Abstract
Background
Congenital anomalies of the kidney and urinary tract (CAKUT) is associated with a slower progression to end-stage renal disease (ESRD) in pre-dialysis patients. However, little is known about the associated mortality risks after transitioning to dialysis.
Methods
This retrospective cohort study included 0–21 year-old incident dialysis patients from the United States Renal Data System starting dialysis between 1995 and 2016. We examined the association of CAKUT vs. non-CAKUT with all-cause mortality, using Cox regression adjusted for case mix variables. We also examined the mortality risk associated with 14 non-CAKUT vs. CAKUT ESRD etiologies and under stratification by estimated glomerular filtration rate (eGFR).
Results
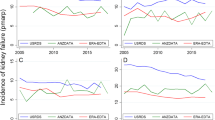
Among 25,761 patients, the median (interquartile range) age was 17 (11–19) years, and 4780 (19%) had CAKUT. CAKUT was associated with lower mortality, with an adjusted hazard ratio (aHR) of 0.72 (95%CI, 0.64–0.81) (reference: non-CAKUT). In age-stratified analyses, CAKUT vs. non-CAKUT aHRs (95%CI) were 0.66 (0.54–0.80), 0.56 (0.39–0.80), 0.66 (0.50–0.86), and 0.97 (0.80–1.18) among patients < 6, 6–< 13, 13–< 18, and ≥ 18 years at dialysis initiation, respectively. Among non-CAKUT ESRD etiologies, the risk of mortality associated with primary glomerulonephritis (aHR, 0.93; 95%CI 0.80–1.09) and focal segmental glomerulosclerosis (aHR, 0.89; 95%CI, 0.75–1.04) were comparable or slightly lower compared to CAKUT, whereas most other primary causes were associated with higher mortality risk. While the CAKUT group had lower mortality risk compared to the non-CAKUT group patients with eGFR ≥5 mL/min/1.73m2, CAKUT was associated with higher mortality in patients with eGFR < 5 mL/min/1.73 m2.
Conclusions
CAKUT is associated with lower mortality among children < 18 years old, but showed comparable mortality with non-CAKUT among patients ≥ 18 years old. ESRD etiology should be considered in risk assessment for children initiating dialysis.






Similar content being viewed by others
References
Ingelfinger JR, Kalantar-Zadeh K, Schaefer F; World Kidney Day Steering Committee (2016) Averting the legacy of kidney disease--focus on childhood. Kidney Int 89:512–518. https://doi.org/10.1016/j.kint.2015.10.014
Harambat J, van Stralen KJ, Kim JJ, Tizard EJ (2012) Epidemiology of chronic kidney disease in children. Pediatr Nephrol 27:363–373. https://doi.org/10.1007/s00467-011-1939-1
Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group (2013) KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl 3:1–150
Calderon-Margalit R, Golan E, Twig G, Leiba A, Tzur D, Afek A, Skorecki K, Vivante A (2018) History of childhood kidney disease and risk of adult end-stage renal disease. N Engl J Med 378:428–438. https://doi.org/10.1056/NEJMoa1700993
Chao SM, Saw AH, Yap HK, Tan SP, Murugasu B, Tay AH (1991) Comparison of progression of renal failure in children with hypoplastic-dysplastic kidneys and chronic glomerulonephritis. Singap Med J 32:304–306
Soares CM, Diniz JS, Lima EM, Silva JM, Oliveira GR, Canhestro MR, Colosimo EA, Simoes e Silva AC, Oliveira EA (2008) Clinical outcome of children with chronic kidney disease in a pre-dialysis interdisciplinary program. Pediatr Nephrol 23:2039–2046. https://doi.org/10.1007/s00467-008-0868-0
