Abstract
Bortezomib-based regimens are widely used as induction therapy for multiple myeloma (MM). Unlike lenalidomide, the role of bortezomib in consolidation and maintenance therapy for MM is less clear. We performed a meta-analysis to evaluate the impact of bortezomib-based consolidation and maintenance therapy on survival outcomes and adverse events. PubMed, Web of Science, Embase databases, and major conference proceedings were searched for randomized controlled trials (RCTs) of bortezomib-based regimens as consolidation or maintenance therapy for MM. Ten RCTs enrolling 3147 patients were included in the meta-analysis. Bortezomib-based regimens were compared with regimens without bortezomib or observation. The meta-analysis suggested that bortezomib-based maintenance therapy improved progression-free survival (PFS; hazard ratio [HR] = 0.72, 95% CI 0.55–0.95, P = 0.02) and overall survival (OS; HR = 0.71, 95% CI 0.58–0.87, P = 0.001). Bortezomib-based consolidation therapy improved PFS (HR = 0.77, 95% CI 0.68–0.88, P < 0.001) but not OS (HR = 0.98, 95% CI 0.78–1.24, P = 0.87). Bortezomib-based consolidation/maintenance therapy led to a trend toward increased risk of grade ≥ 3 neurologic symptoms, gastrointestinal symptoms, and fatigue. More research is warranted to further assess the role of bortezomib-based consolidation and maintenance therapy for multiple myeloma.
Similar content being viewed by others
Introduction
Multiple myeloma (MM) is a clonal plasma cell neoplasm that is associated with significant morbidity and mortality. It is the second most common hematologic malignancy, accounting for about 1% of all cancers1. Better understanding of the disease’s pathophysiology has led to recent advances in therapy and improved patient outcomes dramatically. The initial treatment of newly diagnosed MM patients who are transplant-eligible is induction chemotherapy with a triple-drug regimen followed by high-dose chemotherapy and autologous stem cell transplantation (ASCT). For transplant-ineligible patients, triplet or doublet drug combinations are typically recommended for induction therapy2. Despite therapeutic advancements and the availability of novel drugs, disease relapse is inevitable for the majority of patients after the initial treatment. Therefore, a large portion of patients are given consolidation or maintenance therapy with the intent to prolong progression-free survival (PFS) and overall survival (OS). Consolidation therapy is a short course of treatment to deepen the response to the initial therapy. Maintenance therapy aims to extend the period of disease quiescence with a longer course of a less-intensive regimen3.
At the time of analysis, lenalidomide was the only Food and Drug Administration (FDA)-approved drug in the United States (US) for maintenance therapy after ASCT in MM. Although generally well-tolerated, lenalidomide is associated with increased risk for neutropenia, thrombocytopenia, anemia, infections, thromboembolism, and second primary cancers4,5. Bortezomib is a first-in-class proteasome inhibitor that can lead to cell-cycle arrest and apoptosis6. Bortezomib-based regimens are widely used as induction therapy for MM7,8,9. Bortezomib has been used off label for consolidation or maintenance therapy after the initial treatment of MM, particularly for those with high-risk disease10. Unlike lenalidomide, the role of bortezomib in the consolidation or maintenance setting is less clear. Therefore, we conducted this meta-analysis of randomized controlled trials (RCTs) to examine the efficacy and safety of bortezomib-based regimens as consolidation or maintenance therapy in MM following induction therapy with or without ASCT. Bortezomib-based regimens were compared with regimens without bortezomib or observation.
