Abstract
Objective
The progression of white matter hyperintensities (WMH) varies considerably in adults. In this study, we aimed to predict the progression and related risk factors of WMH based on the radiomics of whole-brain white matter (WBWM).
Methods
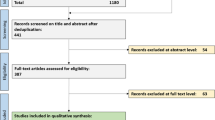
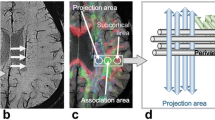
A retrospective analysis was conducted on 141 patients with WMH who underwent two consecutive brain magnetic resonance (MR) imaging sessions from March 2014 to May 2018. The WBWM was segmented to extract and score the radiomics features at baseline. Follow-up images were evaluated using the modified Fazekas scale, with progression indicated by scores ≥ 1. Patients were divided into progressive (n = 65) and non-progressive (n = 76) groups. The progressive group was subdivided into any WMH (AWMH), periventricular WMH (PWMH), and deep WMH (DWMH). Independent risk factors were identified using logistic regression.
Results
The area under the curve (AUC) values for the radiomics signatures of the training sets were 0.758, 0.749, and 0.775 for AWMH, PWMH, and DWMH, respectively. The AUC values of the validation set were 0.714, 0.697, and 0.717, respectively. Age and hyperlipidemia were independent predictors of progression for AWMH. Age and body mass index (BMI) were independent predictors of progression for DWMH, while hyperlipidemia was an independent predictor of progression for PWMH. After combining clinical factors and radiomics signatures, the AUC values were 0.848, 0.863, and 0.861, respectively, for the training set, and 0.824, 0.818, and 0.833, respectively, for the validation set.
Conclusions
MRI-based radiomics of WBWM, along with specific risk factors, may allow physicians to predict the progression of WMH.
Key Points
• Radiomics features detected by magnetic resonance imaging may be used to predict the progression of white matter hyperintensities.
• Radiomics may be used to identify risk factors associated with the progression of white matter hyperintensities.
• Radiomics may serve as non-invasive biomarkers to monitor white matter status.






Similar content being viewed by others
Abbreviations
- AUC:
-
Area under the curve
- AWMH:
-
Progression of WMH in any (periventricular and/or deep) region
- BMI:
-
Body mass index
- DTI:
-
Diffusion tensor imaging
- DWMH:
-
Deep white matter hyperintensities
- FLAIR:
-
Fluid attenuated inversion recovery
- GLCM:
-
Gray-level co-occurrence matrix
- ICC:
-
Intraclass correlation coefficient
- LASSO:
-
The least absolute shrinkage and selection operator
- LDL:
-
Low-density lipoprotein
- MRI:
-
Magnetic resonance imaging
- NAWM:
-
Normal-appearing white matter
- PWMH:
-
Periventricular white matter hyperintensities
- RLM:
-
Run-length matrix
- ROC:
-
Receiver operating characteristic
- ROI:
-
Region of interest
- WBWM:
-
Whole-brain white matter
- WMH:
-
White matter hyperintensities
References
Wardlaw JM, Smith C, Dichgans M (2013) Mechanisms of sporadic cerebral small vessel disease: insights from neuroimaging. Lancet Neurol 12:483–497
Maillard P, Fletcher E, Harvey D et al (2011) White matter hyperintensity penumbra. Stroke 42:1917–1922
Valdes Hernandez Mdel C, Armitage PA, Thrippleton MJ et al (2015) Rationale, design and methodology of the image analysis protocol for studies of patients with cerebral small vessel disease and mild stroke. Brain Behav 5:e00415
Taylor ANW, Kambeitz-Ilankovic L, Gesierich B et al (2017) Tract-specific white matter hyperintensities disrupt neural network function in Alzheimer’s disease. Alzheimers Dement 13:225–235
Valdes Hernandez MDC, Gonzalez-Castro V, Chappell FM et al (2017) Application of texture analysis to study small vessel disease and blood-brain barrier integrity. Front Neurol 8:327
Lee WJ, Jung KH, Ryu YJ et al (2017) Progression of cerebral white matter hyperintensities and the associated sonographic index. Radiology 284:824–833
Holmegaard L, Jensen C, Redfors P, Blomstrand C, Jern C, Jood K (2018) Long-term progression of white matter hyperintensities in ischemic stroke. Acta Neurol Scand 138:548–556
