Abstract
Introduction
The incidence of AML is increasing, in part due to an aging population. Since 2017, eight novel agents have been introduced, 6 of which are oral: midostaurin, enasidenib, ivosidenib, gilteritinib, glasdegib, and venetoclax. With an increase in oral medications (OMs), patients face associated side effects that accompany OMs, which often decreases adherence. We aimed to identify and summarize adherence to OMs in this population.
Methods
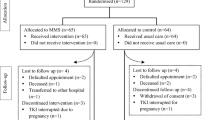
Our mixed method design used focus groups (FG) and patient surveys. After IRB approval, 11 patients and 4 caregivers participated in 4 FGs. Themes from the FGs were used to develop a 37-item OMs adherence needs assessment. Participants were recruited and consented at three cancer centers to complete surveys (online, at the clinic, hospital, or from home).
Results
A total of 100 patients completed OMs survey. The number of pills to be taken was the most frequent and troublesome challenge. The most frequently reported interventions that would improve patient adherence were smaller pills, easier packaging, and scheduling assistance. Nearly 33% of patients indicated they skip OMs dose altogether when they forget to take it. Younger patients (< 65 years) were more accepting of taking oral compared with intravenous medications (p = .03).
Conclusion
This study represents the first assessment of OMs adherence in adults with AML. Findings provide the basis for further exploration of interventions to enhance and increase adherence to OMs regimens.




Similar content being viewed by others
References
American Cancer Society (2019) Key statistics for acute myeloid leukemia (AML). https://www.cancer.org/cancer/acute-myeloid-leukemia/about/key-statistics.html. Accessed 5 Sept 2019
Siegel RL, Miller KD, Jemal A (2019) Cancer statistics, 2019. CA Cancer J Clin 69(1):7–34. https://doi.org/10.3322/caac.21551
National Comprehensive Cancer Network (NCCN) (2018) NCCN clinical practice guidelines in oncology: acute myeloid leukemia. http://oncolife.com.ua/doc/nccn/Acute_Myeloid_Leukemia.pdf
Leak Bryant A, Lee Walton A, Shaw-Kokot J, Mayer DK, Reeve BB (2015) Patient-reported symptoms and quality of life in adults with acute leukemia: a systematic review. Oncol Nurs Forum 42(2):e91–e101. https://doi.org/10.1188/15.onf.e91-e101
Leak Bryant A, Coffman EM, Phillips B, Gray TF, Knafl GJ, Klepin HD, Wood WA, Muss H, Reeve BB (2018) Symptoms, mobility and function, and quality of life in adults with acute leukemia during initial hospitalization. Oncol Nurs Forum 45(5):653–664. https://doi.org/10.1188/18.onf.653-664
Albrecht TA (2014) Physiologic and psychological symptoms experienced by adults with acute leukemia: an integrative literature review. Oncol Nurs Forum 41(3):286–295. https://doi.org/10.1188/14.onf.286-2957
Mukherjee S, Sekeres M (2019) Novel therapies in acute myeloid leukemia. Semin Oncol Nurs 35(6):150955. https://doi.org/10.1016/j.soncn.2019.150955
Greer JA, Amoyal N, Nisotel L, Fishbein JN, MacDonald J, Stagl J, Lennes I, Temel JS, Safren SA, Pirl WF (2016) A systematic review of adherence to oral antineoplastic therapies. Oncologist 21(3):354–376. https://doi.org/10.1634/theoncologist.2015-0405
Noens L, van Lierde MA, De Bock R, Verhoef G, Zachee P, Berneman Z, Martiat P, Mineur P, Van Eygen K, MacDonald K, De Geest S, Albrecht T, Abraham I (2009) Prevalence, determinants, and outcomes of nonadherence to imatinib therapy in patients with chronic myeloid leukemia: the ADAGIO study. Blood 113(22):5401–5411. https://doi.org/10.1182/blood-2008-12-196543
Mislang AR, Wildes TM, Kanesvaran R, Baldini C, Holmes HM, Nightingale G, Coolbrandt A, Biganzoli L (2017) Adherence to oral cancer therapy in older adults: the International Society of Geriatric Oncology (SIOG) taskforce recommendations. Cancer Treat Rev 57:58–66. https://doi.org/10.1016/j.ctrv.2017.05.002
Bryant AL, Chan Y, Richardson J, Foster M, Owenby S, Wujcik D (in press) Understanding barriers to oral therapy adherence in adults with acute myeloid leukemia. Journal of the Advanced Practitioner in Oncology.