Methods
Search strategy and selection criteria
PubMed, Web of Science, and Embase databases were searched for RCTs of bortezomib-based regimens (either single-agent or combination) as consolidation or maintenance therapy for MM through 31 August 2019. The keywords used for the literature search were “myeloma,” “bortezomib,” and “consolidation OR maintenance OR continuous therapy.” We also searched for abstracts presented at the American Society of Clinical Oncology or American Society of Hematology annual conferences. The references of relevant articles were manually searched to identify any additional eligible clinical trials. Studies eligible for inclusion met all the following criteria: (1) RCTs; (2) participants with MM; (3) studies with an intervention group given a bortezomib-containing regimen for consolidation/maintenance vs. a control group given either a bortezomib-free regimen or no consolidation/maintenance therapy; (4) studies reporting PFS and/or OS; and (5) studies published in English. Studies in both the transplantation setting and non-transplantation setting were included. Two investigators (S.Z. and Y.W.) independently conducted the literature search and screened the clinical trials. Discrepancies were resolved through consensus.
Study outcomes and data extraction
Efficacy outcomes included PFS and/or OS. Safety outcomes included treatment-related grade 3 or higher adverse events. For each included trial, we extracted the name of the first author, year of publication or conference presentation, study design, ASCT status, treatment setting (consolidation vs. maintenance), and study arm. We also retrieved the hazard ratio (HR) with 95% confidence interval (CI) of survival outcomes (PFS and/or OS) and grade ≥ 3 adverse event data. For studies that did not report HRs for survival outcomes, the authors were contacted for additional information.
Statistical analysis
Data synthesis was performed according to the guidelines for meta-analyses11. Pooled HRs of survival outcomes with 95% CI were calculated with the inverse variance method12 and pooled risk ratio (RR) of dichotomous safety data with 95% CI were computed with the Mantel–Haenszel and DerSimonian–Laird methods13,14. Study heterogeneity was assessed using the I2 statistic15. Forest plots were constructed for each meta-analysis to examine and display study-level data. The I2 statistic was used to describe the percentage of the variation across studies that is due to between-study differences rather than chance. Common cutoff points for low (I2 = 25%), moderate (I2 = 50%), and high degrees of heterogeneity (I2 = 75% or higher) were used15. Sensitivity analysis was performed by repeating the meta-analysis, excluding each individual study one at a time. Publication bias was evaluated by the funnel plot and Begg’s rank correlation test16. Analysis was conducted with MedCalc 16.2 (MedCalc Software, Ostend, Belgium) and Comprehensive Meta Analysis V3 (Biostat, Englewood, New Jersey, USA), using the random-effects model14. All statistical analyses were two-sided. A P-value < 0.05 was considered statistically significant, except for the heterogeneity analysis as mentioned above.
Results
Search results
We identified 4467 references from the initial database search and kept 12 RCTs for further review after initial screening. Basic research studies, review articles, case reports, retrospective studies, single-arm trials, non-randomized trials, studies not involving MM consolidation or maintenance therapy with bortezomib, duplicate reports, or publications not in English were excluded. Two RCTs of MM consolidation or maintenance therapy were excluded, as both study arms contained bortezomib17,18. Ten RCTs (in nine publications) were included in the final meta-analysis (Fig. 1).
Characteristics of included trials
Of the ten included RCTs19,20,21,22,23,24,25,26,27, there were nine phase III studies and one phase II study included in the analysis. Bortezomib-based regimens were administered as consolidation therapy in seven RCTs19,20,21,22,25,27 and as maintenance therapy in three RCTs23,24,26, following the initial therapy. Only one RCT was conducted in the non-transplantation setting24. The outcomes of the MMY3012 trial (NCT00416273) and MMY3013 trial (NCT00416208) were published as a pre-specified single dataset analysis on the combined data21. They were considered as one study in our meta-analysis. A total of 3147 patients were included: 1506 participants received bortezomib-based regimens, and 1641 received non-bortezomib-based regimens or no consolidation/maintenance (Table 1).
