Abstract
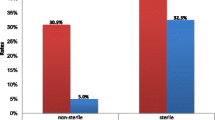
MDR uropathogens lead to high-level morbidity and mortality and pose a tremendous threat towards treatment failure and survival of UTI patients. This study was conducted to evaluate the demographic characteristics, antibiogram, and resistance pattern of Escherichia coli against antibiotics—a retrospective study at Nishtar Medical Hospital in Multan, from June 2016 to July 2017. A total of 150 clinical samples were collected and biochemically characterized by Berge’s manual, and antimicrobial susceptibility testing was performed by using the Kirby–Bauer disc diffusion method and the results were interpreted according to Clinical and Laboratory Standards Institute standards. Data was analyzed by the XL-stat software. Results indicate that UTI was more prevalent in rural areas such as Alipur (28.6%) and Jalalpur (18%) and less common in urban areas like Muzaffargarh (2.66) and Multan (2%). A total of 150 patients were examined, of which 88 were females and 62 males in which more frequently found pathogens were E. coli (33%) and others Klebsiella pneumonia (18%), Proteus (10%), Staphylococcus saprophyticus (8.66%), Staphylococcus aureus (7.33%), Pseudomonas aeruginosa (6.66%), Enterobacter (6%), Candida (5.33%), and Citrobacter (4.66%). The antimicrobial susceptibility testing was carried out against E. coli strains that showed the highest overall resistance patterns of imipenem (IMI), Cip, Aug, Cfm, and CN, which were 80%, 72%, 68%, 60%, and 52%, respectively. MDR E. coli strains showed the highest resistance pattern towards IMI which put through alarming situation in Pakistan. Significant results showed that TZP, AK, and F were found sensitive in vitro against E. coli isolates of UTIs. Prevalence of MDR uropathogens near around Multan has been first time documented in this study with respect to possible risk factors associated with UTI. These alarming signs of MDR E. coli have been rarely addressed and warrant attention on urgent basis.







Similar content being viewed by others
References
Rosen DA, Hooton TM, Stamm WE, Humphrey PA, Hultgren SJ. Detection of intracellular bacterial communities in human urinary tract infection. PLoS Med. 2007;4(12):e329. https://doi.org/10.1371/journal.pmed.0040329.
Klumpp DJ, Rycyk MT, Chen MC, Thumbikat P, Sengupta S, Schaeffer AJ. Uropathogenic Escherichia coli induces extrinsic and intrinsic cascades to initiate urothelial apoptosis. Infect Immun. 2006;74(9):5106–13. https://doi.org/10.1128/IAI.00376-06.
Hsueh PR, Hoban DJ, Carmeli Y, Chen SY, Desikan S, Alejandria M, et al. Consensus review of the epidemiology and appropriate antimicrobial therapy of complicated urinary tract infections in Asia-Pacific region. J Infect. 2011;63(2):114–23. https://doi.org/10.1016/j.jinf.2011.05.015.
Moue A, Aktaruzzaman SA, Ferdous N, Karim MR, Khalil MM, Das AK. Prevalence of urinary tract infection in both outpatient department and in patient department at a medical college setting of Bangladesh. Int J Biosci. 2015;7(5):146–52. https://doi.org/10.12692/ijb/7.5.146-152.
Bano K, Khan J, Begum RH, Munir S, Akbar N, Ansari JA, et al. Patterns of antibiotic sensitivity of bacterial pathogens among urinary tract infections (UTI) patients in a Pakistani population. Afr J Microbiol Res. 2012;6(2):414–20. https://doi.org/10.5897/AJMR11.1171.
Ukah UV, Glass M, Avery B, Daignault D, Mulvey MR, Reid-Smith RJ, et al. Risk factors for acquisition of multidrug-resistant Escherichia coli and development of community-acquired urinary tract infections. Epidemiol Infect. 2018;146(1):46–57. https://doi.org/10.1017/S0950268817002680.
Wiedemann B, Heisig A, Heisig P. Uncomplicated urinary tract infections and antibiotic resistance—epidemiological and mechanistic aspects. Antibiotics. 2014;3(3):341–52. https://doi.org/10.3390/antibiotics3030341.
Iqbal T, Naqvi R, Akhter SF. Frequency of urinary tract infection in renal transplant recipients and effect on graft function. JPMA-Journal of the Pakistan Medical Association. 2010;60(10):826.
Ganeswaran D, Sweeney C, Yousif F, Lang S, Goodman C, Nabi G. Population-based linkage of health records to detect urological complications and hospitalisation following transrectal ultrasound-guided biopsies in men suspected of prostate cancer. World J Urol. 2014;32(2):309–15. https://doi.org/10.1007/s00345-012-0893-2.
Gondos AS, Al-Moyed KA, Al-Robasi AB, Al-Shamahy HA, Alyousefi NA. Urinary tract infection among renal transplant recipients in Yemen. PloS one. 2015;10(12):e0144266. https://doi.org/10.1371/2Fjournal.pone.0144266.