IBM (Released 2019). SPSS Statistics for Windows, Version 26.0, NY: IBM Corp
De Geest S, Zullig LL, Dunbar-Jacob J, Helmy R, Hughes DA, Wilson IB, Vrijens B (2018) ESPACOMP Medication adherence reporting guideline (EMERGE). Ann Intern Med 169(1):30–35. https://doi.org/10.7326/m18-0543
Costa AL, Abreu C, Pacheco TR, Macedo D, Sousa AR, Pulido C, Quintela A, Costa L (2015) Prevention of nausea and vomiting in patients undergoing oral anticancer therapies for solid tumors. Biomed Res Int 2015:309601. https://doi.org/10.1155/2015/309601
Wu YP, Linder LA, Kanokvimankul P, Fowler B, Parsons BG, Macpherson CF, Johnson RH (2018) Use of a smartphone application for prompting oral medication adherence among adolescents and young adults with cancer. Oncol Nurs Forum 45(1):69–76. https://doi.org/10.1188/18.onf.69-76
Malawi Cancer Consortium (2019). http://malawicancerconsortium.web.unc.edu/. Accessed 5 Sept 2019
Dayer L, Heldenbrand S, Anderson P, Gubbins PO, Martin BC (2013) Smartphone medication adherence apps: potential benefits to patients and providers. J Am Pharm Assoc 53(2):172–181. https://doi.org/10.1331/JAPhA.2013.12202
Acknowledgments
This work was supported by Astellas, Inc. We also thank UNC Connected Health for Applications and Interventions (CHAI) core for their efforts in facilitating the interviews and analysis. We thank the patients, caregivers, and nursing staff from all sites for their support of this study.
Funding
This work was supported in part by the University of North Carolina at Chapel Hill’s Connected Health Applications & Interventions Core (CHAI Core) through a grant from NIH (DK056350) to the University of North Carolina Nutrition Obesity Research Center AND/OR from NCI (P30-CA16086) to the Lineberger Comprehensive Cancer Center.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Ashley Leak Bryant, Thomas LeBlanc, Tara Albrecht, Ya-Ning Chan, Jaime Richardson, Matthew Foster, Melissa Dang, William Dudley Susie Owenby, and Debbie Wujcik. The first draft of the manuscript was written by Dr. Ashley Leak Bryant and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
The study was reviewed and approved by the University of North Carolina at Chapel Hill Institutional Review Board (IRB). Informed consent was obtained by all participants prior to joining the groups.
Conflict of interest
Dr. Bryant has received grants from Carevive during the conduct of the study and honorarium outside the submitted work. Dr. Leblanc has received personal fees from AbbVie, personal fees from Agios, grants and personal fees from AstraZeneca, personal fees from Amgen, personal fees from CareVive, personal fees and other from Celgene, personal fees from Daiichi-Sankyo, personal fees from FlatIron, personal fees from Helsinn, personal fees from Heron, personal fees from Medtronic, personal fees from Otsuka, personal fees from Pfizer, grants and personal fees from Seattle Genetics, personal fees from UpToDate, personal fees from Welvie, grants from American Cancer Society, grants from Duke University, grants from NINR/NIH, grants from Jazz Pharmaceuticals, outside the submitted work. Ms. Chan has received assistantship, and scholarship from University of North Carolina at Chapel Hill outside the submitted work. Ms. Richardson has provided consulting for Roche/Ventana outside the submitted work. Dr. Foster has received grants from Celgene, grants from MacroGenics, grants from Bellicum Pharmaceuticals, other from Daiichi-Sankyo, outside the submitted work. Dr. Dudley has received consultation fee from Carevive Systems, Inc. during the conduct of the study. Ms. Owenby and Dr. Wujcik are employed by Carevive System, Inc. during the conduct of the study. Dr. Albrecht and Ms. Dang have no conflict of interest to disclose.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bryant, A.L., LeBlanc, T.W., Albrecht, T. et al. Oral adherence in adults with acute myeloid leukemia (AML): results of a mixed methods study. Support Care Cancer 28, 5157–5164 (2020). https://doi.org/10.1007/s00520-020-05349-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05349-5