Abstract
Background
To investigate the relationship between unexplained indirect hyperbilirubinemia of Vietnamese newborns and the polymorphism of the promoter TATA box and exon 1 of bilirubin uridine diphosphate glucuronosyltransferase (UGT1A1) gene.
Methods
A total of 149 neonates were divided into the hyperbilirubinemia group (n = 99) and control group (n = 50). The gene polymorphisms of UGT1A1 gene in the two groups were detected by PCR and direct sequencing, which revealed the relationship between UGT1A1 polymorphism with neonatal hyperbilirubinemia of neonates. The types of UGT1A1 polymorphism in the hyperbilirubinemia group and the peak total serum bilirubin (PSB) levels with different genotypes were observed.
Results
(1) (TA)7 insertion mutation, 211G>A, 189C>T, 190G>A, 378C>T and 686C>A were detected. (2) The allele frequency of 211G>A allele mutation was significantly different between the two groups (p < 0.05). (3) Logistic regression analysis showed that homozygosity and heterozygosity of 211G>A were both significantly associated with neonatal hyperbilirubinemia. (4) In the hyperbilirubinemia group, the peak total serum bilirubin level of 211G>A homozygous neonates was higher than that of the wild-type neonates (p < 0.05).
Conclusions
We noted that there was an association between neonates with unexplained indirect hyperbilirubinemia in Vietnam and the polymorphism of UGT1A1c.211G>A. In addition, the homozygous 211G>A polymorphism was related to the degree of hyperbilirubinemia.
Impact
-
Our article provided data on UGT1A1 polymorphism distribution in the Vietnamese population, which have not been reported yet.
-
Our findings revealed that mutations in UGT1A1 gene are risk factors for unexplained hyperbilirubinemia in Vietnamese neonates.
-
Our article will strengthen the cognition of neonatal jaundice at the genetic level in the pediatric field in Vietnam.
Similar content being viewed by others
Introduction
Neonatal hyperbilirubinemia is one of the most common clinical manifestations in the neonatal period caused by the combination of catabolism of hemoglobin and physiologic immaturity of the liver in bilirubin conjugation and excretion. Uridine diphosphate glucuronosyltransferase 1A1 (UGT1A1) is expressed mainly in the liver and is an important metabolic enzyme in the bilirubin metabolism pathway. In recent years, several scholars have concentrated on hyperbilirubinemia caused by the decreased enzymatic activity or defect caused by the mutation of UGT1A1 gene. A previous study have found that the polymorphism of different genotypes of UGT1A1 may lead to the decrease of UGT1A1 gene expression or enzymatic activity.1,2,3 To date, >150 functional polymorphisms have been identified on the UGT1A locus, and 113 functional variants have been identified specifically in UGT1A1.4 A number of these variants were associated with a decrease in the UGT1A1 metabolic function. Another research showed that the most common polymorphism of UGT1A1 gene in Caucasians is the insertion of an extra TA into the normal sequence A(TA)6TAA of the promoter TATA box, demonstrating that (TA)6TAA becomes (TA)7TAA (UGT1A1*28).5 However, the most frequent polymorphism of UGT1A1 in Asian population is a non-synonymous single-nucleotide polymorphism (SNP), G-to-A at nucleotide 211, causing substitution of glycine to arginine at amino acid position 71 of exon 1 of UGT1A1 gene (UGT1A1*6 or G71R).6,7 Thus there are significant differences in polymorphic sites of UGT1A1 gene related to neonatal hyperbilirubinemia between different races or regions.
Vietnam also has a high incidence of neonatal hyperbilirubinemia. At present, there are no national statistics on the incidence of neonatal hyperbilirubinemia in Vietnam; however, according to data collected from the Vietnam National Hospital of Pediatrics (Hanoi, Vietnam), with respect to tertiary referral hospital for >31 million people in northern Vietnam, hyperbilirubinemia is responsible for 18% of neonatal admissions in 2002.8 Numerous causes of neonatal hyperbilirubinemia have been reported, and the most common causes were found to be ABO and rhesus (Rh) incompatibility, glucose-6-phosphate dehydrogenase (G6PD) deficiency, and neonatal sepsis, while in a variety of cases, the cause has still remained elusive. We therefore hypothesized that the etiology of these unexplained indirect hyperbilirubinemia may be related to heredity, particularly the polymorphisms of UGT1A1. The relationship between polymorphisms of UGT1A1 and neonatal hyperbilirubinemia in the Vietnamese population has still remained obscure. We, for the first time, attempted to find out the genetic association between hyperbilirubinemia and polymorphisms of UGT1A1 in Vietnamese newborns. The purpose of this study is to explore the distribution frequency of UGT1A1 gene polymorphism in the Vietnamese population and to evaluate correlations between UGT1A1 gene polymorphism and unexplained indirect hyperbilirubinemia among neonates.
