Squaring the circle of selection and allocation in liver transplantation for HCC: An adaptive approach. Hepatology. https://doi.org/10.1002/hep.28420
Gramenzi A, Golfieri R, Mosconi C, et al (2015). Yttrium-90 radioembolization vs sorafenib for intermediate-locally advanced hepatocellular carcinoma: A cohort study with propensity score analysis. Liver Int. https://doi.org/10.1111/liv.12574
Keppke AL, Salem R, Reddy D, Huang J, Jin J, Larson AC, Miller FH (2007). Imaging of hepatocellular carcinoma after treatment with yttrium-90 microspheres. AJR Am J Roentgenol. 188(3):768.
Theysohn JM, Ertle J, Müller S, et al (2014). Hepatic volume changes after lobar selective internal radiation therapy (SIRT) of hepatocellular carcinoma. Clin Radiol. https://doi.org/10.1016/j.crad.2013.09.009
An C. Kim DW, Park YN et al (2015). Single Hepatocellular Carcinoma: Preoperative MR Imaging to Predict Early Recurrence after Curative Resection. Radiology. 276(2):433-43.
Park HJ, Kim JH, Choi SY et al (2017). Prediction of Therapeutic Response of Hepatocellular Carcinoma to Transcatheter Arterial Chemoembolization Based on Pretherapeutic Dynamic CT and Textural Findings. AJR Am J Roentgenol. 209(4):W211-W220.
Zhou Y, He L, Huang Y, et al (2017). CT-based radiomics signature: a potential biomarker for preoperative prediction of early recurrence in hepatocellular carcinoma. Abdom Radiol (NY). 42(6):1695-1704.
Chen S, Zhu Y, Liu Z, Liang C (2017). Texture analysis of baseline multiphasic hepatic computed tomography images for the prognosis of single hepatocellular carcinoma after hepatectomy: A retrospective pilot study. Eur J Radiol. 90:198-204.
Wu M, Tan H, Gao F, et al (2018). Predicting the grade of hepatocellular carcinoma based on non-contrast-enhanced MRI radiomics signature. Eur Radiol. https://doi.org/10.1007/s00330-018-5787-2
Mulé S, Thiefin G, Costentin C et al (2018). Advanced Hepatocellular Carcinoma: Pretreatment Contrast-enhanced CT Texture Parameters as Predictive Biomarkers of Survival in Patients Treated with Sorafenib. Radiology. 288(2):445-455.
Martí-Bonmatí L, Alberich-Bayarri A, Garcí-Marí G et al (2012). Imaging biomarkers, quantitative imaging, and bioengineering. Radiologia. 54(3):269-78. https://doi.org/10.1016/j-rx-2010-12-013
Chen S, Feng S, Wei J et al (2019). Pretreatment prediction of immunoscore in hepatocellular cancer: a radiomics-based clinical model based on Gd-EOB-DTPA-enhanced MRI imaging. Eur Radiol. 29(8):4177-4187. https://doi.org/10.1007/s00330-018-5986-x
Sala M, Llovet JM, Vilana R, et al (2004). Initial response to percutaneous ablation predicts survival in patients with hepatocellular carcinoma. Hepatology. https://doi.org/10.1002/hep.20465
N’Kontchou G, Mahamoudi A, Aout M, et al (2009). Radiofrequency ablation of hepatocellular carcinoma: Long-term results and prognostic factors in 235 western patients with cirrhosis. Hepatology. https://doi.org/10.1002/hep.23181
Poon RTP, Sheung TF, Chung M Lo, Chi LL, Wong J (2002). Long-term survival and pattern of recurrence after resection of small hepatocellular carcinoma in patients with preserved liver function: Implications for a strategy of salvage transplantation. Ann Surg. https://doi.org/10.1097/00000658-200203000-00009
Tabrizian P, Jibara G, Shrager B, Schwartz M, Roayaie S (2015). Recurrence of Hepatocellular Cancer after Resection: Patterns, Treatments, and Prognosis. Ann Surg. https://doi.org/10.1097/sla.0000000000000710
Kielar A, Fowler KJ, Lewis S, et al (2018). Locoregional therapies for hepatocellular carcinoma and the new LI-RADS treatment response algorithm. Abdom Radiol. https://doi.org/10.1007/s00261-017-1281-6
Llovet JM, Mas X, Aponte JJ, et al (2002). Cost effectiveness of adjuvant therapy for hepatocellular carcinoma during the waiting list for liver transplantation. Gut. https://doi.org/10.1136/gut50.1.123
Cescon M, Cucchetti A, Ravaioli M, Pinna AD (2013). Hepatocellular carcinoma locoregional therapies for patients in the waiting list. Impact on transplantability and recurrence rate. J Hepatol. https://doi.org/10.1016/j.jhep.2012.09.021
Vincenzi B, Di Maio M, Silletta M, et al (2015). Prognostic relevance of objective response according to EASL criteria and mRECIST criteria in hepatocellular carcinoma patients treated with loco-regional therapies: A literature-based meta-analysis. PLoS One. https://doi.org/10.1371/journal.pone.0133488
Lencioni R, Montal R, Torres F, et al (2017). Objective response by mRECIST as a predictor and potential surrogate end-point of overall survival in advanced HCC. J Hepatol. 66(6):1166–1172.