Veroux M, Giuffrida G, Corona D, Gagliano M, Scriffignano V, Vizcarra D, Tallarita T, Zerbo D, Virgilio C, Sciacca A, Cappello D. Infective complications in renal allograft recipients: epidemiology and outcome. In Transplantation proceedings. Elsevier. 2008;40(6):1873–76. https://doi.org/10.1016/j.transproceed.2008.05.065.
Erdem I, Ali RK, Ardic E, Omar SE, Mutlu R, Topkaya AE. Community-acquired lower urinary tract infections: Etiology, antimicrobial resistance, and treatment results in female patients. J Global Infect Dis. 2018;10(3):129–132. https://doi.org/10.4103/2jgid.jgid_86_17.
Oliveira J, Reygaert WC. Gram negative bacteria. InStatPearls. 2019. 9. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/pubmed/30855801. Accessed 9 Mar 2010
Sabir S, Anjum AA, Ijaz T, Ali MA. Isolation and antibiotic susceptibility of E. coli from urinary tract infections in a tertiary care hospital. Pakistan journal of medical sciences. 2014;30(2):389 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3999016/.
Otter JA, Galletly TJ, Davies F, Hitchcock J, Gilchrist MJ, Dyakova E, et al. Planning to halve Gram-negative bloodstream infection: getting to grips with healthcare-associated Escherichia coli bloodstream infection sources. J Hosp Infect. 2019;101(2):129–33. https://doi.org/10.1016/j.jhin.2018.07.033.
Oladeinde BH, Omoregie R, Oladeinde OB. Asymptomatic urinary tract infection among pregnant women receiving ante-natal care in a traditional birth home in Benin City, Nigeria. Ethiop J Health Sci. 2015;25(1):3–8. https://doi.org/10.4314/ejhs.v25i1.2.
Nairoukh YR, Mahafzah AM, Irshaid A, Shehabi AA. Molecular characterization of multidrug resistant uropathogenic E. coli isolates from Jordanian patients. The open microbiology journal. 2018;12:1. https://doi.org/10.2174/1874285801812010001.
Dever LA, Dermody TS. Mechanisms of bacterial resistance to antibiotics. Arch Intern Med. 1991;151(5):886–95. https://doi.org/10.1001/archinte.1991.00400050040010.
Babypadmini S, Appalaraju B. Extended spectrum-lactamases in urinary isolates of Escherichia coli and Klebsiella pneumoniae-prevalence and susceptibility pattern in a tertiary care hospital. Indian J Med Microbiol. 2004;22(3):172. http://www.ijmm.org/text.asp?2004/22/3/172/11212–4.
Khawcharoenporn T, Vasoo S, Singh K. Urinary tract infections due to multidrug-resistant Enterobacteriaceae: prevalence and risk factors in a Chicago Emergency Department. Emergency medicine international. 2013. https://doi.org/10.1155/2013/258517.
Ny S, Edquist P, Dumpis U, Gröndahl-Yli-Hannuksela K, Hermes J, Kling AM, et al. Antimicrobial resistance of Escherichia coli isolates from outpatient urinary tract infections in women in six European countries including Russia. Journal of global antimicrobial resistance. 2019;17:25–34. https://doi.org/10.1016/j.jgar.2018.11.004.
Jean SS, Coombs G, Ling T, Balaji V, Rodrigues C, Mikamo H, et al. Epidemiology and antimicrobial susceptibility profiles of pathogens causing urinary tract infections in the Asia-Pacific region: results from the Study for Monitoring Antimicrobial Resistance Trends (SMART), 2010–2013. Int J Antimicrob Agents. 2016;47(4):328–34. https://doi.org/10.1016/j.ijantimicag.2016.01.008.
Aghazadeh M, Sari S, Nahaie M, Hashemi SS, Mehri S. Prevalence and antibiotic susceptibility pattern of E. coli isolated from urinary tract infection in patients with renal failure disease and renal transplant recipients. Trop J Pharm Res. 2015;14(4):649–53. https://doi.org/10.4314/tjpr.v14i4.13.
Bamnote PT, Ovhal RS, Kulkarni DM, More SK. Prevalence of urinary tract infections and its antibiogram in diabetic and non-diabetic patients attending tertiary care hospital in Maharashtra. International Journal of Medical Microbiology and Tropical Diseases. 2018;4(2):76–9. https://doi.org/10.18231/2581-4761.2018.0017.
Kiffer CR, Mendes C, Oplustil CP, Sampaio JL. Antibiotic resistance and trend of urinary pathogens in general outpatients from a major urban city. International braz j urol. 2007;33(1):42–9. https://doi.org/10.1590/S1677-55382007000100007.
Al Benwan K, Al Sweih N, Rotimi VO. Etiology and antibiotic susceptibility patterns of community-and hospital-acquired urinary tract infections in a general hospital in Kuwait. Med Princ Pract. 2010;19(6):440–6. https://doi.org/10.1159/000320301.