Methods
Study subjects
This is a case–control study and 149 Vietnamese full-term newborns were recruited into this study after obtaining informed consent from their parents. All infants were born and treated in Binh Thuan General Hospital (Binhthuan, Vietnam) between January 2017 and June 2018 (range of infants’ age, 2–14 days; range of infants’ body weight at birth, 2.5–4.0 kg). All infants were divided into two groups, including hyperbilirubinemia group (n = 99 cases) and control group (n = 50), according to the presence or absence of hyperbilirubinemia. The diagnosis standard of neonatal hyperbilirubinemia was performed on the basis of the guidelines of the American Academy of Pediatrics published in 2004.9 The hyperbilirubinemia group included 99 neonates with unexplained unconjugated hyperbilirubinemia (total serum bilirubin level above the 95th percentile of Bhutani nomogram).9 The control group comprised of 50 neonates without hyperbilirubinemia (total serum bilirubin level below the 40th percentile of Bhutani nomogram9). The peak total serum bilirubin (PSB) was the highest serum concentration of bilirubin detected prior to initiation of phototherapy. Patients with maternal disease, ABO and Rh incompatibility, hemolytic anemia, G6PD deficiency, infection, asphyxia, cephalohematoma, hypothyroidism, or liver disease that would affect the total serum bilirubin level were excluded. These conditions were evaluated by means of history, clinical, and laboratory examinations such as full blood cell count, reticulocyte count, blood group and subgroups, Coombs test, G6PD activity, liver function tests, thyroid-stimulating hormone, and total T4.
DNA extraction
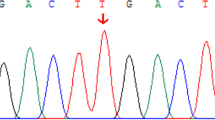
DNA was extracted from 2 mL venous blood using the TIANamp Genomic DNA Kit (TIANGEN Biotechnology Co., Ltd., Beijing, China) and was stored in a refrigerator at −20 °C. According to the sequence and flank structure of the promoter TATA box and exon 1 of UGT1A1 gene, the primers were designed and manufactured by Sangon Biotech Co., Ltd. (Shanghai, China). The fragment containing the TATA box of the UGT1A1 gene promoter was amplified by polymerase chain reaction (PCR) with a sense primer (5′-ACTGTTGTTGCCTATTAAGAAACCTAATAAAG-3′) and an antisense primer (5′-ACAACTATTTCATGTCCCCTCTGC-3′), and the PCR product had a size of 376 bp. The fragment containing the exon 1 of UGT1A1 gene was amplified by PCR with a sense primer (5′-TGGGAAGATACTGTTGATCCCAGTGGA-3′) and an antisense primer (5′-TGATGCCAAAGACAGACTCAAAC-3′), and the PCR product had a size of 949 bp. Fragment 1 (TATA box) was amplified under the following conditions: initial predenaturation at 95 °C for 5 min; 35 cycles of denaturation at 94 °C for 30 s, annealing at 60 °C for 30 s, extension at 72 °C for 30 s, and final extension at 72 °C for 5 min. Fragment 2 (exon 1) was amplified under the following conditions: initial predenaturation at 95 °C for 5 min; 35 cycles of denaturation at 94 °C for 60 s, annealing at 60 °C for 60 s, extension at 72 °C for 60 s, and final extension at 72 °C for 8 min. The PCR products were analyzed by 2% agarose gel (DOC2000, Bio-Rad Laboratories Inc., Hercules, CA, USA) electrophoresis and were sequenced by the first-generation sequencing approach (Sangon Biotech Co., Ltd., Shanghai, China).
