Abstract
Purpose
The purpose of this study was to examine the predictive value concerning clinical outcome and implant survival, as well as the accuracy of individual tests of a recently published radiographic decision aid for unicondylar knee arthroplasty indication findings.
Methods
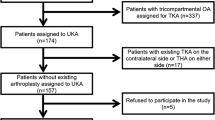
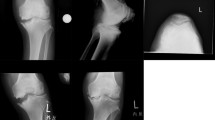
In the retrospective part of the study, 98 consecutive patients who had undergone unicondylar knee arthroplasty (Phase 3 Oxford medial UKA) were included, using revision questionnaires, as well as the Forgotten Joint Score-12 (FJS-12) and Knee Osteoarthritis Outcome Score (KOOS) and analysed for suitability of the radiographic decision aid. Inappropriate and appropriate indications were then compared concerning the clinical outcome and implant survival. The prospective part of the study assessed the accuracy of the decision aid's radiographic tests (varus and valgus stress views, true lateral view and skyline view), and included 90 patients. Definition as appropriate for UKA procedure included medial bone-on-bone situation in varus stress views, full-thickness lateral cartilage and functional medial collateral ligament in valgus stress views, functional anterior cruciate ligament (ACL) in true lateral views and absence of lateral facet osteoarthritis with bone loss in skyline views. Pre-operative radiographic assessment with respect to the decision aid was then compared with intraoperative articular conditions. The clinical outcome was analysed using non-parametric tests (Mann–Whitney U), and revision rates were compared using the Fisher’s exact test. Accuracy assessment included calculations of the sensitivity, specificity, negative predictive value and positive predictive value. A p value < 0.05 was considered statistically significant.
Results
Appropriate unicondylar knee arthroplasty with respect to the decision aid showed a significantly lower revision rate compared to inappropriate unicondylar knee arthroplasty (7.3% vs. 50.0%, p < 0.0001), as well as higher clinical outcome scores (FJS-12: 53.13 vs. 31.25, p = 0.041 and KOOS-QDL: 68.75 vs. 50.0, p = 0.036). The overall sensitivity (70.1%) and specificity (76.2%) for the radiographic decision aid was comparably low, which was essentially based on false negative cases (22.7%) regarding medial bone-to-bone conditions.
Conclusion
The radiographic decision aid is a helpful tool to predict clinical outcome and implant survival of mobile-bearing unicondylar knee arthroplasty. Strict use of the radiographic decision aid may lead to increased exclusion of appropriate patients with unicondylar knee arthroplasty implantation.


Similar content being viewed by others
Abbreviations
- ACL:
-
Anterior cruciate ligament
- FTCL:
-
Full-thickness cartilage loss
- KOOS:
-
Knee Osteoarthritis Outcome Score
- KSS:
-
Knee Society Score
- LJ:
-
List JP
- MCL:
-
Medial collateral ligament
- MRI:
-
Magnetic resonance imaging
- NPV:
-
Negative predictive value
- PPV:
-
Positive predictive value
- PTCL:
-
Partial-thickness cartilage loss
- SONK:
-
Spontaneous osteonecrosis of the knee
- TKA:
-
Total knee arthroplasty
- UKA:
-
Unicondylar knee arthroplasty
References
Alnachoukati OK, Barrington JW, Berend KR, Kolczun MC, Emerson RH, Lombardi AV Jr, Mauerhan DR (2018) Eight hundred twenty-five medial mobile-bearing unicompartmental knee arthroplasties: the first 10-year us multi-center survival analysis. J Arthroplasty 33:677–683. https://doi.org/10.1016/j.arth.2017.10.015
Berend KR, Berend ME, Dalury DF, Argenson JN, Dodd CA, Scott RD (2015) Consensus statement on indications and contraindications for medial unicompartmental knee arthroplasty. J Surg Orthop Adv 24:252–256
