Abstract
Purpose
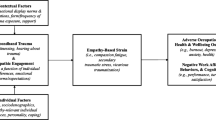
This study aimed to investigate the level of fertility related quality of life (FertiQoL) in women with recurrent pregnancy loss (RPL), and to further examine moderated mediation effects of dispositional mindfulness and negative emotions on the relationship between perceived stress and FertiQoL.
Methods
A cross-sectional study was conducted with 262 participants recruited from the infertility outpatient clinics. A self-administered, structured questionnaire including the Simplified Chinese version of FertiQoL tool, the Perceived Stress Scale-10 (PSS-10), the Chinese Version of the Hospital Anxiety and Depression Scale (HADS), and the Mindfulness Attention Awareness Scale (MAAS) was used to collect information in this research. The mediation model and moderated mediation model were conducted using the PROCESS macro for SPSS.
Results
The mean score of Core FertiQoL was 64.59 (SD = 14.76) among women with RPL. Mediation analysis revealed that the association between perceived stress and FertiQoL was partially mediated by negative emotions (indirect effect = − 0.194 for anxiety, and − 0.151 for depression, all P < 0.001). Moderated mediation analysis indicated that the indirect effects of perceived stress on FertiQoL through negative emotions were significantly moderated by dispositional mindfulness. Specifically, the indirect effects of perceived stress on FertiQoL through negative emotions decreased were significant as dispositional mindfulness levels increased.
Conclusion
Overall, women with RPL experienced poor FertiQoL. The Moderated mediation model provides a better understanding of how perceived stress, negative emotions and dispositional mindfulness work together to affect FertiQoL. Interventions aiming to improve FertiQoL in women with RPL should consider targeting these aspects.






Similar content being viewed by others
References
Practice Committee of the American Society for Reproductive Medicine. (2013). Definitions of infertility and recurrent pregnancy loss: a committee opinion. Fertility and Sterility,99(1), 63. https://doi.org/10.1016/j.fertnstert.2012.09.023.
Bender Atik, R., Christiansen, O. B., Elson, J., Kolte, A. M., Lewis, S., Middeldorp, S., et al. (2018). ESHRE guideline: recurrent pregnancy loss. Human Reproductive Open. https://doi.org/10.1093/hropen/hoy004.
Rai, R., & Regan, L. (2006). Recurrent miscarriage. The Lancet,368(9535), 601–611.
Bellhouse, C., Temple-Smith, M., Watson, S., & Bilardi, J. (2019). "The loss was traumatic.. some healthcare providers added to that": Women's experiences of miscarriage. Women Birth,32(2), 137–146. https://doi.org/10.1016/j.wombi.2018.06.006.
Abbaspoor, Z., Razmju, P. S., & Hekmat, K. (2016). Relation between quality of life and mental health in pregnant women with prior pregnancy loss. Journal of Obstetrics and Gynaecology Research,42(10), 1290–1296. https://doi.org/10.1111/jog.13061.
He, L., Wang, T., Xu, H., Chen, C., Liu, Z., Kang, X., et al. (2019). Prevalence of depression and anxiety in women with recurrent pregnancy loss and the associated risk factors. Archives of Gynecology and Obstetrics,300(4), 1061–1066. https://doi.org/10.1007/s00404-019-05264-z.
Lok, I. H., & Neugebauer, R. (2007). Psychological morbidity following miscarriage. Best Practice & Research Clinical Obstetrics & Gynaecology,21(2), 229–247.
Farren, J., Mitchell-Jones, N., Verbakel, J. Y., Timmerman, D., Jalmbrant, M., & Bourne, T. (2018). The psychological impact of early pregnancy loss. Human Reproductive Update,24(6), 731–749. https://doi.org/10.1093/humupd/dmy025.
Tavoli, Z., Mohammadi, M., Tavoli, A., Moini, A., Effatpanah, M., Khedmat, L., et al. (2018). Quality of life and psychological distress in women with recurrent miscarriage: a comparative study. Health and Quality of Life Outcomes,16(1), 150.
Coughlan, C., Walters, S., Ledger, W., & Li, T. C. (2014). A comparison of psychological stress among women with and without reproductive failure. International Journal of Gynecology & Obstetrics,124(2), 143–147.
Seo, E. J., Ahn, J. A., Hayman, L. L., & Kim, C. J. (2018). The association between perceived stress and quality of life in university students: The parallel mediating role of depressive symptoms and health-promoting behaviors. Asian Nursing Research,12(3), 190–196. https://doi.org/10.1016/j.anr.2018.08.001.
Yang, J., Guo, J., Tang, Y., Huang, L., Wiley, J., Zhou, Z., et al. (2019). The mediating effect of coping styles and self-efficacy between perceived stress and satisfaction with QOL in Chinese adolescents with type 1 diabetes. Journal of Advanced Nursing,75(7), 1439–1449. https://doi.org/10.1111/jan.13933.