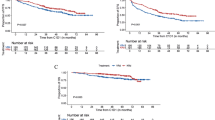
Survival outcomes for bortezomib-based consolidation therapy
Pooled data from the included trials showed that bortezomib-based consolidation therapy significantly improved PFS (HR = 0.77, 95% CI 0.68–0.88, P < 0.001), but not OS (HR = 0.98, 95% CI 0.78–1.24, P = 0.87) as compared with no consolidation or regimens without bortezomib (Fig. 2). Given that only one arm in Cavo’s study27 received bortezomib in induction and consolidation, we excluded this trial and repeated the meta-analysis to better assess the impact of bortezomib-containing regimen in the consolidation phase. This did not change the overall result and demonstrated improved PFS (HR = 0.79, 95% CI 0.68–0.90, P < 0.001), but not OS (HR = 1.01, 95% CI 0.79–1.29, P = 0.92). Of note, the OS data of the VCAT trial20 were not available for the meta-analysis.
(a) HRs for progression-free survival and (b) HRs for overall survival of bortezomib-based regimen vs. control. HRs for each trial are represented by squares, where the size of the square represents the weight of the trial in the meta-analysis and the horizontal line crossing the square represents the 95% confidence interval (CI). The diamonds represent the overall summary HR estimates and 95% CIs.
Survival outcomes for bortezomib-based maintenance therapy
Bortezomib-based maintenance therapy significantly increased PFS (HR = 0.72, 95% CI 0.55–0.95, P = 0.02) and OS (HR = 0.71, 95% CI 0.58–0.87, P = 0.001) as compared with no maintenance or regimens without bortezomib (Fig. 3). To assess the role of bortezomib-based maintenance therapy specifically in patients after ASCT, we excluded the trial involving transplant-ineligible patients24 and performed the meta-analysis again, which showed improved OS (HR = 0.72, 95% CI 0.54–0.96, P = 0.025) and a clear trend toward improved PFS (HR = 0.84, 95% CI 0.699–1.001, P = 0.052).
(a) HRs for progression-free survival and (b) HRs for overall survival of bortezomib-based regimen vs. control. HRs for each trial are represented by squares, where the size of the square represents the weight of the trial in the meta-analysis and the horizontal line crossing the square represents the 95% confidence interval (CI). The diamonds represent the overall summary HR estimates and 95% CIs.
Of note, one trial23 had three maintenance arms: bortezomib + thalidomide (VT) vs. thalidomide (T) vs. alfa-2b interferon (IFN). The pooled HRs shown above were based on the HRs between VT and T, as interferon is rarely used for MM in the current era. We also calculated the pooled HRs using the HRs between VT and IFN, and this did not change the overall conclusion (data not shown).
The meta-analysis was conducted in both MedCalc 16.2 and Comprehensive Meta Analysis V3 with same results.
Adverse events
Regarding safety, we calculated the pooled RRs for grade 3 or higher adverse events. Bortezomib-based consolidation/maintenance therapy induced a trend toward increased risk of grade ≥ 3 neurologic symptoms (RR = 1.59, 95% CI 0.94–2.69, P = 0.08), gastrointestinal symptoms (RR = 1.66, 95% CI 0.71–3.88, P = 0.24), and fatigue (RR = 2.10, 95% CI 0.83–5.30, P = 0.12) as compared with no consolidation/maintenance or regimens without bortezomib. However, these findings did not reach statistical significance (Table 2). Of note, subcutaneous bortezomib was used in only one study (in both the initial therapy and consolidation therapy)20 based on available data in these publications.
Heterogeneity analysis
We evaluated the heterogeneity of the studies using the I2 statistic. There was no clear evidence of statistical heterogeneity for the consolidation PFS (I2 = 0%), consolidation OS (I2 = 0%), or maintenance OS (I2 = 0%) data. There was moderate heterogeneity in the maintenance PFS (I2 = 71.47%) data. We repeated the meta-analysis for the survival outcomes using the fixed-effects model and the results did not change the overall conclusions of this study (data not shown).
Sensitivity analysis
Sensitivity analysis was carried out by removing one study at a time and repeating the meta-analysis to evaluate the stability of the results. The pooled HRs ranged from 0.75 to 0.80 for PFS and from 0.90 to 1.02 for OS in the consolidation setting. The pooled HRs ranged from 0.65 to 0.84 for PFS and from 0.70 to 0.72 for OS in the maintenance setting. The analysis showed that the results were overall stable.