Yip SS, Aerts HJ (2016) Applications and limitations of radiomics. Phys Med Biol 61:R150–R166
Liang C, Huang Y, He L et al (2016) The development and validation of a CT-based radiomics signature for the preoperative discrimination of stage I-II and stage III-IV colorectal cancer. Oncotarget 7:31401–31412
Huang YQ, Liang CH, He L et al (2016) Development and validation of a radiomics nomogram for preoperative prediction of lymph node metastasis in colorectal cancer. J Clin Oncol 34:2157–2164
Abbasian Ardakani A, Gharbali A, Saniei Y, Mosarrezaii A, Nazarbaghi S (2015) Application of texture analysis in diagnosis of multiple sclerosis by magnetic resonance imaging. Glob J Health Sci 7:68–78
Holli KK, Harrison L, Dastidar P et al (2010) Texture analysis of MR images of patients with mild traumatic brain injury. BMC Med Imaging 10:8
Wardlaw JM, Valdes Hernandez MC, Munoz-Maniega S (2015) What are white matter hyperintensities made of? Relevance to vascular cognitive impairment. J Am Heart Assoc 4:001140
Promjunyakul N, Lahna D, Kaye JA et al (2015) Characterizing the white matter hyperintensity penumbra with cerebral blood flow measures. Neuroimage Clin 8:224–229
Shao Y, Chen Z, Ming S et al (2018) Predicting the development of normal-appearing white matter with radiomics in the aging brain: a longitudinal clinical study. Front Aging Neurosci 10:393
Prins ND, van Straaten EC, van Dijk EJ et al (2004) Measuring progression of cerebral white matter lesions on MRI: visual rating and volumetrics. Neurology 62:1533–1539
Kim KW, MacFall JR, Payne ME (2008) Classification of white matter lesions on magnetic resonance imaging in elderly persons. Biol Psychiatry 64:273–280
ten Dam VH, van den Heuvel DM, de Craen AJ et al (2007) Decline in total cerebral blood flow is linked with increase in periventricular but not deep white matter hyperintensities. Radiology 243:198–203
van den Heuvel DM, ten Dam VH, de Craen AJ et al (2006) Increase in periventricular white matter hyperintensities parallels decline in mental processing speed in a non-demented elderly population. J Neurol Neurosurg Psychiatry 77:149–153
Maillard P, Carmichael O, Fletcher E, Reed B, Mungas D, DeCarli C (2012) Coevolution of white matter hyperintensities and cognition in the elderly. Neurology 79:442–448
Park BY, Lee MJ, Lee SH et al (2018) DEWS (DEep White matter hyperintensity Segmentation framework): a fully automated pipeline for detecting small deep white matter hyperintensities in migraineurs. Neuroimage Clin 18:638–647
Fazekas F, Kleinert R, Offenbacher H et al (1993) Pathologic correlates of incidental MRI white matter signal hyperintensities. Neurology 43:1683–1689
Schmidt R, Schmidt H, Haybaeck J et al (2011) Heterogeneity in age-related white matter changes. Acta Neuropathol 122:171–185
Bernbaum M, Menon BK, Fick G et al (2015) Reduced blood flow in normal white matter predicts development of leukoaraiosis. J Cereb Blood Flow Metab 35:1610–1615
Nasel C, Boubela R, Kalcher K, Moser E (2017) Normalised time-to-peak-distribution curves correlate with cerebral white matter hyperintensities - could this improve early diagnosis? J Cereb Blood Flow Metab 37:444–455
Madden DJ, Spaniol J, Whiting WL et al (2007) Adult age differences in the functional neuroanatomy of visual attention: a combined fMRI and DTI study. Neurobiol Aging 28:459–476
Maillard P, Fletcher E, Lockhart SN et al (2014) White matter hyperintensities and their penumbra lie along a continuum of injury in the aging brain. Stroke 45:1721–1726
Yoon CW, Choi Y, Jeon S et al (2017) Is antiplatelet treatment effective at attenuating the progression of white matter hyperintensities? PLoS One 12:e0176300
Munoz Maniega S, Chappell FM, Valdes Hernandez MC et al (2017) Integrity of normal-appearing white matter: influence of age, visible lesion burden and hypertension in patients with small-vessel disease. J Cereb Blood Flow Metab 37:644–656