Zhang, H., Zhang, Q., Gao, T., Kong, Y., Qin, Z., Hu, Y., et al. (2019). Relations between stress and quality of life among women in late pregnancy: The parallel mediating role of depressive symptoms and sleep quality. Psychiatry Investigation,16(5), 363–369. https://doi.org/10.30773/pi.2019.02.14.
Cheng, C. Y., Stevenson, E. L., Yang, C. T., & Liou, S. R. (2018). Stress and quality of life for Taiwanese women who underwent infertility treatment. Journal of Obstetric, Gynecologic, and Neonatal Nursing,47(4), 498–508. https://doi.org/10.1016/j.jogn.2018.03.005.
Gana, K., & Jakubowska, S. (2016). Relationship between infertility-related stress and emotional distress and marital satisfaction. Journal of Health Psychology,21(6), 1043–1054. https://doi.org/10.1177/1359105314544990.
Kim, J. H., Shin, H. S., & Yun, E. K. (2018). A dyadic approach to infertility stress, marital adjustment, and depression on quality of life in infertile couples. Journal of Holistic Nursing,36(1), 6–14. https://doi.org/10.1177/0898010116675987.
Shahraki, Z., Ghajarzadeh, M., & Ganjali, M. (2019). Depression, anxiety, quality of life and sexual dysfunction in Zabol women with infertility. Maedica (Buchar),14(2), 131–134. https://doi.org/10.26574/maedica.2019.14.2.131.
Shahraki, Z., Tanha, F. D., & Ghajarzadeh, M. (2018). Depression, sexual dysfunction and sexual quality of life in women with infertility. BMC Womens Health,18(1), 92. https://doi.org/10.1186/s12905-018-0584-2.
Kolte, A. M., Olsen, L. R., Christiansen, O. B., Schmidt, L., & Nielsen, H. S. (2019). Pregnancy outcomes after recurrent pregnancy loss: A longitudinal cohort study on stress and depression. Reprod Biomed Online,38(4), 599–605. https://doi.org/10.1016/j.rbmo.2018.12.006.
Kabat-Zinn, J. (2003). Mindfulness-based interventions in context: Past, present, and future. Clinical Psychology: Science and Practice,10(2), 144–156. https://doi.org/10.1093/clipsy.bpg016.
Brown, K. W., & Ryan, R. M. (2003). The benefits of being present: mindfulness and its role in psychological well-being. Journal of Personality and Social Psychology,84(4), 822–848. https://doi.org/10.1037/0022-3514.84.4.822.
Hicks, A., Phillips, K., Siwik, C., Salmon, P., Litvan, I., Jablonski, M. E., et al. (2019). The role of dispositional mindfulness in a stress-health pathway among Parkinson's disease patients and caregiving partners. Quality of Life Research,28(10), 2705–2716. https://doi.org/10.1007/s11136-019-02217-6.
Sala, M., Rochefort, C., Lui, P. P., & Baldwin, A. S. (2019). Trait mindfulness and health behaviours: A meta-analysis. Health Psychology Review. https://doi.org/10.1080/17437199.2019.1650290.
Chiesa, A., Serretti, A., & Jakobsen, J. C. (2013). Mindfulness: top-down or bottom-up emotion regulation strategy? Clinical Psychology Review,33(1), 82–96. https://doi.org/10.1016/j.cpr.2012.10.006.
Britton, W. B., Shahar, B., Szepsenwol, O., & Jacobs, W. J. (2012). Mindfulness-based cognitive therapy improves emotional reactivity to social stress: results from a randomized controlled trial. Behavior Therapy,43(2), 365–380. https://doi.org/10.1016/j.beth.2011.08.006.
Feldman, G., Lavalle, J., Gildawie, K., & Greeson, J. M. (2016). Dispositional mindfulness uncouples physiological and emotional reactivity to a laboratory stressor and emotional reactivity to executive functioning lapses in daily life. Mindfulness (N Y),7(2), 527–541. https://doi.org/10.1007/s12671-015-0487-3.
Mascaro, J. S., Rilling, J. K., Negi, L. T., & Raison, C. L. (2013). Pre-existing brain function predicts subsequent practice of mindfulness and compassion meditation. Neuroimage,69, 35–42. https://doi.org/10.1016/j.neuroimage.2012.12.021.
Way, B. M., Creswell, J. D., Eisenberger, N. I., & Lieberman, M. D. (2010). Dispositional mindfulness and depressive symptomatology: Correlations with limbic and self-referential neural activity during rest. Emotion,10(1), 12–24.
Bergin, A. J., & Pakenham, K. I. (2016). The stress-buffering role of mindfulness in the relationship between perceived stress and psychological adjustment. Mindfulness,7(4), 928–939.