Sanna-Cherchi S, Ravani P, Corbani V, Parodi S, Haupt R, Piaggio G, Innocenti ML, Somenzi D, Trivelli A, Caridi G, Izzi C, Scolari F, Mattioli G, Allegri L, Ghiggeri GM (2009) Renal outcome in patients with congenital anomalies of the kidney and urinary tract. Kidney Int 76:528–533. https://doi.org/10.1038/ki.2009.220
Matsell DG, Cojocaru D, Matsell EW, Eddy AA (2015) The impact of small kidneys. Pediatr Nephrol 30:1501–1509. https://doi.org/10.1007/s00467-015-3079-5
Wuhl E, van Stralen KJ, Verrina E, Bjerre A, Wanner C, Heaf JG, Zurriaga O, Hoitsma A, Niaudet P, Palsson R, Ravani P, Jager KJ, Schaefer F (2013) Timing and outcome of renal replacement therapy in patients with congenital malformations of the kidney and urinary tract. Clin J Am Soc Nephrol 8:67–74. https://doi.org/10.2215/CJN.03310412
Vidal E, van Stralen KJ, Chesnaye NC, Bonthuis M, Holmberg C, Zurowska A, Trivelli A, Da Silva JEE, Herthelius M, Adams B, Bjerre A, Jankauskiene A, Miteva P, Emirova K, Bayazit AK, Mache CJ, Sanchez-Moreno A, Harambat J, Groothoff JW, Jager KJ, Schaefer F, Verrina E, ESPN/ERA-EDTA Registry (2017) Infants requiring maintenance dialysis: outcomes of hemodialysis and peritoneal dialysis. Am J Kidney Dis 69:617–625. https://doi.org/10.1053/j.ajkd.2016.09.024
Schwartz GJ, Feld LG, Langford DJ (1984) A simple estimate of glomerular filtration rate in full-term infants during the first year of life. J Pediatr 104:849–854
Schwartz GJ, Munoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL (2009) New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20:629–637. https://doi.org/10.1681/ASN.2008030287
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF III, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J, CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration) (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150:604–612
Austin PC (2009) Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med 28:3083–3107. https://doi.org/10.1002/sim.3697
Austin PC (2011) Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharm Stat 10:150–161. https://doi.org/10.1002/pst.433
Fine JP, Gray RJ (1999) A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 94:496–509. https://doi.org/10.1080/01621459.1999.10474144
Atkinson MA, Oberai PC, Neu AM, Fivush BA, Parekh RS (2010) Predictors and consequences of higher estimated glomerular filtration rate at dialysis initiation. Pediatr Nephrol 25:1153–1161. https://doi.org/10.1007/s00467-010-1459-4
Stel VS, Dekker FW, Ansell D, Augustijn H, Casino FG, Collart F, Finne P, Ioannidis GA, Salomone M, Traynor JP, Zurriaga O, Verrina E, Jager KJ (2009) Residual renal function at the start of dialysis and clinical outcomes. Nephrol Dial Transplant 24:3175–3182. https://doi.org/10.1093/ndt/gfp264
Kazmi WH, Gilbertson DT, Obrador GT, Guo H, Pereira BJ, Collins AJ, Kausz AT (2005) Effect of comorbidity on the increased mortality associated with early initiation of dialysis. Am J Kidney Dis 46:887–896. https://doi.org/10.1053/j.ajkd.2005.08.005
Okuda Y, Soohoo M, Tang Y, Obi Y, Laster M, Rhee CM, Streja E, Kalantar-Zadeh K (2019) Estimated GFR at dialysis initiation and mortality in children and adolescents. Am J Kidney Dis 73:797–805. https://doi.org/10.1053/j.ajkd.2018.12.038
Alexander RT, Foster BJ, Tonelli MA, Soo A, Nettel-Aguirre A, Hemmelgarn BR, Samuel SM, of the Pediatric Renal Outcomes Group Canada (2012) Survival and transplantation outcomes of children less than 2 years of age with end-stage renal disease. Pediatr Nephrol 27:1975–1983. https://doi.org/10.1007/s00467-012-2195-8