Statistical analysis
Data were analyzed by the SPSS 16. 0 software (IBM, Armonk, NY, USA). The analysis of continuous data was undertaken by independent samples t test, and the data were expressed as mean ± standard deviation (SD). To compare the qualitative data (e.g., the frequency of genotypes and alleles), Chi-square test or Fisher’s exact test was applied. Logistic regression analysis was performed to identify the risk factors for neonatal hyperbilirubinemia in Vietnamese population, in which multivariate (adjusted) odds ratio (ORs) and 95% confidence intervals (CIs) for hyperbilirubinemia were estimated. Subgroup analysis was conducted to evaluate the effects of different polymorphisms of UGT1A1 gene on serum bilirubin peak level. Besides, p < 0.05 was considered statistically significant.
Results
Allele and genotype frequency
Among the 149 neonates, we detected that 43 infants carried heterozygote genotype of 211G>A polymorphism, 8 infants carried homozygous genotypes of 211G>A polymorphism, 12 infants were of (TA)7/6 heterozygous genotypes, and 2 infants were of (TA)7/7 homozygous genotype. In addition, the following rare polymorphisms: five 189C>T heterozygous carriers, one 190G>A heterozygous carriers, one 378C>T heterozygous carriers, and one 686C>A heterozygous carrier, were detected in this study. These rare polymorphisms were all combined with 211G>A polymorphisms or (TA)7 polymorphisms to form the compound heterozygous variant of UGT1A1. As shown in Table 1, no significant difference was noted in infants’ gender, birth weight, and feeding between the two groups (all p > 0.05). Among the eight infants with 211G>A homozygous genotype, two infants also carried the 189C>T heterozygous mutation. Among the 43 infants, who carried the 211G>A heterozygous polymorphism, two infants also carried the heterozygous genotype of (TA)7 polymorphism, one infants carried 189C>T heterozygous polymorphism, one infant carried the 190G>A heterozygous polymorphism, and one infant carried the 378C>T heterozygous polymorphism. Among the 12 infants with TA7 mutant heterozygotes, 1 infant carried 686C>A heterozygous polymorphism. The distribution of polymorphisms in UGT1A1 gene in the two groups is as noted below.
There were 43 cases of A/G and 8 cases of A/A among 149 neonates. “A” that represents allele frequency in the hyperbilirubinemia group (27.3%) was significantly higher than that in the control group (5.0%; p < 0.01; Table 2). In contrast, there was no statistically significant difference in the allele frequency of UGT1A1*28 between the hyperbilirubinemia group and the control group (5.1% and 6.0%, respectively; p > 0.05; Table 2). Similarly, there was no statistically significant difference in the allele frequency of 189C>T between the hyperbilirubinemia group and the control group (2.5% and 0%, respectively; p > 0.05; Table 2).
Only one 190G>A heterozygous carrier, one 378C>T heterozygous carrier, and one 686C>A heterozygous carrier were identified in the study group, while none of these polymorphisms could be identified in the control group. Therefore, statistical analysis was not possible for comparing such cases.
Risk factor of neonatal hyperbilirubinemia
Logistic regression was carried out to analyze the influences of a mutant TATA box with an additional TA insertion, A(TA)7TAA, coding region 211G>A and 189C>T polymorphism, and the risk of hyperbilirubinemia on Vietnamese population.
Logistic regression analysis showed that 211G>A homozygosity and heterozygosity were both significantly associated with neonatal hyperbilirubinemia. However, no association was found between (TA)7 insertion mutation and neonatal hyperbilirubinemia, either in (TA)7/7 homozygous or (TA)6/7 heterozygous individuals. Similarly, 189C>T polymorphism (only heterozygous T/C) was not associated with risk of hyperbilirubinemia in Vietnamese newborns (Table 2)
Comparing serum bilirubin levels in neonates with different genotypes in the hyperbilirubinemia group
Among the 99 patients in the hyperbilirubinemia group, 46 cases were detected without any mutation, and the mean peak level of serum bilirubin was 263.21 ± 59.36μmol/L. According to different genotypes, the 211G>A polymorphism was divided into 8 A/A homozygous and 38 A/G heterozygous, and the serum bilirubin levels of each type were 364.2 ± 105.4 and 284.89 ± 61.0 μmol/L, respectively. The PSB levels of (TA)7/7 and (TA)7/6 were 226.7 and 273.6 ± 76.1 μmol/L, respectively. The PSBs of the 2 infants who were compound heterozygous for 211G>A and (TA)7/6, 2 infants who were compound for 211G>A homozygous and 189C>T heterozygous, 3 infants who were compound heterozygous for 211G>A and 189C>T, 1 infant who was compound heterozygous for 211G>A and 190G>A, 1 infant who was compound heterozygous for 211G>A and 378C>T, and 1 who was compound heterozygous for 686C>A and (TA)7/6 were 237.65 ± 41.51, 413.95 ± 200.6, 305.7 ± 86.27, 274.9, 301.0, and 275.5 μmol/L, respectively (Table 3). The serum bilirubin levels of the 211G>A polymorphism subgroup with homozygotes was significantly higher than that in the wild-type subgroups and the 211G>A heterozygous polymorphism subgroup (p < 0.05). Comparison of 211G>A heterozygote polymorphism subgroup with wild-type subgroup showed that there were no statistically significant differences in serum bilirubin levels (p > 0.05). In addition, no statistical differences were noted in serum bilirubin levels between the other mutant subgroups and the wild-type subgroup in the hyperbilirubinemia group (p > 0.05; Table 3).
