Abstract
Purpose
This study assessed the effectiveness of the Better Life After Cancer: Energy, Strength, and Support (BLESS) program, a 12-week social capital-based exercise adherence program for breast cancer survivors (BCS), regarding cancer-related fatigue (CRF), quality of life (QOL), physical activity, and psychosocial characteristics.
Methods
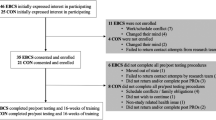
Forty-eight BCS with moderate or high (≥ 4) CRF participated in this randomized control trial (intervention group n = 23, control group n = 25). The intervention group participated in small group sessions to activate social capital while targeting CRF in supervised physical exercises supplemented by home-based physical exercises. The control group was only given written information on exercise. A questionnaire was used to assess CRF, QOL, physical activity, depression, anxiety, sleep quality, and social capital.
Results
The majority of participants had undergone surgery less than 2 years ago. After participating in BLESS, the CRF behavioral/severity domain significantly decreased (t = 2.642, p = 0.011) and physical activity significantly increased (t = − 2.049, p = 0.046) in the intervention group, in comparison with the control group; there were no significant post-intervention differences in the control group. Both groups showed improvements in sleep quality, depression, anxiety, and QOL.
Conclusion
The BLESS program decreased behavioral/severity in the CRF and increased physical activity after 12 weeks among BCS. Future research needs to evaluate whether the promising results on physical activity and behavioral fatigue observed in the short term will persist over time. Also, longer-term effects should be examined.

Similar content being viewed by others
Change history
16 October 2020
Tables��1, 2, and 3 are incorrect.
Abbreviations
- BLESS:
-
Better Life After Cancer: Energy, Strength, and Support
- CRF:
-
cancer-related fatigue
- BCS:
-
breast cancer survivors
- QOL:
-
quality of life
References
Cancer statistics. National Cancer Information Center: Ministry of Health and Welfare; 2019 [Available from: https://www.cancer.go.kr/
Mock V, Abernethy AP, Atkinson A, Barsevick AM, Berger AM, Cella D et al (2007) Cancer-related fatigue clinical practice guidelines in oncology. J Natl Compr Cancer Netw 5(10):1054–1078
Mallinson T, Cella D, Cashy J, Holzner B (2006) Giving meaning to measure: linking self-reported fatigue and function to performance of everyday activities. J Pain Symptom Manag 31(3):229–241
Bower JE (2014) Cancer-related fatigue—mechanisms, risk factors, and treatments. Nat Rev Clin Oncol 11(10):597–609
Oh CH, Park H, Lee JS, Choi JY (2016) A test for psychobiologic entropy model on cancer related fatigue among patients with solid tumors. Korean J Adult Nurs 28(1):1–12
Jaremka LM, Andridge RR, Fagundes CP, Alfano CM, Povoski SP, Lipari AM, Agnese DM, Arnold MW, Farrar WB, Yee LD, Carson WE 3rd, Bekaii-Saab T, Martin EW Jr, Schmidt CR, Kiecolt-Glaser JK (2014) Pain, depression, and fatigue: loneliness as a longitudinal risk factor. Health Psychol 33(9):948–957
Neil SE, Klika RJ, Garland SJ, McKenzie DC, Campbell KL (2013) Cardiorespiratory and neuromuscular deconditioning in fatigued and non-fatigued breast cancer survivors. Support Care Cancer 21(3):873–881
Windsor P, Potter J, McAdam K, McCowan C (2009) Evaluation of a fatigue initiative: information on exercise for patients receiving cancer treatment. Clin Oncol 21(6):473–482
Kim T-S, Park I-S (2018) The roles of exercise in cancer prevention and improvement of health for cancer survivors. J Korea Entertain Ind Assoc 12(1):165–173
Allgayer H, Owen RW, Nair J, Allgayer H, Owen RW, Nair J et al (2008) Short-term moderate exercise programs reduce oxidative DNA damage as determined by high-performance liquid chromatography-electrospray ionization-mass spectrometry in patients with colorectal carcinoma following primary treatment. Scand J Gastroenterol 43(8):971–978
Fong DY, Ho JW, Hui BP, Lee AM, Macfarlane DJ, Leung SS et al (2012) Physical activity for cancer survivors: meta-analysis of randomised controlled trials. Bmj. 344:e70
Hutnick NA, Williams NI, Kraemer WJ, Orsega-Smith E, Dixon RH, Bleznak AD, Mastro AM (2005) Exercise and lymphocyte activation following chemotherapy for breast cancer. Med Sci Sports Exerc 37(11):1827–1835
Kroenke CH, Chen WY, Rosner B, Holmes MD (2005) Weight, weight gain, and survival after breast cancer diagnosis. J Clin Oncol 23(7):1370–1378
Kim I (2014) Literature review of exercise therapy effects in patients with breast cancer. J Korean Soc Integr Med 2(2):49–58
Chae Y-R, Choe M-A (2001) Effects of exercise on cardiopulmonary functions and shoulder joint functioning in breast cancer patients undergoing radiation therapy after breast surgery. J Korean Acad Nurs 31(3):454–466
Burnham TR, Wilcox A (2002) Effects of exercise on physiological and psychological variables in cancer survivors. Med Sci Sports Exerc 34(12):1863–1867
Eom AY, Lee E (2004) Shoulder range of motion in postmastectomy patients. Asian Oncol Nurs 4(1):62–70
Young B (2003) Typology of social capital through the empirical analysis on cyber communities. Korean J Sociol 37(5):161–186
Putnam R. The prosperous community: social capital and public life. The american prospect. 1993;13(Spring), Vol. 4. Available online: http://www.prospect.org/print/vol/13 (accessed 7 April 2003)
Jang Y-M (2011) A study on the effects to the change of social capital from participation in elderly employment programs. Korean J Soc Welf 63(2):261–289