Bergeson AG, Berend KR, Lombardi AV Jr, Hurst JM, Morris MJ, Sneller MA (2013) Medial mobile bearing unicompartmental knee arthroplasty: early survivorship and analysis of failures in 1000 consecutive cases. J Arthroplasty 28:172–175. https://doi.org/10.1016/j.arth.2013.01.005
Hamilton TW, Pandit HG, Inabathula A, Ostlere SJ, Jenkins C, Mellon SJ, Dodd CA, Murray DW (2017) Unsatisfactory outcomes following unicompartmental knee arthroplasty in patients with partial thickness cartilage loss: a medium-term follow-up. Bone Joint J 99-B:475–482. https://doi.org/10.1302/0301-620X.99B4.BJJ-2016-1061.R1
Hamilton TW, Pandit HG, Lombardi AV, Adams JB, Oosthuizen CR, Clave A, Dodd CA, Berend KR, Murray DW (2016) Radiological decision aid to determine suitability for medial unicompartmental knee arthroplasty: development and preliminary validation. Bone Joint J 98-B:3–10. https://doi.org/10.1302/0301-620X.98B10.BJJ-2016-0432.R1
Kendrick BJ, Rout R, Bottomley NJ, Pandit H, Gill HS, Price AJ, Dodd CA, Murray DW (2010) The implications of damage to the lateral femoral condyle on medial unicompartmental knee replacement. J Bone Joint Surg Br 92:374–379. https://doi.org/10.1302/0301-620X.92B3.23561
Kleeblad LJ, van der List JP, Zuiderbaan HA, Pearle AD (2018) Larger range of motion and increased return to activity, but higher revision rates following unicompartmental versus total knee arthroplasty in patients under 65: a systematic review. Knee Surg Sports Traumatol Arthrosc 26:1811–1822. https://doi.org/10.1007/s00167-017-4817-y
Koskinen E, Paavolainen P, Eskelinen A, Pulkkinen P, Remes V (2007) Unicondylar knee replacement for primary osteoarthritis: a prospective follow-up study of 1,819 patients from the Finnish Arthroplasty Register. Acta Orthop 78:128–135. https://doi.org/10.1080/17453670610013538
Kuipers BM, Kollen BJ, Bots PC, Burger BJ, van Raay JJ, Tulp NJ, Verheyen CC (2010) Factors associated with reduced early survival in the Oxford phase III medial unicompartment knee replacement. Knee 17:48–52. https://doi.org/10.1016/j.knee.2009.07.005
Kwon HM, Kang KT, Kim JH, Park KK (2019) Medial unicompartmental knee arthroplasty to patients with a ligamentous deficiency can cause biomechanically poor outcomes. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-019-05636-7
Liddle AD, Judge A, Pandit H, Murray DW (2014) Adverse outcomes after total and unicompartmental knee replacement in 101,330 matched patients: a study of data from the National Joint Registry for England and Wales. Lancet 384:1437–1445. https://doi.org/10.1016/S0140-6736(14)60419-0
Liddle AD, Pandit H, Judge A, Murray DW (2015) Patient-reported outcomes after total and unicompartmental knee arthroplasty: a study of 14,076 matched patients from the National Joint Registry for England and Wales. Bone Joint J 97-B:793–801. https://doi.org/10.1302/0301-620X.97B6.35155
Liow MH, Tsai TY, Dimitriou D, Li G, Kwon YM (2016) Does 3-dimensional in vivo component rotation affect clinical outcomes in unicompartmental knee arthroplasty? J Arthroplasty 31:2167–2172. https://doi.org/10.1016/j.arth.2016.03.003
Luscombe KL, Lim J, Jones PW, White SH (2007) Minimally invasive Oxford medial unicompartmental knee arthroplasty. A note of caution! Int Orthop 31:321–324. https://doi.org/10.1007/s00264-006-0202-z
Maier MW, Kuhs F, Streit MR, Schuhmacher P, Walker T, Ewerbeck V, Gotterbarm T (2015) Unicompartmental knee arthroplasty in patients with full versus partial thickness cartilage loss (PTCL): equal in clinical outcome but with higher reoperation rate for patients with PTCL. Arch Orthop Trauma Surg 135:1169–1175. https://doi.org/10.1007/s00402-015-2236-4