Discussion
To date, >113 allelic variants of UGT1A1 have been reported.4 These variants were associated with diminished or absent enzymatic activity, leading to abnormalities of bilirubin metabolism, such as Gilbert’s syndrome and Crigler–Najjar syndrome (type 1 (CN1) and type 2 (CN2)), which are characterized by inherited non-hemolytic unconjugated hyperbilirubinemia. The TATA box of promoter changes in repeat number of TA dinucleotide and coding region mononucleotide replacement mutations are the two most common types of UGT1A1 gene polymorphisms.3
The incidence of polymorphisms in UGT1A1 gene varies across different regions of world. The TATA box (TA)7 mutation has an allele frequency of 26–31% in Caucasians, 42–56% in African Americans, and only 6.5–16% in Asian populations.10,11 In the present study, the allele frequency of the TA7 variant in control group was 6.0%, which is relatively lower than the data previously reported in Asian population, while it is significantly lower than that in Caucasian and African American populations, which may be due to environmental racism. The current research revealed that allele frequency of the TA7 polymorphism in the hyperbilirubinemia group and the control group was 5.1% and 6%, respectively, with no statistically significant difference between the two groups (p > 0.05). The variant (TA)7 promoter of UGT1A1 was not found as a risk factor for Vietnamese newborns as well. However, c.211G>A (UGT1A1*6) alleles of coding region of UGT1A1 is relatively common in East Asian populations (Japanese, Chinese, and Korean) compared with that in European and African individuals.6,11 The results of the present study indicated that the allele frequency of 211G>A in the control group was 5.0%, which was close to the rate reported in southern China (4.0–9.7%),12,13,14 while it is lower than that observed in northern China (14.3–14.9%),15,16 Taiwan region of China (11.0–15.6%),17,18 and Japan population (13.4–18.3%);7,19 besides, the rate that we achieved in the present study was relatively higher than Thai population20 (3.5%), as well as being significantly higher than the Indian (0.2–2.6%),21,22 American (0.7%),23 and Italian (1.2%)24 populations.
Since 1998, a series of studies have confirmed that 211G>A polymorphism is a high risk factor for the occurrence and development of neonatal hyperbilirubinemia.7,18,25,26 Therefore, we speculate that the polymorphism of UGT1A1 gene may also contribute to neonatal hyperbilirubinemia in Vietnamese population. In the current study, there was a statistically significant difference in allele frequency of 211G>A between the hyperbilirubinemia group and the non-hyperbilirubinemia group (p < 0.05). In addition, logistic regression analysis showed that 211G>A, rather than A(TA)7TAA or 189C>T, led to significant elevation of the risk of neonatal hyperbilirubinemia in Vietnam. Our findings were consistent with those previously reported in East Asia.6,7,11,18,25,26 Other SNP variants of UGT1A1, such as 190G>A, 378C>T, and 686C>A, were also detected in the present study, and the polymorphism frequency was very low. In order to indicate whether the polymorphisms have an influence on neonatal hyperbilirubinemia, further research is required. In addition, the present research revealed that the serum level of bilirubin in the homozygous c.211G>A polymorphism subgroup was significantly higher than that in the wild-type subgroups and heterozygous c.211G>A polymorphism subgroup (p < 0.05), suggesting that the homozygous 211G>A carrier may remarkably decrease enzymatic activity of UGT1A1, resulting in a higher serum bilirubin level. However, the heterozygous 211G>A polymorphism did not cause significant changes in serum bilirubin level, which is likely because the heterozygous 211G>A polymorphism could only partially impair enzymatic activity of UGT1A1, thus the influences of conjugation of indirect bilirubin was not noticeable. This result is