Grueter BE, Schulz UG (2012) Age-related cerebral white matter disease (leukoaraiosis): a review. Postgrad Med J 88:79–87
Moody DM, Thore CR, Anstrom JA, Challa VR, Langefeld CD, Brown WR (2004) Quantification of afferent vessels shows reduced brain vascular density in subjects with leukoaraiosis. Radiology 233:883–890
Stokes KY, Cooper D, Tailor A, Granger DN (2002) Hypercholesterolemia promotes inflammation and microvascular dysfunction: role of nitric oxide and superoxide. Free Radic Biol Med 33:1026–1036
VanTeeffelen JW, Constantinescu AA, Vink H, Spaan JA (2005) Hypercholesterolemia impairs reactive hyperemic vasodilation of 2A but not 3A arterioles in mouse cremaster muscle. Am J Physiol Heart Circ Physiol 289:H447–H454
Cho YI, Cho DJ, Rosenson RS (2014) Endothelial shear stress and blood viscosity in peripheral arterial disease. Curr Atheroscler Rep 16:404
Ryu WS, Woo SH, Schellingerhout D et al (2014) Grading and interpretation of white matter hyperintensities using statistical maps. Stroke 45:3567–3575
Griffanti L, Jenkinson M, Suri S et al (2018) Classification and characterization of periventricular and deep white matter hyperintensities on MRI: a study in older adults. Neuroimage 170:174–181
van Overbeek EC, Staals J, Knottnerus IL, ten Cate H, van Oostenbrugge RJ et al (2016) Plasma tPA-activity and progression of cerebral white matter hyperintensities in lacunar stroke patients. PLoS One 11:e0150740
Lee WJ, Jung KH, Ryu YJ et al (2017) Cystatin C, a potential marker for cerebral microvascular compliance, is associated with white-matter hyperintensities progression. PLoS One 12:e0184999
Harrison LC, Raunio M, Holli KK et al (2010) MRI texture analysis in multiple sclerosis: toward a clinical analysis protocol. Acad Radiol 17:696–707
Tozer DJ, Zeestraten E, Lawrence AJ, Barrick TR, Markus HS (2018) Texture analysis of T1-weighted and fluid-attenuated inversion recovery images detects abnormalities that correlate with cognitive decline in small vessel disease. Stroke 49:1656–1661
Loizou CP, Pattichis CS, Seimenis I et al (2009) Quantitative analysis of brain white matter lesions in multiple sclerosis subjects. International Conference on Information Technology & Applications in Biomedicine; 1–4
Li Z, Mao Y, Huang W et al (2017) Texture-based classification of different single liver lesion based on SPAIR T2W MRI images. BMC Med Imaging 17:42
Yu O, Steibel J, Mauss Y et al (2004) Remyelination assessment by MRI texture analysis in a cuprizone mouse model. Magn Reson Imaging 22:1139–1144
Gouw AA, van der Flier WM, van Straaten EC et al (2008) Reliability and sensitivity of visual scales versus volumetry for evaluating white matter hyperintensity progression. Cerebrovasc Dis 25:247–253
Acknowledgments
We are grateful to Ms. Peipei Pang (GE Healthcare, Shanghai, China) for her technical support.
Funding
Fund of Zhejiang Traditional Chinese Medicine Science Research Projection in China (2019ZA004) and Fund of Health Commission of Zhejiang Province in China (2019KY302).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Zhenyu Shu.
Conflict of interest
One of the authors of this manuscript (Peipei Pang) is an employee of GE Healthcare China. The remaining authors declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
Some study subjects or cohorts have been previously reported in Shao Y, Chen Z, Ming S, et al Predicting the Development of Normal-Appearing White Matter With Radiomics in the Aging Brain: A Longitudinal Clinical Study. Front Aging Neurosci 2018;10:393.
Methodology
• Retrospective
• Diagnostic or prognostic study
• Performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOC 1621 kb)
Rights and permissions
About this article
Cite this article
Shu, Z., Xu, Y., Shao, Y. et al. Radiomics from magnetic resonance imaging may be used to predict the progression of white matter hyperintensities and identify associated risk factors. Eur Radiol 30, 3046–3058 (2020). https://doi.org/10.1007/s00330-020-06676-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-06676-1