Abstract
Purpose
The purposes of this study were to analyse the correlations between the inflection point (IP) and spinal sagittal parameters and to establish the corresponding linear regressions in asymptomatic adults.
Methods
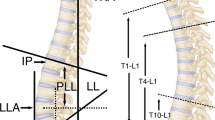
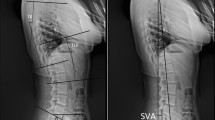
A total of 205 asymptomatic subjects older than 18 years were recruited between April 2017 and September 2019. A full-spine, standing X-ray was collected for each subject. The following parameters were documented: the IP, the apices of thoracic kyphosis (TKA) and lumbar lordosis (LLA), the distance between the plumb line of the thoracic apex (TAPL) or lumbar apex (LAPL) and gravity plumb line, thoracic kyphosis (TK), lumbar lordosis (LL) and the upper arc and the lower arc of lumbar lordosis (LLUA and LLLA, respectively). The correlations between the IP and the above parameters and between the thoracic and lumbar parameters were analysed. The level of significance was P < 0.05.
Results
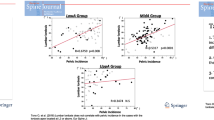
The IP was statistically correlated with age (rs = 0.327), the TKA (rs = 0.639), the TAPL (rs = 0.338), TK (rs = 0.391), the LLA (rs = 0.545), the LAPL (rs = − 0.383), the LLUA (rs = 0.371) and the LLLA (rs = − 0.145) but was not linked with LL (rs = 0.118). In addition, there were relationships between the TKA and LLA (rs = 0.397), the TAPL and LAPL (rs = − 0.357), TK and LL (rs = 0.529), TK and the LLUA (rs = 0.742) and TK and the LLLA (rs = 0.148).
Conclusion
The IP was significantly related to spinal sagittal alignment in asymptomatic adults. Moreover, predictive formulae for sagittal parameters as a function of the IP were developed, which are helpful for surgeons in comprehending the regulatory mechanisms of spinal sagittal alignment and designing an ideal therapeutic plan.
Graphic abstract
These slides can be retrieved under Electronic Supplementary Material.







Similar content being viewed by others
References
Vialle R, Levassor N, Rillardon L et al (2005) Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J Bone Joint Surg Am 87(2):260–267
Glassman SD, Berven S, Bridwell K et al (2005) Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine 30(6):682–688
Schwab FJ, Blondel B, Bess S et al (2013) Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine 38(13):E803–E812
Le Huec JC, Thompson W, Mohsinaly Y et al (2019) Sagittal balance of the spine. Eur Spine J 28(9):1889–1905
Roussouly P, Pinheiro-Franco JL (2011) Sagittal parameters of the spine: biomechanical approach. Eur Spine J 20(Suppl 5):578–585
Berthonnaud E, Dimnet J, Roussouly P et al (2005) Analysis of the sagittal balance of the spine and pelvis using shape and orientation parameters. J Spinal Disord Tech 18(1):40–47
Roussouly P, Gollogly S, Berthonnaud E et al (2005) Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine 30(3):346–353
Yamato Y, Sato Y, Togawa D et al (2019) Differences in the geometrical spinal shape in the sagittal plane according to age and magnitude of pelvic incidence in healthy elderly individuals. J Orthop Sci. https://doi.org/10.1016/j.jos.2019.07.005
Pan C, Wang G, Sun J (2019) Correlation between the apex of lumbar lordosis and pelvic incidence in asymptomatic adult. Eur Spine J. https://doi.org/10.1007/s00586-019-06183-y
Schwab F, Lafage V, Boyce R et al (2006) Gravity line analysis in adult volunteers: age-related correlation with spinal parameters, pelvic parameters, and foot position. Spine 31(25):E959–E967
Lafage R, Obeid I, Liabaud B et al (2018) Location of correction within the lumbar spine impacts acute adjacent-segment kyphosis. J Neurosurg Spine 30(1):69–77
Lee JH, Kim KT, Lee SH et al (2016) Overcorrection of lumbar lordosis for adult spinal deformity with sagittal imbalance: comparison of radiographic outcomes between overcorrection and undercorrection. Eur Spine J 25(8):2668–2675
Harrison DE, Janik TJ, Harrison DD et al (2002) Can the thoracic kyphosis be modeled with a simple geometric shape? J Spinal Disord Tech 15(3):213–220
Vacari DA, Neves EB, Ulbricht L (2015) Comparison between methods of assessing lumbosacral curve obtained by radiographic image. Acta Ortop Bras 23(2):67–71
Mac-Thiong JM, Roussouly P, Berthonnaud E et al (2011) Age- and sex-related variations in sagittal sacropelvic morphology and balance in asymptomatic adults. Eur Spine J 20(Suppl 5):572–577
Barrey C, Jund J, Noseda O et al (2007) Sagittal balance of the pelvis-spine complex and lumbar degenerative diseases. A comparative study about 85 cases. Eur Spine J 16(9):1459–1467
Giglio CA, Volpon JB (2007) Development and evaluation of thoracic kyphosis and lumbar lordosis during growth. J Child Orthop 1(3):187–193
Voutsinas SA, MacEwen GD (1986) Sagittal profiles of the spine. Clin Orthop Relat Res 210:235–242
Roussouly P, Pinheiro-Franco JL (2011) Biomechanical analysis of the spino-pelvic organization and adaptation in pathology. Eur Spine J 20(Suppl 5):609–618
Jun HS, Kim JH, Ahn JH et al (2016) The effect of lumbar spinal muscle on spinal sagittal alignment. Neurosurgery 79(6):847–855
Acknowledgements
The authors thank the Department of Imaging in Shandong provincial hospital, for providing the image data of patients.
Funding
This article did not receive any funding and grants.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
There was no conflict of interest.
Informed consent
All authors were consent to the author sequence.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Pan, C., Wang, G., Sun, J. et al. Correlations between the inflection point and spinal sagittal alignment in asymptomatic adults. Eur Spine J 29, 2272–2280 (2020). https://doi.org/10.1007/s00586-020-06360-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-020-06360-4