Abstract
Background
Black men have significantly higher incidence and are up to three times more likely to die of prostate cancer (PCa) than White men. Multiparametric magnetic resonance imaging-ultrasound fusion biopsy (FBx) has emerged as a promising modality for the detection of PCa. The goal of our study is to identify differences in utilization of FBx between Black and White men presenting with suspicion of PCa.
Methods
We performed a retrospective review of Black and White men who presented with suspicion of PCa and required biopsy from January 2014 to December 2018. Multivariate logistic regression analysis was done to study the influence of race on the utilization of FBx.
Results
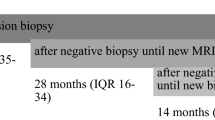
Six hundred nineteen (Black: 182, White: 437) men were included in the study. Forty-one out of 182 (22.5%) Black men underwent FBx compared with 225/437 (51.5%) of White men (P < 0.001). After adjusting for age, race, prostate-specific antigen level, digital rectal exam, family history of PCa and health insurance provider, Black race was found to be a significant negative predictor of obtaining FBx (OR:0.32, 95% CI: 0.21–0.51, P < 0.001). Black race stayed an independent negative predictor (OR: 0.36, 95% CI: 0.20–0.64, P < 0.001) in the cohort of patients who were biopsy naïve; however, although reduced, there was no significant difference in the cohort with a prior negative biopsy (OR: 0.51, 95% CI: 0.19–1.36, P = 0.179).
Conclusions
Although FBx is a superior modality for early detection of PCa, we found that Black men were less likely to undergo FBx when presenting with PCa suspicion. Further investigation is needed to evaluate if this difference is patient preference or if there are underlying socioeconomic, cultural or provider biases influencing this disparity.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Sonn GA, Chang E, Natarajan S, Margolis DJ, Macairan M, Lieu P, et al. Value of targeted prostate biopsy using magnetic resonance-ultrasound fusion in men with prior negative biopsy and elevated prostate-specific antigen. Eur Urol. 2014;65:809–15.
Mohler JL, Antonarakis ES. NCCN guidelines updates: management of prostate cancer. J Natl Compr Cancer Netw. 2019;17:583–6.
Rosenkrantz AB, Verma S, Choyke P, Eberhardt SC, Eggener SE, Gaitonde K, et al. Prostate magnetic resonance imaging and magnetic resonance imaging targeted biopsy in patients with a prior negative biopsy: a consensus statement by AUA and SAR. J Urol. 2016;196:1613–18. https://doi.org/10.1016/j.juro.2016.06.079.
Hoffman RM, Gilliland FD, Eley JW, Harlan LC, Stephenson RA, Stanford JL, et al. Racial and ethnic differences in advanced-stage prostate cancer: the prostate cancer outcomes study. J Natl Cancer Inst. 2001;93:388–95.
Shin T, Smyth TB, Ukimura O, de Castro Abreu AL, Oishi M, Mimata H, et al. Detection of prostate cancer using magnetic resonance imaging/ultrasonography image-fusion targeted biopsy in African-American men. BJU Int. 2017;120:233–8.
Mahal BA, Berman RA, Taplin ME, Huang FW. Prostate cancer-specific mortality across gleason scores in black vs nonblack men. JAMA 2018;320:2479–81.
Mahal BA, Alshalalfa M, Spratt DE, Davicioni E, Zhao SG, Feng FY, et al. Prostate cancer genomic-risk differences between African-American and white men across Gleason scores. Eur Urol. 2019;75:1038–40.
Howlader N, Noone AM, Krapcho M, Miller D, Brest A, Yu M, et al. SEER Cancer Statistics Review, 1975-2016, National Cancer Institute. Bethesda, MD, https://seer.cancer.gov/csr/1975_2016/, based on November 2018 SEER data submission, posted to the SEER web site, April 2019.
Weinreb JC, Barentsz JO, Choyke PL, Cornud F, Haider MA, Macura KJ, et al. PI-RADS prostate imaging-reporting and data system: 2015, version 2. Eur Urol. 2016;69:16–40.
DeSantis CE, Miller KD, Goding Sauer A, Jemal A, Siegel RL. Cancer statistics for African Americans, 2019. CA Cancer J Clin. 2019;69:211–33.
Sidana A, Watson MJ, George AK, Rastinehad AR, Vourganti S, Rais-Bahrami S, et al. Fusion prostate biopsy outperforms 12-core systematic prostate biopsy in patients with prior negative systematic biopsy: a multi-institutional analysis. Urol Oncol. 2018;36:341.e1–341.e7.
Fulgham PF, Rukstalis DB, Turkbey IB, Rubenstein JN, Taneja S, Carroll PR, et al. AUA policy statement on the use of multiparametric magnetic resonance imaging in the diagnosis, staging and management of prostate cancer. J Urol. 2017;198:832–8.
Bjurlin MA, Carroll PR, Eggener S, Fulgham PF, Margolis DJ, Pinto PA, et al. Update of the standard operating procedure on the use of multiparametric magnetic resonance imaging for the diagnosis, staging and management of prostate cancer. J Urol. 2019; 101097JU0000000000000617.
Krimphove MJ, Cole AP, Fletcher SA, Harmouch SS, Berg S, Lipsitz SR, et al. Evaluation of the contribution of demographics, access to health care, treatment, and tumor characteristics to racial differences in survival of advanced prostate cancer. Prostate Cancer Prostatic Dis. 2019;22:125–36. https://doi.org/10.1038/s41391-018-0083-4.