Publication bias
Publication bias was assessed by formal tests16. The P-value for consolidation PFS and OS from the Begg’s rank correlation test was 0.71 and 1.0, respectively. The P-value for maintenance PFS and OS from the Begg’s rank correlation test was 1.0 and 0.30, respectively. The funnel plots are shown in Supplementary Fig. 1. These results demonstrate that there is no indication of significant publication bias among the included RCTs.
Discussion
Despite the introduction of several novel drugs and combination regimens in MM in recent years, maintaining remission after induction therapy is challenging and remains an unmet need. Consolidation and maintenance therapies are the strategies to prolong remission and survival in these patients. Our meta-analysis demonstrated that bortezomib-based maintenance significantly prolonged PFS and OS in MM patients after induction therapy in the absence or presence of ASCT. However, consolidation therapy with bortezomib-containing regimens only improved PFS but not OS. To our knowledge, our study is the first comprehensive meta-analysis evaluating the benefits and risks of bortezomib-based consolidation and maintenance therapy in patients with MM. By pooling data from multiple studies (even though the majority of which did not show conflicting results), our study provides a higher level of evidence regarding the role of bortezomib in consolidation and maintenance therapy for MM.
Bortezomib-based consolidation therapy
Consolidation therapy for MM is given as a short course of chemotherapy after the initial therapy, particularly in patients who have undergone ASCT. We identified seven RCTs (published in six articles)19,20,21,22,25,27 comparing consolidation with bortezomib-based regimens vs. non-bortezomib-based regimens or no consolidation. Consolidation was given after ASCT in all seven trials. The pooled analysis suggested delayed disease progression with bortezomib-based consolidation. However, the published RCTs evaluating the impact of consolidation with bortezomib-containing regimens on OS have reported different results. Studies led by Cavo et al.27, Einsele et al.21, and Stadtmauer et al.19 showed that consolidation with bortezomib-containing regimens led to a trend toward improved OS. In contrast, Mellqvist et al.25 showed the opposite. The contradictory effects on OS shown in Mellqvist’s study might be due to the fact that all patients were bortezomib-naive before consolidation and more patients in the control group received bortezomib-containing intensive therapy after first relapse (48/183 vs. 19/187)25. The study by Sezer et al.22 revealed similar effects on OS in the bortezomib arm compared with observation (HR = 1.01). Of note, none of these studies was statistically significant in terms of OS. The pooled HR of these studies was 0.98, indicating no OS advantage with bortezomib-based consolidation. The BMT CTN 0702 trial was the only study to properly isolate the effects of consolidation from maintenance. In this well-designed trial, consolidation with four cycles of bortezomib, lenalidomide, and dexamethasone prior to lenalidomide maintenance did not significantly improve OS19. One of the advantages of consolidation therapy is that treatment can be completed in a relatively short period of time. This could potentially decrease the risk of toxicities compared with maintenance therapy, in which more doses of bortezomib are given. However, the value of consolidation chemotherapy as a concept remains to be proven in MM and it needs studies such as the BMT CTN 0702 trial19, wherein the effect of consolidation is isolated. Consolidation therapy for MM is not the preferred approach in our clinical practice given the lack of OS benefit.
Bortezomib-based maintenance therapy
Maintenance therapy refers to a course of low-dose chemotherapy over a long period of time for patients with MM after induction therapy ± ASCT. The duration of maintenance therapy is usually 2–3 years or until disease progression, relapse, or unacceptable toxicity. Three RCTs evaluated the role of maintenance therapy with bortezomib-containing regimens in MM. Two studies were conducted in the transplant setting23,26 and one in transplant-ineligible patients24. The study by Palumbo et al.24 revealed that maintenance with bortezomib + thalidomide was superior to observation in terms of PFS and OS. Sonneveld et al.26 found that bortezomib led to significantly prolonged OS, but not PFS, as compared with thalidomide in the maintenance setting. Rosinol et al.23 compared three maintenance regimens: bortezomib + thalidomide vs. thalidomide vs. alfa-2b interferon and showed that bortezomib + thalidomide resulted in a trend toward improved PFS and OS. Our meta-analysis suggested that maintenance with bortezomib-based regimens prolonged both PFS and OS (pooled HR = 0.72 and 0.71, respectively).