Mohammad HR, Strickland L, Hamilton TW, Murray DW (2018) Long-term outcomes of over 8,000 medial Oxford Phase 3 Unicompartmental Knees-a systematic review. Acta Orthop 89:101–107. https://doi.org/10.1080/17453674.2017.1367577
Morris MJ, Molli RG, Berend KR, Lombardi AV Jr (2013) Mortality and perioperative complications after unicompartmental knee arthroplasty. Knee 20:218–220. https://doi.org/10.1016/j.knee.2012.10.019
Niinimaki TT, Murray DW, Partanen J, Pajala A, Leppilahti JI (2011) Unicompartmental knee arthroplasties implanted for osteoarthritis with partial loss of joint space have high re-operation rates. Knee 18:432–435. https://doi.org/10.1016/j.knee.2010.08.004
Pandit H, Gulati A, Jenkins C, Barker K, Price AJ, Dodd CA, Murray DW (2011) Unicompartmental knee replacement for patients with partial thickness cartilage loss in the affected compartment. Knee 18:168–171. https://doi.org/10.1016/j.knee.2010.05.003
Pandit H, Hamilton TW, Jenkins C, Mellon SJ, Dodd CA, Murray DW (2015) The clinical outcome of minimally invasive Phase 3 Oxford unicompartmental knee arthroplasty: a 15-year follow-up of 1000 UKAs. Bone Joint J 97-B:1493–1500. https://doi.org/10.1302/0301-620X.97B11.35634
Price AJ, Webb J, Topf H, Dodd CA, Goodfellow JW, Murray DW, Oxford H, Knee G (2001) Rapid recovery after oxford unicompartmental arthroplasty through a short incision. J Arthroplasty 16:970–976. https://doi.org/10.1054/arth.2001.25552
Tinius M, Hepp P, Becker R (2012) Combined unicompartmental knee arthroplasty and anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 20:81–87. https://doi.org/10.1007/s00167-011-1528-7
Vorlat P, Putzeys G, Cottenie D, Van Isacker T, Pouliart N, Handelberg F, Casteleyn PP, Gheysen F, Verdonk R (2006) The Oxford unicompartmental knee prosthesis: an independent 10-year survival analysis. Knee Surg Sports Traumatol Arthrosc 14:40–45. https://doi.org/10.1007/s00167-005-0621-1
Walker T, Hetto P, Bruckner T, Gotterbarm T, Merle C, Panzram B, Innmann MM, Moradi B (2019) Minimally invasive Oxford unicompartmental knee arthroplasty ensures excellent functional outcome and high survivorship in the long term. Knee Surg Sports Traumatol Arthrosc 27:1658–1664. https://doi.org/10.1007/s00167-018-5299-2
Zumbrunn T, Schutz P, von Knoch F, Preiss S, List R, Ferguson SJ (2019) Medial unicompartmental knee arthroplasty in ACL-deficient knees is a viable treatment option: in vivo kinematic evaluation using a moving fluoroscope. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-019-05594-0
Acknowledgements
L. Tuecking has nothing to disclose. Dr. Savov has nothing to disclose. PD Dr. Ettinger reports grants and personal fees from Smith & Nephew, personal fees from Stryker, Grants and personal fees from Waldemar Link Gmbh, grants and personal fees from Medacta, outside the submitted work. Prof. Dr. Windhagen reports personal fees from Aesculap, personal fees from Stryker, personal fees from Medacta, outside the submitted work.
Funding
No external source of funding was used for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
LT, PS, TR, HW and ME declare that they have no conflict of interest.
Ethical approval
This study was approved by the local ethics committee (Nr. 3299–2016/Nr. 3306–2016).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tuecking, LR., Savov, P., Richter, T. et al. Clinical validation and accuracy testing of a radiographic decision aid for unicondylar knee arthroplasty patient selection in midterm follow-up. Knee Surg Sports Traumatol Arthrosc 28, 2082–2090 (2020). https://doi.org/10.1007/s00167-020-05912-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-05912-x