Abstract
Background
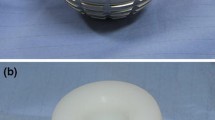
Patients undergoing primary total hip arthroplasty (THA) with prior lumbar spine fusion (LSF) are a high-risk group for instability with reported incidence of dislocation as high as 8.3% using fixed bearing femoral heads. Purpose of this study was to determine risk of post-operative instability in patients undergoing primary THA with a history of prior LSF using dual mobility acetabular cups.
Methods
This was a multicenter retrospective study with 93 patients undergoing primary THA using a dual mobility cup with a prior history of instrumented LSF. There were 56 females and 47 males with an average age of 66 years (46–87) and average BMI of 30 with mean follow-up of 2.7 years (range 12–124 months). Surgical approach included posterior (63), direct lateral (15), anterior (11), and direct superior (4). Forty-four percent had one level lumbar fusion, 29% with two levels, and 15% with three or more levels fused. The primary outcome investigated was instability.
Results
There were no cases of instability or prosthetic joint infection in this group of patients with prior lumbar spine fusion undergoing primary THA using a dual mobility cup. There was one intra-operative periprosthetic femur fracture and one case of aseptic acetabular cup loosening.
Conclusion
Patients undergoing THA with prior LSF are at increased risk for instability due to loss of normal spinopelvic relationship. The use of dual mobility cups in patients with prior LSF undergoing primary THA appears promising with no cases of instability in this high-risk group of patients.


Similar content being viewed by others
References
Bozic KJ, Kurtz SM, Lau E, Ong K, Vail TP, Berry DJ (2009) The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am 91(1):128–133
Gwam CU, Mistry JB, Mohamed NS, Thomas M, Bigart KC, Mont MA, Delanois RE (2017) Current Epidemiology of Revision Total Hip Arthroplasty in the United States: National Inpatient Sample 2009 to 2013. J Arthroplasty 32(7):2088–2092
Goel A, Lau EC, Ong KL, Berry DJ, Malkani AL (2015) Dislocation rates following primary total hip arthroplasty have plateaued in the Medicare population. J Arthroplasty 30(5):7436
Buckland AJ, Puvanesarajah V, Vigdorchik J, Schwarzkopf R, Jain A, Klineberg EO, Hart RA, Callaghan JJ, Hassanzadeh H (2017) Dislocation of a primary total hip arthroplasty is more common in patients with a lumbar spinal fusion. Bone Joint J 99-B(5):585–591
Perfetti DC, Schwarzkopf R, Buckland AJ, Paulino CB, Vigdorchik JM (2017) Prosthetic dislocation and revision after primary Total hip Arthroplasty in lumbar fusion patients: a propensity score matched-pair analysis. J Arthroplasty 32(5):1635–1640
An VVG, Phan K, Sivakumar BS, Mobbs RJ, Bruce WJ (2018) Prior lumbar spinal fusion is associated with an increased risk of dislocation and revision in Total hip Arthroplasty: a meta-analysis. J Arthroplasty 33(1):297–300
Salib CG, Reina N, Perry KI, Taunton MJ, Berry DJ, Abdel MP (2019) Lumbar fusion involving the sacrum increases dislocation risk in primary total hip arthroplasty. Bone Joint J 101-B(2):198–206
Malkani AL, Garber AT, Ong KL, Dimar JR, Baykal D, Glassman SD, Cochran AR, Berry DJ (2018) Total hip Arthroplasty in patients with previous lumbar fusion surgery: are there more dislocations and revisions? J Arthroplasty 33(4):1189–1193
Heckmann N, McKnight B, Stefl M, Trasolini NA, Ike H, Dorr LD (2018) Late dislocation following Total hip Arthroplasty: Spinopelvic imbalance as a causative factor. J Bone Joint Surg Am 100(21):1845–1853
Bedard NA, Martin CT, Slaven SE, Pugely AJ, Mendoza-Lattes SA, Callaghan JJ (2016) Abnormally high dislocation rates of Total hip Arthroplasty after spinal deformity surgery. J Arthroplasty 31(12):2884–2885
Esposito CI, Carroll KM, Sculco PK, Padgett DE, Jerabek SA, Mayman DJ (2018) Total hip Arthroplasty patients with fixed Spinopelvic alignment are at higher risk of hip dislocation. J Arthroplasty 33(5):1449–1454
Lazennec JY, Boyer P, Gorin M, Catonné Y, Rousseau MA (2011) Acetabular anteversion with CT in supine, simulated standing, and sitting positions in a THA patient population. Clin Orthop Relat Res 469(4):1103–1109
Kanawade V, Dorr LD, Wan Z (2014) Predictability of Acetabular component angular change with postural shift from standing to sitting position. J Bone Joint Surg Am 96(12):978–986
McArthur BA, Nam D, Cross MB, Westrich GH, Sculco TP (2013) Dual-mobility acetabular components in total hip arthroplasty. Am J Orthop (Belle Mead NJ) 42(10):473–478
Huang RC, Malkani AL, Harwin SF, Hozack WJ, Mont MA, Higuera-Rueda CA, Westrich GH (2019) Multicenter evaluation of a modular dual mobility construct for revision Total hip Arthroplasty. J Arthroplasty 34(7S):S287–S291