Mitsnefes MM, Laskin BL, Dahhou M, Zhang X, Foster BJ (2013) Mortality risk among children initially treated with dialysis for end-stage kidney disease, 1990-2010. JAMA 309:1921–1929. https://doi.org/10.1001/jama.2013.4208
Warady BA, Chadha V (2007) Chronic kidney disease in children: the global perspective. Pediatr Nephrol 22:1999–2009. https://doi.org/10.1007/s00467-006-0410-1
Mitsnefes MM (2005) Cardiovascular morbidity and mortality in children with chronic kidney disease in North America: lessons from the USRDS and NAPRTCS databases. Perit Dial Int 25(Suppl 3):S120–S122
Tsai TC, Chen YC, Lo CW, Wang WS, Lo SS, Tang GJ, Thien PF (2014) Incidence and renal survival of ESRD in the young Taiwanese population. Clin J Am Soc Nephrol 9:302–309. https://doi.org/10.2215/CJN.12761212
Orr NI, McDonald SP, McTaggart S, Henning P, Craig JC (2009) Frequency, etiology and treatment of childhood end-stage kidney disease in Australia and New Zealand. Pediatr Nephrol 24:1719–1726. https://doi.org/10.1007/s00467-009-1181-2
McDonald SP, Craig JC, Australian, New Zealand Paediatric Nephrology Association (2004) Long-term survival of children with end-stage renal disease. N Engl J Med 350:2654–2662. https://doi.org/10.1056/NEJMoa031643
Sule S, Fivush B, Neu A, Furth S (2012) Increased hospitalizations and death in patients with ESRD secondary to lupus. Lupus 21:1208–1213. https://doi.org/10.1177/0961203312451506
Holtta T, Bonthuis M, Van Stralen KJ, Bjerre A, Topaloglu R, Ozaltin F, Holmberg C, Harambat J, Jager KJ, Schaefer F, Groothoff JW (2016) Timing of renal replacement therapy does not influence survival and growth in children with congenital nephrotic syndrome caused by mutations in NPHS1: data from the ESPN/ERA-EDTA registry. Pediatr Nephrol 31:2317–2325. https://doi.org/10.1007/s00467-016-3517-z
Roy S, Dillon MJ, Trompeter RS, Barratt TM (1997) Autosomal recessive polycystic kidney disease: long-term outcome of neonatal survivors. Pediatr Nephrol 11:302–306
Pavkov ME, Bennett PH, Knowler WC, Krakoff J, Sievers ML, Nelson RG (2006) Effect of youth-onset type 2 diabetes mellitus on incidence of end-stage renal disease and mortality in young and middle-aged Pima Indians. JAMA 296:421–426. https://doi.org/10.1001/jama.296.4.421
Temme J, Kramer A, Jager KJ, Lange K, Peters F, Muller GA, Kramar R, Heaf JG, Finne P, Palsson R, Reisaeter AV, Hoitsma AJ, Metcalfe W, Postorino M, Zurriaga O, Santos JP, Ravani P, Jarraya F, Verrina E, Dekker FW, Gross O (2012) Outcomes of male patients with Alport syndrome undergoing renal replacement therapy. Clin J Am Soc Nephrol 7:1969–1976. https://doi.org/10.2215/CJN.02190312
Cattran DC, Rao P (1998) Long-term outcome in children and adults with classic focal segmental glomerulosclerosis. Am J Kidney Dis 32:72–79. https://doi.org/10.1053/ajkd.1998.v32.pm9669427
Ha IS, Yap HK, Munarriz RL, Zambrano PH, Flynn JT, Bilge I, Szczepanska M, Lai WM, Antonio ZL, Gulati A, Hooman N, van Hoeck K, Higuita LM, Verrina E, Klaus G, Fischbach M, Riyami MA, Sahpazova E, Sander A, Warady BA, Schaefer F, International Pediatric Peritoneal Dialysis Network Registry (2015) Risk factors for loss of residual renal function in children treated with chronic peritoneal dialysis. Kidney Int 88:605–613. https://doi.org/10.1038/ki.2015.108