Adcock CS, Florez E, Zand KA, Patel A, Howard CM, Fatemi A (2018). Assessment of Treatment Response Following Yttrium-90 Transarterial Radioembolization of Liver Malignancies. Cureus. https://doi.org/10.7759/cureus.2895
Gordic S, Corcuera-Solano I, Stueck A, et al (2017). Evaluation of HCC response to locoregional therapy: Validation of MRI-based response criteria versus explant pathology. J Hepatol. https://doi.org/10.1016/j.jhep.2017.07.030
Hussein RS, Tantawy W, Abbas YA (2019). MRI assessment of hepatocellular carcinoma after locoregional therapy. Insights Imaging. https://doi.org/10.1186/s13244-019-0690-1
Bruix J, Reig M, Rimola J, et al (2011). Clinical decision making and research in hepatocellular carcinoma: Pivotal role of imaging techniques. Hepatology. https://doi.org/10.1002/hep.24670
Lencioni R, Llovet JM (2010). Modified RECIST (mRECIST) assessment for hepatocellular carcinoma. Semin Liver Dis. https://doi.org/10.1055/s-0030-1247132
Vogel A, Cervantes A, Chau I, et al (2018). Hepatocellular carcinoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. https://doi.org/10.1093/annonc/mdy308
Voizard, N., Cerny, M., Assad, A. et al (2019). Assessment of hepatocellular carcinoma treatment response with LI-RADS: a pictorial review. Insights Imaging. 10, 121. https://doi.org/10.1186/s13244-019-0801-z
Erin L. Shropshire, Mohammad Chaudhry, Chad M. Miller, Brian C. Allen, Erol Bozdogan, Diana M. Cardona, Lindsay Y. King, Gemini L. Janas, Richard K. Do, Charles Y. Kim, James Ronald MRB (2019). LI-RADS Treatment Response Algorithm: Performance and Diagnostic Accuracy. Radiology. 00(0):1–9. https://doi.org/10.1148/radiol.2019182135
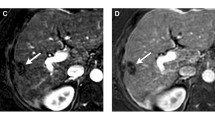
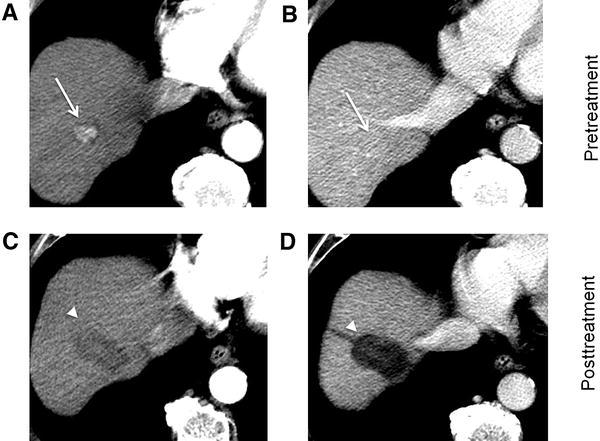
Semaan S, Makkar J, Lewis S, Chatterji M, Kim E, Taouli B (2017). Imaging of hepatocellular carcinoma response after 90y radioembolization. Am J Roentgenol. https://doi.org/10.2214/ajr.17.17993
Chaudhry M, McGinty KA, Mervak B, et al (2019). The LI-RADS version 2018 MRI treatment response algorithm: evaluation of ablated hepatocellular carcinoma. Radiology. https://doi.org/10.1148/radiol.2019191581.
Chapiro J, Wood LD, De Lin M, et al (2014). Radiologic-pathologic analysis of contrast-enhanced and diffusion-weighted MR imaging in patients with HCC after TACE: Diagnostic accuracy of 3D quantitative image analysis. Radiology. https://doi.org/10.1148/radiol.14140033
Tacher V, Lin M De, Duran R, et al (2016). Comparison of existing response criteria in patients with hepatocellular carcinoma treated with transarterial chemoembolization using a 3D quantitative approach. Radiology. https://doi.org/10.1148/radiol.2015142951
Chapiro J, Duran R, Lin M De, et al (2015). Early survival prediction after intra-arterial therapies: a 3D quantitative MRI assessment of tumour response after TACE or radioembolization of colorectal cancer metastases to the liver. Eur Radiol. https://doi.org/10.1007/s00330-015-3595-5
Sahin H, Harman M, Cinar C, Bozkaya H, Parildar M, Elmas N (2012). Evaluation of treatment response of chemoembolization in hepatocellular carcinoma with diffusion-weighted imaging on 3.0-T MR imaging. J Vasc Interv Radiol. https://doi.org/10.1016/j.jvir.2011.08.030
Taouli B, Johnson RS, Hajdu CH, et al (2013). Hepatocellular carcinoma: Perfusion quantification with dynamic contrast-enhanced MRI. Am J Roentgenol. https://doi.org/10.2214/ajr.12.9798
Spârchez Z, Mocan T, Radu P, et al (2016). Contrast enhanced ultrasonography in assessing the treatment response to transarterial chemoembolization in patients with hepatocellular carcinoma. Med Ultrason. https://doi.org/10.11152/mu.2013.2066.181.scz
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Amorim, J., França, M., Perez-Girbes, A. et al. Critical review of HCC imaging in the multidisciplinary setting: treatment allocation and evaluation of response. Abdom Radiol 45, 3119–3128 (2020). https://doi.org/10.1007/s00261-020-02470-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-020-02470-1