It is not entirely clear why OS was improved with bortezomib-based regimens in the maintenance setting, but not in the consolidation setting. One can hypothesize that continuous suppression of myeloma cells with a bortezomib-containing regimen over a long period of time is needed to have a positive effect on OS. The flip side is that more exposure to bortezomib can potentially cause more side effects. It raises the question whether bortezomib-based maintenance for high-risk patients should be preferred over bortezomib-based consolidation given the lack of OS benefit with consolidation therapy. In our practice, we prefer maintenance therapy with bortezomib 1.3 mg/m2 every 2 weeks for certain high-risk patients. We typically treat patients for at least 2 years or till disease progression. The duration of treatment should also be based on toxicities, tolerance, and cost. Future studies are warranted to answer these questions.
Adverse events
Peripheral neuropathy is one of the dose-limiting toxicities of bortezomib and dose modification or discontinuation is often required in clinical practice. Our meta-analysis showed a trend of increased risk of grade ≥ 3 neurologic adverse events with bortezomib-based consolidation/maintenance. Bortezomib is also known to cause gastrointestinal symptoms, fatigue, and thrombocytopenia, etc. Although there is a trend toward increased grade ≥ 3 adverse events, our meta-analysis showed that bortezomib did not significantly increase the rate of these events. This may be partially explained by the fact that not all studies reported these adverse events, resulting in a relatively small patient number in the meta-analysis. Also, the route of administration (intravenous vs. subcutaneous) and the side effects resulting from induction therapy, pre-transplant high-dose chemotherapy, ASCT, and other medications (i.e., thalidomide) in the control arm during consolidation/maintenance might have confounded the results. Nevertheless, patients should be closely monitored for side effects during treatment.
Bortezomib vs. lenalidomide
Immunomodulatory drugs have been extensively studied in consolidation and maintenance therapy for MM. Posttransplant maintenance with lenalidomide is commonly utilized as it is the only US Food and Drug Administration-approved drug for this indication. In a meta-analysis of RCTs published in the Journal of Clinical Oncology, McCarthy et al.28 demonstrated both PFS benefit and OS benefit with lenalidomide maintenance after ASCT. However, its use has been limited by side effects including second primary neoplasms, less activity in high-risk disease, and high out-of-pocket costs to patients. In fact, some patients choose not to take oral lenalidomide for maintenance because of the financial burden its use imposes and prefer a non-oral medication. Here we show that bortezomib-based maintenance therapy improves both PFS and OS. Furthermore, bortezomib does not need dose adjustment in patients with renal impairment. Therefore, bortezomib may be an alternative option for certain patients.
Our colleagues at Mayo Clinic suggest a risk-adapted approach after initial therapy: lenalidomide maintenance is recommended for standard-risk disease, whereas bortezomib or carfilzomib-based maintenance is reserved for high-risk disease10. This approach is based on the finding that certain high-risk features, such as translocation between chromosomes 4 and 14 [t(4;14)], can be overcome by bortezomib29,30, and those high-risk patients would benefit more from a bortezomib-based regimen31,32. The role of bortezomib in patients with chromosome 17p deletion [del(17p)] is controversial. Although some studies suggested that bortezomib may negate the poor prognosis conferred by del(17p)7,33, this was not observed in a large study of 507 patients by Avet-Loiseau et al.30. We attempted to perform a subgroup analysis of high-risk patients; however, not enough data were presented in these published studies for such a meta-analysis. Nevertheless, high-quality evidence is needed to support these recommendations and further studies may identify which patient groups could derive the most benefit from bortezomib-based or lenalidomide-based therapy for consolidation and maintenance.