Shafi T, Jaar BG, Plantinga LC, Fink NE, Sadler JH, Parekh RS, Powe NR, Coresh J (2010) Association of residual urine output with mortality, quality of life, and inflammation in incident hemodialysis patients: the choices for healthy outcomes in Caring for End-Stage Renal Disease (CHOICE) study. Am J Kidney Dis 56:348–358. https://doi.org/10.1053/j.ajkd.2010.03.020
Renkema KY, Winyard PJ, Skovorodkin IN, Levtchenko E, Hindryckx A, Jeanpierre C, Weber S, Salomon R, Antignac C, Vainio S, Schedl A, Schaefer F, Knoers NV, Bongers EM, EUCAKUT consortium (2011) Novel perspectives for investigating congenital anomalies of the kidney and urinary tract (CAKUT). Nephrol Dial Transplant 26:3843–3851. https://doi.org/10.1093/ndt/gfr655
Layton JB, Hogan SL, Jennette CE, Kenderes B, Krisher J, Jennette JC, McClellan WM (2010) Discrepancy between medical evidence form 2728 and renal biopsy for glomerular diseases. Clin J Am Soc Nephrol 5:2046–2052. https://doi.org/10.2215/CJN.03550410
Mu Y, Chin AI, Kshirsagar AV, Bang H (2018) Data concordance between ESRD medical evidence report and Medicare claims: is there any improvement? PeerJ 6:e5284. https://doi.org/10.7717/peerj.5284
Schisterman EF, Cole SR, Platt RW (2009) Overadjustment bias and unnecessary adjustment in epidemiologic studies. Epidemiology 20:488–495. https://doi.org/10.1097/EDE.0b013e3181a819a1
Acknowledgments
The data reported here have been supplied by the USRDS. The interpretation and reporting of these data are the responsibility of the authors and in no way should be seen as official policy or interpretation of the US government.
Funding
The authors are supported by the research grants from the NIH/NIDDK including T32-DK104687 (M.L.), K23-DK102903 (C.M.R), R03-DK114642 (C.M.R), K24 DK091419 (K.K. Z), U01 DK102163 (K.K. Z), and philanthropist grants from H. Simmons, L. Chang and J. Lee. Y.T. is supported by the grant from Shengjing Hospital of China Medical University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was approved by the Institutional Review Board of University of California Irvine with waiver of informed consent because the USRDS contains only deidentified information.
Conflict of interest
K.K.-Z. has received honoraria and/or support from Abbott, Abbvie, Alexion, Amgen, American Society of Nephrology, Astra-Zeneca, AVEO Oncology, Chugai, DaVita, Fresenius, Genentech, Haymarket Media, Hofstra Medical School, International Federation of Kidney Foundations, International Society of Hemodialysis, International Society of Renal Nutrition and Metabolism, Japanese Society of Dialysis Therapy, Hospira, Kabi, Keryx, Novartis, National Institutes of Health, National Kidney Foundation, OPKO, Pfizer, Relypsa, Resverlogix, Sandoz, Sanofi, Shire, Vifor, UpToDate, and ZSPharma. K.I. has received grants from Asahi Kasei Pharma, Astellas Pharma, Chugai Pharmaceutical, Fuso Pharmaceutical Industries, JMS, Novartis Pharma and Zenyaku Kogyo; personal fees from Chugai Pharmaceutical, Zenyaku Kogyo, Novartis Pharma and Vifor Pharma and other funding from Alexion Pharmaceuticals, Astellas Pharma, Novartis Pharma and Otsuka Pharmaceutical.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(PDF 564 kb)
Rights and permissions
About this article
Cite this article
Okuda, Y., Soohoo, M., Ishikura, K. et al. Primary causes of kidney disease and mortality in dialysis-dependent children. Pediatr Nephrol 35, 851–860 (2020). https://doi.org/10.1007/s00467-019-04457-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-019-04457-7