Daubenmier, J., Hayden, D., Chang, V., & Epel, E. (2014). It's not what you think, it's how you relate to it: Dispositional mindfulness moderates the relationship between psychological distress and the cortisol awakening response. Psychoneuroendocrinology,48, 11–18. https://doi.org/10.1016/j.psyneuen.2014.05.012.
Lucas-Thompson, R. G., Miller, R. L., Seiter, N. S., & Prince, M. A. (2019). Dispositional mindfulness predicts cortisol, cardiovascular, and psychological stress responses in adolescence. Psychoneuroendocrinology,110, 104405. https://doi.org/10.1016/j.psyneuen.2019.104405.
Bravo, A. J., Pearson, M. R., Stevens, L. E., & Henson, J. M. (2016). Depressive symptoms and alcohol-related problems among college students: A moderated-mediated model of mindfulness and drinking to Cope. Journal of Studies on Alcohol and Drugs,77(4), 661–666. https://doi.org/10.15288/jsad.2016.77.661.
Su, M. R., & Shum, K. K. (2019). The moderating effect of mindfulness on the mediated relation between critical thinking and psychological distress via cognitive distortions among adolescents. Frontiers in Psychology,10, 1455. https://doi.org/10.3389/fpsyg.2019.01455.
Sugiura, Y., & Sugiura, T. (2018). Mindfulness as a moderator in the relation between income and psychological well-being. Frontiers in Psychology,9, 1477. https://doi.org/10.3389/fpsyg.2018.01477.
Rudaz, M., Ledermann, T., & Grzywacz, J. G. (2018). Spiritual coping, perceived growth, and the moderating role of spiritual mindfulness in cancer survivors. Journal of Psychosocial Oncology,36(5), 609–623. https://doi.org/10.1080/07347332.2018.1464091.
Zhong, M., Goh, P. H., Li, D., Bao, J., & Xu, W. (2017). Dispositional mindfulness as a moderator between perceived stress and psychological symptoms in Chinese digestive tract cancer patients. Journal of Health Psychology. https://doi.org/10.1177/1359105317736576.
Skoranski, A., Kelly, N. R., Radin, R. M., Thompson, K. A., Galescu, O., Demidowich, A. P., et al. (2018). Relationship of mindfulness to distress and cortisol response in adolescent girls at-risk for type 2 diabetes. Journal of Child and Family Studies,27(7), 2254–2264. https://doi.org/10.1007/s10826-018-1065-9.
Brown, K. W., Weinstein, N., & Creswell, J. D. (2012). Trait mindfulness modulates neuroendocrine and affective responses to social evaluative threat. Psychoneuroendocrinology,37(12), 2037–2041. https://doi.org/10.1016/j.psyneuen.2012.04.003.
Faul, F., Erdfelder, E., Buchner, A., & Lang, A. G. (2009). Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behavior Research Methods,41(4), 1149–1160. https://doi.org/10.3758/brm.41.4.1149.
Cohen, S., Kamarck, T., & Mermelstein, R. (1983). A global measure of perceived stress. Journal of Health and Social Behavior,24(4), 385–396.
Leung, D. Y., Lam, T. H., & Chan, S. S. (2010). Three versions of Perceived Stress Scale: Validation in a sample of Chinese cardiac patients who smoke. BMC Public Health,10, 513. https://doi.org/10.1186/1471-2458-10-513.
Lu, W., Bian, Q., Wang, W., Wu, X., Wang, Z., & Zhao, M. (2017). Chinese version of the Perceived Stress Scale-10: A psychometric study in Chinese university students. PLoS ONE,12(12), e0189543. https://doi.org/10.1371/journal.pone.0189543.
Deng, Y.-Q., Li, S., Tang, Y.-Y., Zhu, L.-H., Ryan, R., & Brown, K. (2012). Psychometric properties of the Chinese translation of the mindful attention awareness scale (MAAS). Mindfulness (N Y),3(1), 10–14.
Lianchao, A., & Tingting, M. (2020). Mindfulness, rumination and post-traumatic growth in a Chinese cancer sample. Psychol Health Med,25(1), 37–44. https://doi.org/10.1080/13548506.2019.1612079.
Chan, Y.-F., Leung, D. Y. P., Fong, D. Y. T., Leung, C.-M., & Lee, A. M. (2010). Psychometric evaluation of the Hospital Anxiety and Depression Scale in a large community sample of adolescents in Hong Kong. Quality of Life Research,19(6), 865–873. https://doi.org/10.1007/s11136-010-9645-1.
Boivin, J., Takefman, J., & Braverman, A. (2011). The Fertility Quality of Life (FertiQoL) tool: Development and general psychometric properties. Fertility & Sterility,96(2), 409–415.e403.