Limitations
Our study has a few limitations. Frist, the study is limited by a relatively small number of clinical trials, particularly for trials of maintenance therapy and trials in the non-transplantation setting. Second, abstracted data from published RCTs instead of individual patient data were used for the meta-analysis. Therefore, a subgroup analysis of high-risk patients could not be performed. Third, the RCTs had apparent heterogeneities in the patient population, study design, induction therapy regimen, bortezomib dose, schedule, and other factors. Some trials used bortezomib in the induction therapy and continued to use a bortezomib-based regimen for consolidation/maintenance. A second randomization would help delineate the role of a bortezomib-based regimen in the setting of consolidation/maintenance therapy. For example, Rosinol et al.23 did a second randomization before starting maintenance therapy. However, in the studies by Cavo et al.27 and Sonneveld et al.26, only one arm received bortezomib in the induction phase and consolidation/maintenance phase, and no randomization was performed before entering consolidation/maintenance, making it difficult to isolate the impact of bortezomib-containing regimens in consolidation/maintenance. In the consolidation setting, we repeated the meta-analysis by excluding Cavo’s trial and found similar outcomes. A similar analysis in the maintenance setting could not be performed because of the small number of studies. These considerations can potentially confound our results. However, it is unlikely that the survival differences seen are due to induction therapy, because clinical trials that solely evaluated differences in induction regimens have seldom shown an effect on OS. For example, the IFM 2005–01 trial compared the efficacy of bortezomib + dexamethasone vs. vincristine + doxorubicin + dexamethasone as induction therapy before ASCT, but it failed to demonstrate a significant OS benefit34. Thus, the effect on OS shown in the meta-analysis is likely due to maintenance therapy. More clinical trials in this area are needed to confirm our results. Given the heterogeneity of the included trials, we decided to use the random-effects model to conduct the meta-analysis of survival outcomes. Caution should be used when interpreting results from this meta-analysis.
Conclusion
This meta-analysis showed that consolidation therapy with bortezomib-containing regimens only improved PFS but not OS in patients with MM. Despite the limitations of this analysis, we have some suggestion of the benefit of bortezomib-based maintenance therapy, particularly in high-risk patients. Further research is warranted to assess the role of bortezomib in maintenance therapy for MM. Given that different patient groups may respond differently to a specific regimen, we believe a risk-adapted approach should be used in future studies to tailor consolidation and maintenance therapy based on disease risks, regimens used in induction therapy, and minimal residual disease status.
References
Kazandjian, D. Multiple myeloma epidemiology and survival: a unique malignancy. Semin. Oncol. 43, 676–681 (2016).
Kumar, S. K. et al. Multiple myeloma. Nat. Rev. Dis. Primers 3, 17046 (2017).
Lipe, B., Vukas, R. & Mikhael, J. The role of maintenance therapy in multiple myeloma. Blood Cancer J. 6, e485 (2016).
McCarthy, P. L. et al. Lenalidomide after stem-cell transplantation for multiple myeloma. N. Engl. J. Med. 366, 1770–1781 (2012).
Attal, M. et al. Lenalidomide maintenance after stem-cell transplantation for multiple myeloma. N. Engl. J. Med. 366, 1782–1791 (2012).
Richardson, P. G., Hideshima, T. & Anderson, K. C. Bortezomib (PS-341): a novel, first-in-class proteasome inhibitor for the treatment of multiple myeloma and other cancers. Cancer Control. 10, 361–369 (2003).
San Miguel, J. F. et al. Bortezomib plus melphalan and prednisone for initial treatment of multiple myeloma. N. Engl. J. Med. 359, 906–917 (2008).
Durie, B. G. et al. Bortezomib with lenalidomide and dexamethasone versus lenalidomide and dexamethasone alone in patients with newly diagnosed myeloma without intent for immediate autologous stem-cell transplant (SWOG S0777): a randomised, open-label, phase 3 trial. Lancet 389, 519–527 (2017).
