Abstract
Background
Accurately diagnosing urinary tract infections (UTI) in children with neuropathic bladders can be difficult given the lack of specificity of both clinical symptoms and routine screening tests. We aimed to identify a priori unknown classes/groups of children with neuropathic bladder with respect to symptoms and UA results and examine their relationships with odds of UTI.
Methods
We used latent class analysis (LCA) to identify unobserved classes/groups of children with neuropathic bladder based on symptoms and urinalysis (UA) results, respectively. Demographic and clinical data were gathered by retrospective chart review of a cohort with neuropathic bladder. Symptoms and UA results were obtained by chart review of visits where urine culture was ordered.
Results
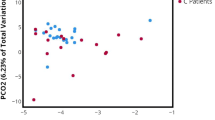
Around 193 patients were included in UA results analysis and 179 in symptom-based analysis. Two latent classes of patients were identified with respect to symptoms, labeled “pyelonephritis class” and “cystitis class,” and two, with respect to UA results, were labeled “positive UA class” and “negative UA class.” The pyelonephritis class had significantly higher odds of UTI compared to the asymptomatic class. While odds of UTI in cystitis class were higher than the asymptomatic class, this difference was not statistically significant. Positive UA class had significantly higher odds of UTI compared to negative UA class.
Conclusion
Two unobserved classes/groups exist in children with neuropathic bladder with respect to symptoms, corresponding to cystitis and pyelonephritis, and two classes of UA results that correspond with either a positive or negative UA. Our results suggest a differential approach to treatments may be considered.
Similar content being viewed by others
References
Schlager TA, Dilks S, Trudell J, Whittam TS, Hendley JO (1995) Bacteriuria in children with neurogenic bladder treated with intermittent catheterization: natural history. J Pediatr 126:490–496
Ottolini MC, Shaer CM, Rushton HG, Majd M, Gonzales EC, Patel KM (1995) Relationship of asymptomatic bacteriuria and renal scarring in children with neuropathic bladders who are practicing clean intermittent catheterization. J Pediatr 127:368–372
Madden-Fuentes R, McNamara E (2013) Variation in definitions of urinary tract infections in spina bifida patients: a systematic review. Pediatrics 132:132–139
Forster CS, Haslam DB, Jackson E, Goldstein SL (2017) Utility of a routine urinalysis in children who require clean intermittent catheterization. J Pediatr Urol 13(488):e1-488–e1-4e5
Elliott SP, Villar R, Duncan B (2005) Bacteriuria management and urological evaluation of patients with spina bifida and neurogenic bladder: a multicenter survey. J Urol 173:217–220
Ortiz TK, Velazquez N, Ding L, Routh JC, Wiener JS, Seed PC, Ross SS (2018) Predominant bacteria and patterns of antibiotic susceptibility in urinary tract infection in children with spina bifida. J Pediatr Urol 14(444):e1-444–e1-4e8
Takaba K, Shigemura K, Osawa K, Nomi M, Fujisawa M, Arakawa S (2014) Emergence of extended-spectrum β-lactamase-producing Escherichia coli in catheter-associated urinary tract infection in neurogenic bladder patients. Am J Infect Control 42:e29–e31
Groah SL, Pérez-Losada M, Caldovic L, Ljungberg IH, Sprague BM, Castro-Nallar E, Chandel NJ, Hsieh MH, Pohl HG (2016) Redefining healthy urine: a cross-sectional exploratory metagenomic study of people with and without bladder dysfunction. J Urol 196:579–587
Massa LM, Hoffman JM, Cardenas DD (2009) Validity, accuracy, and predictive value of urinary tract infection signs and symptoms in individuals with spinal cord injury on intermittent catheterization. J Spinal Cord Med 32:568–573
Collins L, Lanza S (2010) Latent class and latent transition analysis: with applications in the social, Behavioural, and health sciences. Wiley, New York
Vermunt J, Magidson J (2002) Latent class cluster analysis. Applied Latent Class Analysis, Eds J. https://doi.org/10.1017/CBO9780511499531.004
McCutcheon A (1987) Latent class analysis. Quantitative applications in the social sciences series no. 64. SAGE Publications, Thousand Oaks
Muthen B (2001) Latent variable mixture modeling. In: Marcoulides G, Schumacker R (eds) New developments and techniques in structural equation modeling. Lawrence Erlbaum Associates, Mahwah, pp 1–33
Muthen B (2002) Beyond SEM: General Latent Variable Modelind. Behaviormetrika. 29:81–117
Wang J, Wang X (2019) Structural equation modeling: applications using Mplus, 2nd edn. Wiley, New York
Hose AJ, Depner M, Illi S, Lau S, Keil T, Wahn U, Fuchs O, Pfefferle PI, Schmaußer-Hechfellner E, Genuneit J, Lauener R, Karvonen AM, Roduit C, Dalphin JC, Riedler J, Pekkanen J, von Mutius E, Ege MJ, MAS; PASTURE study groups (2017) Latent class analysis reveals clinically relevant atopy phenotypes in 2 birth cohorts. J Allergy Clin Immunol 139:1935–1945.e12
Roduit C, Frei R, Depner M, Karvonen AM, Renz H, Braun-Fahrländer C, Schmausser-Hechfellner E, Pekkanen J, Riedler J, Dalphin JC, von Mutius E, Lauener RP, the PASTURE study group, Hyvärinen A, Kirjavainen P, Remes S, Roponen M, Dalphin ML, Kaulek V, Ege M, Genuneit J, Illi S, Kabesch M, Schaub B, Pfefferle PI, Doekes G (2017) Phenotypes of atopic dermatitis depending on the timing of onset and progression in childhood. JAMA Pediatr 171:655
Forster CS, Jackson E, Ma Q, Bennett M, Shah SS, Goldstein SL (2018) Predictive ability of NGAL in identifying urinary tract infection in children with neurogenic bladders. Pediatr Nephrol 33:1365–1374. https://doi.org/10.1007/s00467-018-3936-0
Roberts KB (2011) Urinary tract infection: clinical practice guideline for the diagnosis and management of the initial UTI in febrile infants and children 2 to 24 months. Pediatrics 128:595–610
Schlager TA, Dilks SA, Lohr JA, Hayden GF, Kopco JA, Hendley JW (1992) Periurethral colonization and urinary leukocytes as markers for bacteriuria in children with neurogenic bladder. Urol Res 20:361–363
Subcommittee on Urinary Tract Infection, Steering Committee on Quality Improvement and Management, Roberts KB (2011) Urinary tract infection: clinical practice guideline for the diagnosis and Management of the Initial UTI in febrile infants and children 2 to 24 months. Pediatrics 128:595–610. https://doi.org/10.1542/peds.2011-1330
Funding
This work was partially supported by National Institutes of Health (K12-HD-001339). The funder did not have any role in either study design; data collection, interpretation, or analysis; the writing of this report; or the decision to submit this report for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest relevant.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Forster, C.S., Wang, J. Symptom- and urinalysis-based approach to diagnosing urinary tract infections in children with neuropathic bladders. Pediatr Nephrol 35, 807–814 (2020). https://doi.org/10.1007/s00467-019-04448-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-019-04448-8