Hayes, A. F., & Rockwood, N. J. (2017). Regression-based statistical mediation and moderation analysis in clinical research: Observations, recommendations, and implementation. Behaviour Research and Therapy,98, 39–57. https://doi.org/10.1016/j.brat.2016.11.001.
Hayes, A. F. (2018). Introduction to mediation, moderation, and conditional process analysis second edition: A regression-based approach. New York, NY: Guilford Press.
Hayes, A. F., & Matthes, J. (2009). Computational procedures for probing interactions in OLS and logistic regression: SPSS and SAS implementations. Behavior Research Methods,41(3), 924–936. https://doi.org/10.3758/brm.41.3.924.
Aarts, J. W., van Empel, I. W., Boivin, J., Nelen, W. L., Kremer, J. A., & Verhaak, C. M. (2011). Relationship between quality of life and distress in infertility: A validation study of the Dutch FertiQoL. Human Reproduction,26(5), 1112–1118. https://doi.org/10.1093/humrep/der051.
Hasson, J., Tulandi, T., Shavit, T., Shaulov, T., Seccareccia, E., & Takefman, J. (2017). Quality of life of immigrant and non-immigrant infertile patients in a publicly funded in vitro fertilisation program: A cross-sectional study. BJOG,124(12), 1841–1847. https://doi.org/10.1111/1471-0528.14709.
Goker, A., Yanikkerem, E., Birge, O., & Kuscu, N. K. (2018). Quality of life in Turkish infertile couples and related factors. Human Fertility (Cambridge),21(3), 195–203. https://doi.org/10.1080/14647273.2017.1322223.
ZurloCattaneo DellaVoltaVallone, M. C. M. F. F. (2018). Predictors of quality of life and psychological health in infertile couples: The moderating role of duration of infertility. Quality of Life Research,27(4), 945–954. https://doi.org/10.1007/s11136-017-1781-4.
Chachamovich, J. R., Chachamovich, E., Zachia, S., Knauth, D., & Passos, E. P. (2007). What variables predict generic and health-related quality of life in a sample of Brazilian women experiencing infertility? Human Reproduction,22(7), 1946–1952. https://doi.org/10.1093/humrep/dem080.
Karaca, N., Karabulut, A., Ozkan, S., Aktun, H., Orengul, F., Yilmaz, R., et al. (2016). Effect of IVF failure on quality of life and emotional status in infertile couples. European Journal of Obstetrics, Gynecology, and Reproductive Biology,206, 158–163. https://doi.org/10.1016/j.ejogrb.2016.09.017.
Kim, J. H., & Shin, H. S. (2013). A structural model for quality of life of infertile women. Journal of Korean Academy of Nursing,43(3), 312–320. https://doi.org/10.4040/jkan.2013.43.3.312.
Qu, F., Wu, Y., Zhu, Y. H., Barry, J., Ding, T., Baio, G., et al. (2017). The association between psychological stress and miscarriage: A systematic review and meta-analysis. Scientific Reports,7(1), 1731. https://doi.org/10.1038/s41598-017-01792-3.
Li, W., Newell-Price, J., Jones, G. L., Ledger, W. L., & Li, T. C. (2012). Relationship between psychological stress and recurrent miscarriage. Reproductive Biomedicine Online,25(2), 180–189. https://doi.org/10.1016/j.rbmo.2012.03.012.
Galhardo, A., Cunha, M., & Pinto-Gouveia, J. (2019). A 7-year follow-up study of the Mindfulness-Based Program for Infertility: Are there long-term effects? Clinical Psychology & Psychotherapy. https://doi.org/10.1002/cpp.2362.
Branstrom, R., Duncan, L. G., & Moskowitz, J. T. (2011). The association between dispositional mindfulness, psychological well-being, and perceived health in a Swedish population-based sample. The British Journal of Health Psychology,16(Pt 2), 300–316. https://doi.org/10.1348/135910710x501683.
Schell, L. K., Monsef, I., Wockel, A., & Skoetz, N. (2019). Mindfulness-based stress reduction for women diagnosed with breast cancer. Cochrane Database of Systematic Review. https://doi.org/10.1002/14651858.CD011518.pub2.
Acknowledgements
This work was supported by grants from the Shandong medical and health science and technology development plan (2017WS301). We are thankful for the generous contributions of the research participants and the staffs who assisted with data collection during the study.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. GL and ZJ analyzed and interpreted data and drafted the article; GL contributed to data interpretation and critical review; XH, ZJ and XS were responsible for the collection of data and literature review; WT and XK were in charge for literature review; FM was in charge for study design and essential help.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, G., Jiang, Z., Han, X. et al. A moderated mediation model of perceived stress, negative emotions and mindfulness on fertility quality of life in women with recurrent pregnancy loss. Qual Life Res 29, 1775–1787 (2020). https://doi.org/10.1007/s11136-020-02460-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-020-02460-2