Attal, M. et al. Lenalidomide, Bortezomib, and dexamethasone with transplantation for myeloma. N. Engl. J. Med. 376, 1311–1320 (2017).
Mayo Stratification of Myeloma and Risk-Adapted Therapy (mSMART). https://www.msmart.org/mm-treatment-guidelines. Accessed 31 Dec 2018.
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G. & Group, P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 339, b2535 (2009).
Borenstein, M., Hedges, L. V., Higgins, J. P. T. & Rothstein, H. R. Introduction to Meta‐Analysis (Wiley, 2009).
Mantel, N. & Haenszel, W. Statistical aspects of the analysis of data from retrospective studies of disease. J. Natl Cancer Inst. 22, 719–748 (1959).
DerSimonian, R. & Laird, N. Meta-analysis in clinical trials. Control Clin. Trials 7, 177–188 (1986).
Higgins, J. P. & Thompson, S. G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 21, 1539–1558 (2002).
Begg, C. B. & Mazumdar, M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 50, 1088–1101 (1994).
Jacobus, S. J. et al. Randomized phase III trial of consolidation therapy with bortezomib-lenalidomide-Dexamethasone (VRd) vs bortezomib-dexamethasone (Vd) for patients with multiple myeloma who have completed a dexamethasone based induction regimen. Blood Cancer J. 6, e448 (2016).
Mateos, M.-V. et al. Bortezomib, melphalan, and prednisone versus bortezomib, thalidomide, and prednisone as induction therapy followed by maintenance treatment with bortezomib and thalidomide versus bortezomib and prednisone in elderly patients with untreated multiple myeloma: a randomised trial. Lancet Oncol. 11, 934–941 (2010).
Stadtmauer, E. A. et al. Autologous transplantation, consolidation, and maintenance therapy in multiple myeloma: results of the BMT CTN 0702 Trial. J. Clin. Oncol. 37, 589–597 (2019).
Horvath, N. et al. Phase 3 study of subcutaneous bortezomib, thalidomide, and prednisolone consolidation after subcutaneous bortezomib-based induction and autologous stem cell transplantation in patients with previously untreated multiple myeloma: the VCAT study. Leuk. Lymphoma 60, 2122–2133 (2019).
Einsele, H. et al. Response-adapted consolidation with bortezomib after ASCT improves progression-free survival in newly diagnosed multiple myeloma. Leukemia 31, 1463–1466 (2017).
Sezer, O. et al. Effects of single-agent bortezomib as post-transplant consolidation therapy on multiple myeloma-related bone disease: a randomized phase II study. Br. J. Haematol. 178, 61–71 (2017).
Rosinol, L. et al. Bortezomib and thalidomide maintenance after stem cell transplantation for multiple myeloma: a PETHEMA/GEM trial. Leukemia. 31, 1922–1927 (2017).
Palumbo, A. et al. Bortezomib-melphalan-prednisone-thalidomide followed by maintenance with bortezomib-thalidomide compared with bortezomib-melphalan-prednisone for initial treatment of multiple myeloma: updated follow-up and improved survival. J. Clin. Oncol. 32, 634–640 (2014).
Mellqvist, U. H. et al. Bortezomib consolidation after autologous stem cell transplantation in multiple myeloma: a Nordic Myeloma Study Group randomized phase 3 trial. Blood. 121, 4647–4654 (2013).
Sonneveld, P. et al. Bortezomib induction and maintenance treatment in patients with newly diagnosed multiple myeloma: results of the randomized phase III HOVON-65/ GMMG-HD4 trial. J. Clin. Oncol. 30, 2946–2955 (2012).
Cavo, M. et al. Bortezomib-thalidomide-dexamethasone is superior to thalidomide-dexamethasone as consolidation therapy after autologous hematopoietic stem cell transplantation in patients with newly diagnosed multiple myeloma. Blood. 120, 9–19 (2012).
McCarthy, P. L. et al. Lenalidomide maintenance after autologous stem-cell transplantation in newly diagnosed multiple myeloma: a meta-analysis. J Clin Oncol. 35, 3279–3289 (2017).