Dess RT, Hartman HE, Mahal BA, Soni PD, Jackson WC, Cooperberg MR, et al. Association of black race with prostate cancer-specific and other-cause mortality. JAMA Oncol. 2019;5:975–83.
Han PK, Kobrin S, Breen N, Joseph DA, Li J, Forsch DL, et al. National evidence on the use of shared decision making in prostate-specific antigen screening. Ann Fam Med. 2013;11:306–14.
Hoffman RM. Clinical practice. Screening for prostate cancer. N. Engl J Med. 2011;365:2013–9.
Kennedy BR, Mathis CC, Woods AK. African Americans and their distrust of the health care system: healthcare for diverse populations. J Cult Divers. 2007;14:56–60.
Jacobs EA, Rolle I, Ferrans CE, Whitaker EE, Warnecke RB. Understanding African Americans’ views of the trustworthiness of physicians. J Gen Intern Med. 2006;21:642–7.
Armstrong K, McMurphy S, Dean L, Micco E, Putt M, Halbert CH, et al. Differences in the patterns of healthcare system distrust between blacks and whites. J Gen Intern Med. 2008;23:827.
Halbert CH, Weathers B, Belmoor E, Mahler B, Coyne J, Thompson HS, et al. Racial differences in medical mistrust among men diagnosed with prostate cancer. Cancer. 2009;115:2553–61. https://doi.org/10.1002/cncr.24249
Bustillo NE, McGinty HL, Dahn JR, Yanez B, Antoni MH, Kava BR, et al. Fatalism, medical mistrust and pretreatment health-related quality of life in ethnically diverse prostate cancer patients. Psychooncology 2017;26:323–9. https://doi.org/10.1002/pon.4030
Moore AD, Hamilton JB, Knafl GJ, Godley PA, Carpenter WR, Bensen JT, et al. The influence of mistrust, racism, religious participation, and access to care on patient satisfaction for African American men: the North Carolina-Louisiana Prostate Cancer Project. J Natl Med Assoc 2013;105:59–68. Spring
Pietro GD, Chornokur G, Kumar NB, Davis C, Park JY. Racial differences in the diagnosis and treatment of prostate cancer. Int Neurourol J. 2016;20 Suppl 2:S112–S119. https://doi.org/10.5213/inj.1632722.361.
Bhuyan SS, Chandak A, Gupta N, Isharwal S, LaGrange C, Mahmood A, et al. Patient-provider communication about prostate cancer screening and treatment: new evidence from the Health Information National Trends Survey. Am J Mens Health. 2017;11:134–46. https://doi.org/10.1177/1557988315614082.
Altonji JG, Doraszelski U, Segal L. Black/white differences in wealth. Econ Perspect. 2000;24:38–50.
Arroyo-Johnson C, Mincey KD. Obesity epidemiology worldwide. Gastroenterol Clin North Am. 2016;45:571–9. https://doi.org/10.1016/j.gtc.2016.07.012
Raley RK, Sweeney MM, Wondra D. The growing racial and ethnic divide in U.S. marriage patterns. Future Child. 2015;25:89–109.
Arnett MJ, Thorpe RJ Jr, Gaskin DJ, Bowie JV, LaVeist TA. Race, medical mistrust, and segregation in primary care as usual source of care: findings from the exploring health disparities in integrated communities study. J Urban Health. 2016;93:456–67. https://doi.org/10.1007/s11524-016-0054-9.
Tehranifar P, Neugut AI, Phelan JC, Link BG, Liao Y, Desai M, et al. Medical advances and racial/ethnic disparities in cancer survival. Cancer Epidemiol Biomark Prev. 2009;18:2701–8. https://doi.org/10.1158/1055-9965.EPI-09-0305
Sabin J, Nosek BA, Greenwald A, Rivara FP. Physicians’ implicit and explicit attitudes about race by MD race, ethnicity, and gender. J Health Care Poor Underserved. 2009;20:896–913. https://doi.org/10.1353/hpu.0.0185.
Hall WJ, Chapman MV, Lee KM, Merino YM, Thomas TW, Payne BK, et al. Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: a systematic review. Am J Public Health. 2015;105:e60–e76. https://doi.org/10.2105/AJPH.2015.302903
Penner LA, Dovidio JF, Gonzalez R, Albrecht TL, Chapman R, Foster T, et al. The effects of oncologist implicit racial bias in racially discordant oncology interactions. J Clin Oncol. 2016;34:2874–80. https://doi.org/10.1200/JCO.2015.66.3658.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hoge, C., Verma, S., Lama, D.J. et al. Racial disparity in the utilization of multiparametric MRI–ultrasound fusion biopsy for the detection of prostate cancer. Prostate Cancer Prostatic Dis 23, 567–572 (2020). https://doi.org/10.1038/s41391-020-0223-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-020-0223-5
This article is cited by
-
Disparities in prostate cancer diagnosis and management: recognizing that disparities exist at all junctures along the prostate cancer journey
Prostate Cancer and Prostatic Diseases (2023)
-
Review of Active Surveillance in Underrepresented and High-Risk Populations: Feasibility and Safety
Current Urology Reports (2023)
-
Substantial Gleason reclassification in Black men with national comprehensive cancer network low-risk prostate cancer – A propensity score analysis
Prostate Cancer and Prostatic Diseases (2022)