Washington JA, editor. Laboratory procedures in clinical microbiology. Springer Science & Business Media; 2012; 248–268. https://doi.org/10.1007/978-1-4612-5070-8
Hudzicki J. Kirby-Bauer disk diffusion susceptibility test protocol.12:2009.
Balouiri M, Sadiki M, Ibnsouda SK. Methods for in vitro evaluating antimicrobial activity: a review. Journal of pharmaceutical analysis. 2016;6(2):71–9. https://doi.org/10.1016/j.jpha.2015.11.005.
CLSI, Performance standards for antimicrobial disk susceptibility tests, Approved Standard, 7th ed., CLSI document M02-A11. Clinical and Laboratory Standards Institute, 950 West Valley Road, Suite 2500, Wayne, Pennsylvania 19087, USA, 2012.
Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18(3):268–81. https://doi.org/10.1111/j.14690691.2011.03570.x.
Dhodi DK, et al. A study to evaluate prescribing pattern of antibiotics among patients of urinary tract infection with preexisting renal disorders in a tertiary care hospital. International Journal of Basic& Clinical Pharmacology. 2017;3(4):687–91. https://doi.org/10.5455/2319-2003.ijbcp20140825.
Pallett A, Hand K. Complicated urinary tract infections: practical solutions for the treatment of multiresistant Gram-negative bacteria. J Antimicrob Chemother. 2010;65(suppl_3):iii25–33. https://doi.org/10.1093/jac/dkq298.
Manjula NG, Math GC, Patil A, Gaddad SM, Shivannavar CT. Incidence of urinary tract infections and its aetiological agents among pregnant women in Karnataka region. Advances in Microbiology. 2013;3(06):473. https://doi.org/10.4236/aim.2013.36063.
Hu KK, Boyko EJ, Scholes D, Normand E, Chen CL, Grafton J, et al. Risk factors for urinary tract infections in postmenopausal women. Arch Intern Med. 2004;164(9):989–93. https://doi.org/10.1001/archinte.164.9.989.
Carlsson S, Weitzberg E, Wiklund P, Lundberg JO. Intravesical nitric oxide delivery for prevention of catheter-associated urinary tract infections. Antimicrob Agents Chemother. 2005;49(6):2352–5. https://doi.org/10.1128/AAC.49.6.2352-2355.2005.
Hazelett SE, Tsai M, Gareri M, Allen K. The association between indwelling urinary catheter use in the elderly and urinary tract infection in acute care. BMC Geriatr. 2006;6(1):15. https://doi.org/10.1186/1471-2318-6-15.
Zarb P, Coignard B, Griskeviciene J, Muller A, Vankerckhoven V, Weist K, et al. The European Centre for Disease Prevention and Control (ECDC) pilot point prevalence survey of healthcare-associated infections and antimicrobial use. Eurosurveillance. 2012;17(46):20316.
Karam MR, Habibi M, Bouzari S. Urinary tract infection: pathogenicity, antibiotic resistance and development of effective vaccines against Uropathogenic Escherichia coli. Mol Immunol. 2019;108:56–67. https://doi.org/10.1016/j.molimm.2019.02.007.
Hertting O. Urinary tract infection: pathogenesis and complications. Instförmikrobiologi, tumör-ochcellbiologi/Dept of Microbiology, Tumor and Cell Biology; 2011 https://doi.org/10.1046/j.1365-2249.2003.02076.x
Liu HY, Lin HC, Lin YC, Yu SH, Wu WH, Lee YJ. Antimicrobial susceptibilities of urinary extended-spectrum beta-lactamase-producing Escherichia coli and Klebsiella pneumoniae to fosfomycin and nitrofurantoin in a teaching hospital in Taiwan. J Microbiol Immunol Infect. 2011;44(5):364–8. https://doi.org/10.1016/j.jmii.2010.08.012.
Xie J, Peters BM, Li B, Li L, Yu G, Xu Z, et al. Clinical features and antimicrobial resistance profiles of important Enterobacteriaceae pathogens in Guangzhou representative of Southern China, 2001–2015. Microb Pathog. 2017;107:206–11. https://doi.org/10.1016/j.micpath.2017.03.038.
Oladeinde BH, Omoregie R, Olley M, Anunibe JA. Urinary tract infection in a rural community of Nigeria. N Am J Med Sci. 2011;3(2):75. https://doi.org/10.4297/najms.2011.375.
Acknowledgments
We would like to thank Dr. Asghar Javaid (Nishtar Medical Hospital Multan) for his help during the research work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the Institutional Ethics Committee of Nishtar Medical University, Multan, Pakistan.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Consent for Publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Medicine
Rights and permissions
About this article
Cite this article
Fatima, T., Rafiq, S., Iqbal, A. et al. Prevalence and Antibiogram of MDR E. coli Strains Isolated from UTI Patients—1-Year Retrospective Study at Nishtar Medical Hospital, Multan. SN Compr. Clin. Med. 2, 423–431 (2020). https://doi.org/10.1007/s42399-020-00246-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42399-020-00246-8