Cavo, M. et al. Bortezomib with thalidomide plus dexamethasone compared with thalidomide plus dexamethasone as induction therapy before, and consolidation therapy after, double autologous stem-cell transplantation in newly diagnosed multiple myeloma: a randomised phase 3 study. Lancet. 376, 2075–2085 (2010).
Avet-Loiseau, H. et al. Bortezomib plus dexamethasone induction improves outcome of patients with t(4;14) myeloma but not outcome of patients with del(17p). J. Clin. Oncol. 28, 4630–4634 (2010).
Mikhael, J. R. et al. Management of newly diagnosed symptomatic multiple myeloma: updated Mayo Stratification of Myeloma and Risk-Adapted Therapy (mSMART) consensus guidelines 2013. Mayo Clin. Proc. 88, 360–376 (2013).
Sengsayadeth, S., Malard, F., Savani, B. N., Garderet, L. & Mohty, M. Posttransplant maintenance therapy in multiple myeloma: the changing landscape. Blood Cancer J. 7, e545 (2017).
Neben, K. et al. Administration of bortezomib before and after autologous stem cell transplantation improves outcome in multiple myeloma patients with deletion 17p. Blood. 119, 940–948 (2012).
Harousseau, J. L. et al. Bortezomib plus dexamethasone is superior to vincristine plus doxorubicin plus dexamethasone as induction treatment prior to autologous stem-cell transplantation in newly diagnosed multiple myeloma: results of the IFM 2005-01 phase III trial. J. Clin. Oncol. 28, 4621–4629 (2010).
Sonneveld, P. et al. Bortezomib induction and maintenance treatment improves survival in patients with newly diagnosed multiple myeloma: extended follow-up of the HOVON-65/GMMG-HD4 Trial. Blood. 122, 404–404 (2013).
Goldschmidt, H. et al. Bortezomib before and after high-dose therapy in myeloma: long-term results from the phase III HOVON-65/GMMG-HD4 trial. Leukemia. 32, 383–390 (2018).
Acknowledgements
We thank Drs. Pieter Sonneveld, Ulf-Henrik Mellqvist, Christian Straka, Hermann Einsele, and Laura Rosinol for providing additional data on their clinical trials; Dr. Lin Zhang for her suggestion on statistical analysis; and Dr. Yvonne Datta and Michael Franklin for reviewing the manuscript. This work was done with no funding support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Michael Wang made the following disclosures: research grants, consulting/advisory board, and honoraria—Janssen and Acerta Pharma; research grants and consulting/advisory board—Pharmacyclics, AstraZeneca, Celgene, Juno Therapeutics, Loxo Oncology, Kite Pharma, and BioInvent; research grants—BeiGene, VelosBio, and Aviara; consulting/advisory board—Pulse Biosciences and Guidepoint Global; consulting/advisory board and stock—MoreHealth; honoraria—OMI, Physicians Education Resources, and Oncology News, outside the submitted work. Dr. Veronika Bachanova reported non-financial support from ArticulateScience, grants from Novartis, grants from GT Biopharma, personal fees from Seattle Genetics, Kite Pharma, and Zymogen, outside the submitted work. No other disclosures were reported.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhang, S., Kulkarni, A.A., Xu, B. et al. Bortezomib-based consolidation or maintenance therapy for multiple myeloma: a meta-analysis. Blood Cancer J. 10, 33 (2020). https://doi.org/10.1038/s41408-020-0298-1
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41408-020-0298-1
This article is cited by
-
Myasthenia gravis: the changing treatment landscape in the era of molecular therapies
Nature Reviews Neurology (2024)
-
Budget Impact Analysis of Idecabtagene Vicleucel for the Treatment of Adult Patients with Relapsed or Refractory Multiple Myeloma in the US
Clinical Drug Investigation (2022)
-
The role of novel agents for consolidation after autologous transplantation in newly diagnosed multiple myeloma: a systematic review
Annals of Hematology (2021)