Lee S, Lee S (2018) A study on the relationship between lifelong education and social capital formation. J Lifelong Learn Soc 14(1):71–100
Yoon S-J 2013 A network approach to the effects of social capital: bonding vs. bridging The e-Business Studies 14(1):203–24
Putnam RD 2000 Bowling alone: America’s declining social capital. Culture and politics: Springer. p. 223–34
Leonard M (2004) Bonding and bridging social capital: reflections from Belfast. Sociology. 38(5):927–944
Michael YL, Berkman LF, Colditz GA, Holmes MD, Kawachi I (2002) Social networks and health-related quality of life in breast cancer survivors: a prospective study. J Psychosom Res 52(5):285–293
Bender JL, Jimenez-Marroquin MC, Ferris LE, Katz J, Jadad AR (2013) Online communities for breast cancer survivors: a review and analysis of their characteristics and levels of use. Support Care Cancer 21(5):1253–1263
Giese-Davis J, Bliss-Isberg C, Carson K, Star P, Donaghy J, Cordova MJ et al (2006) The effect of peer counseling on quality of life following diagnosis of breast cancer: an observational study. Psychooncology 15(11):1014–1022
Schover LR, Jenkins R, Sui D, Adams JH, Marion MS, Jackson KE (2006) Randomized trial of peer counseling on reproductive health in African American breast cancer survivors. J Clin Oncol 24(10):1620–1626
Wen M, Browning CR, Cagney KA (2007) Neighbourhood deprivation, social capital and regular exercise during adulthood: a multilevel study in Chicago. Urban Stud 44(13):2651–2671
Stang I, Mittelmark MB (2010) Intervention to enhance empowerment in breast cancer self-help groups. Nurs Inq 17(1):47–57
Kim GY, Kim EM, Bae SS (2009) Social capital and stage of change for physical activity in a community sample of adults. J Korean Soc Health Educ Promot 26(1):63–80
Kim S, Ko YH, Song Y, Kang MJ, Lee H, Kim SH et al (2019) Development of an exercise adherence program for breast cancer survivors with cancer-related fatigue—an intervention mapping approach. Support Care Cancer:1–8
Sandel SL, Judge JO, Landry N, Faria L, Ouellette R, Majczak M (2005) Dance and movement program improves quality-of-life measures in breast cancer survivors. Cancer Nurs 28(4):301–309
Villalonga-Olives E, Kawachi I (2015) The measurement of social capital. Gac Sanit 29:62–64
Armstrong T, Bull F (2006) Development of the world health organization global physical activity questionnaire (GPAQ). J Public Health 14(2):66–70
Jeon Y 2013 Development of the Korean version of global physical activity questionnaire and assessment of reliability and validity. Academic research on task, Final Report, Korea Center for Disease Control and Prevention
Lee EH (1999) Construct validity of the revised Piper Fatigue Scale in Korean women with breast cancer. J Korean Acad Nurs 29(2):485–493
Brady MJ, Cella DF, Mo F, Bonomi AE, Tulsky DS, Lloyd SR, Deasy S, Cobleigh M, Shiomoto G (1997) Reliability and validity of the functional assessment of cancer therapy-breast quality-of-life instrument. J Clin Oncol 15(3):974–986
Oh SM, Min KJ, Park DB (1999) A study on the standardization of the hospital anxiety and depression scale for Koreans: a comparison of normal, depressed and anxious groups. J Korean Neurol Assoc 38(2):289–296
Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67(6):361–370
Buysse DJ, Reynolds Iii CF, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28(2):193–213
Sohn SI, Kim DH, Lee MY, Cho YW (2012) The reliability and validity of the Korean version of the Pittsburgh Sleep Quality Index. Sleep Breath 16(3):803–812
Carpenter JS, Andrykowski MA (1998) Psychometric evaluation of the Pittsburgh Sleep Quality Index. J Psychosom Res 45(1):5–13
Wang P, Chen X, Gong J, Jacques-Tiura AJ (2014) Reliability and validity of the personal social capital scale 16 and personal social capital scale 8: two short instruments for survey studies. Soc Indic Res 119(2):1133–1148
Chen X, Stanton B, Gong J, Fang X, Li X (2008) Personal Social Capital Scale: an instrument for health and behavioral research. Health Educ Res 24(2):306–317
Gerritsen JK, Vincent AJ (2016) Exercise improves quality of life in patients with cancer: a systematic review and meta-analysis of randomised controlled trials. Br J Sports Med 50(13):796–803
Lipsett A, Barrett S, Haruna F, Mustian K, O’Donovan A (2017) The impact of exercise during adjuvant radiotherapy for breast cancer on fatigue and quality of life: a systematic review and meta-analysis. Breast 32:144–155
American College of Sports Medicine. ACSM’s guidelines for exercise testing and prescription. 6th ed. Lippincott Williams & Wilkins; Philadelphia, PA: 2009
Acknowledgments
We wish to acknowledge the breast cancer survivors who participated in our study.
Funding
This research was supported by the Basic Science Research Program through the National Research Foundation for Korea (NRF) funded by the Ministry of Education (grant number: 2015R1D1A1A01059846).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
An institutional review board exemption was obtained from Severance Hospital, Korea (IRB 4–2017–0164).
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kim, S., Ko, Y.H., Song, Y. et al. Pre-post analysis of a social capital-based exercise adherence intervention for breast cancer survivors with moderate fatigue: a randomized controlled trial. Support Care Cancer 28, 5281–5289 (2020). https://doi.org/10.1007/s00520-020-05363-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05363-7