Hartzler MA, Abdel MP, Sculco PK, Taunton MJ, Pagnano MW, Hanssen AD (2018) Otto Aufranc award: dual-mobility constructs in revision THA reduced dislocation, Rerevision, and reoperation compared with large femoral heads. Clin Orthop Relat Res 476(2):293–301
Gausden EB, Parhar HS, Popper JE, Sculco PK, Rush BNM (2018) Risk factors for early dislocation following primary elective Total hip Arthroplasty. J Arthroplasty 33(5):1567–1571
Eftekhary N, Shimmin A, Lazennec JY, Buckland A, Schwarzkopf R, Dorr LD, Mayman D, Padgett D, Vigdorchik J (2019) A systematic approach to the hip-spine relationship and its applications to total hip arthroplasty. Bone Joint J 101-B(7):808–816
Lazennec JY, Brusson A, Rousseau MA (2011) Hip-spine relations and sagittal balance clinical consequences. Eur Spine J 20(Suppl 5):686–698
Lazennec JY, Clark IC, Folinais D, Tahar IN, Pour AE (2017) What is the impact of a spinal fusion on Acetabular implant orientation in functional standing and sitting positions? J Arthroplasty 32(10):3184–3190
Barry JJ, Sing DC, Vail TP, Hansen EN (2017) Early outcomes of primary Total hip Arthroplasty after prior lumbar spinal fusion. J Arthroplasty 32(2):470–474
Phan D, Bederman SS, Schwarzkopf R (2015) The influence of sagittal spinal deformity on anteversion of the acetabular component in total hip arthroplasty. Bone Joint J 97-B(8):1017–1023
Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR (1978) Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am 60(2):217–220
DelSole EM, Vigdorchik JM, Schwarzkopf R, Errico TJ, Buckland AJ (2017) Total hip Arthroplasty in the spinal deformity population: does degree of sagittal deformity affect rates of safe zone placement, instability, or revision? J Arthroplasty 32(6):1910–1917
Tezuka T, Heckmann ND, Bodner RJ, Dorr LD (2019) Functional safe zone is superior to the Lewinnek safe zone for Total hip Arthroplasty: why the Lewinnek safe zone is not always predictive of stability. J Arthroplasty 34(1):3–8
Buckland AJ, Vigdorchik J, Schwab FJ, Errico TJ, Lafage R, Ames C, Bess S, Smith J, Mundis GM, Lafage V (2015) Acetabular Anteversion changes due to spinal deformity correction: bridging the gap between hip and spine surgeons. J Bone Joint Surg Am 97(23):1913–1920
Reina N, Pareek A, Krych AJ, Pagnano MW, Berry DJ, Abdel MP (2019) Dual-mobility constructs in primary and revision Total hip Arthroplasty: a systematic review of comparative studies. J Arthroplasty 34(3):594–603
Romagnoli M, Grassi A, Costa GG, Lazaro LE, Lo Presti M, Zaffagnini S (2019) The efficacy of dual-mobility cup in preventing dislocation after total hip arthroplasty: a systematic review and meta-analysis of comparative studies. Int Orthop 43(5):1071–1082
Fabry C, Langlois J, Hamadouche M, Bader R (2016) Intra-prosthetic dislocation of dual-mobility cups after total hip arthroplasty: potential causes from a clinical and biomechanical perspective. Int Orthop 40(5):901–906
Hamadouche M, Arnould H, Bouxin B (2012) Is a cementless dual mobility socket in primary THA a reasonable option? Clin Orthop Relat Res 470(11):3048–3053
Combes A, Migaud H, Girard J, Duhamel A, Fessy MH (2013) Low rate of dislocation of dual-mobility cups in primary total hip arthroplasty. Clin Orthop Relat Res 471(12):3891–3900. https://doi.org/10.1007/s11999-013-2929-3
Kreipke R, Rogmark C, Pedersen AB, Kärrholm J, Hallan G, Havelin LI, Mäkelä K, Overgaard S (2019) Dual mobility cups: effect on risk of revision of primary Total hip Arthroplasty due to osteoarthritis: a matched population-based study using the Nordic Arthroplasty register association database. J Bone Joint Surg Am 101(2):169–176
Reina N, Delaunay C, Chiron P, Ramdane N, Hamadouche M, Société française de chirurgie orthopédique et traumatologique (2013) Infection as a cause of primary total hip arthroplasty revision and its predictive factors. Orthop Traumatol Surg Res 99(5):555–561
Elson L, Dounchis J, Illgen R, Marchand RC, Padgett DE, Bragdon CR, Malchau H (2015) Precision of acetabular cup placement in robotic integrated total hip arthroplasty. Hip Int 25(6):531–536
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Arthur L. Malkani, MD, Joseph P. Nessler, MD, Geoff Westrich, MD, Steven F. Harwin, MD, and Seth Jerabek, MD report a conflict of interest with Stryker. David Mayman, MD reports a conflict of interest with Smith and Nephew. Shikha Sachdeva, MD, has no conflict of interest to declare.
Human and animal rights and informed consent
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nessler, J.M., Malkani, A.L., Sachdeva, S. et al. Use of dual mobility cups in patients undergoing primary total hip arthroplasty with prior lumbar spine fusion. International Orthopaedics (SICOT) 44, 857–862 (2020). https://doi.org/10.1007/s00264-020-04507-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-020-04507-y