consistent with Yamamoto et al.’s finding who found that the enzymatic activity of UGT1A1 in the homozygous 211G>A polymorphism was 32.2 ± 1.6%, while in the heterozygous 211G>A polymorphism it was 60.2 ± 3.5%.27 Although (TA)n polymorphism is considered as a risk factor for neonatal hyperbilirubinemia in Caucasian and African, most scholars agree that (TA)n polymorphism is not a risk factor for neonatal hyperbilirubinemia in the population of east Asian countries,14,17 and some studies even suggest that it is a protective factor for neonatal hyperbilirubinemia in the Asian population.28,29 The present study showed that TATA box polymorphism was not significantly associated with the occurrence and development of neonatal hyperbilirubinemia in Vietnamese population, which was consistent with the findings of other East Asian countries. The polymorphism of 189C>T(p.Asp63=) and 378C>T(p.Gly126=) are synonymous variant, and the produced amino acid sequence is not modified, thus the enzymatic activity of UGT1A1 is not decreased. This may be the reason that the PSB levels of infants with 189C>T or 378C>T polymorphism subgroups were not significantly different from that of wild-type subgroup. Although the polymorphisms 190G>A(p.Ala64Thr) and 686C>A(p.Pro229Gln) were both missense mutations, which theoretically may have led to the decreased enzymatic activity of UGT1A1,30 however, the incidence rates were too low to be analyzed. Our study only focused on the contribution of carrying the first exon or TATA box polymorphism of UGT1A1 gene to neonatal hyperbilirubinemia in the Vietnamese population. Obviously, there are other areas of UGT1A1, other genes (such as G6PD, HMOX1, BLVRA, SLCO1B1, and SLCO1B3), and other factors that can cause neonatal hyperbilirubinemia that we have not evaluated. Gene–gene interaction between UGT1A1 and G6PD has been shown to contribute to the pathogenesis of neonatal hyperbilirubinemia.31,32,33 In addition, previous studies demonstrated that there was a significant gene–environment interaction between the UGT1A1 gene coding region variation and breastfeeding to increase the risk of neonatal hyperbilirubinemia.34
At present, a high incidence of neonatal hyperbilirubinemia exists in Vietnam. Hence, it is of great significance to study the pathogenesis of neonatal hyperbilirubinemia in Vietnam. To date, genetic testing is still not emphasized in the diagnosis of neonatal hyperbilirubinemia in Vietnam. In conclusion, the present study strengthens the cognition of neonatal jaundice at the genetic level in the field of pediatric in Vietnam. However, only a small subgroup of 8 patients (out of 149 in the study group) were homozygous for the 211G>A polymorphism, indicating that there may be other environmental or genetic factors causing the disease. Therefore, further study on the pathogenesis of this disease needs to be carried out.
References
Shin, H. J. et al. Functional study of haplotypes in UGT1A1 promoter to find a novel genetic variant leading to reduced gene expression. Ther. Drug Monit. 37, 369–374 (2015).
Liu, W. et al. Genetic factors affecting gene transcription and catalytic activity of UDP-glucuronosyltransferases in human liver. Hum. Mol. Genet. 23, 5558–5569 (2014).
Kaplan, M., Hammerman, C. & Maisels, M. J. Bilirubin genetics for the nongeneticist: hereditary defects of neonatal bilirubin conjugation. Pediatrics 111, 886–893 (2003).
Strassburg, C. P. Pharmacogenetics of Gilbert’s syndrome. Pharmacogenomics 9, 703–715 (2008).
Liu, J. Y., Qu, K., Sferruzza, A. D. & Bender, R. A. Distribution of the UGT1A1*28 polymorphism in Caucasian and Asian populations in the US: a genomic analysis of 138 healthy individuals. Anticancer Drugs 18, 693–696 (2007).
Mehrad-Majd, H. et al. Effects of Gly71Arg mutation in UGT1A1 gene on neonatal hyperbilirubinemia: a systematic review and meta-analysis. J. Matern. Fetal Neonatal Med. 32, 1575–1585 (2019).
Akaba, K. et al. Neonatal hyperbilirubinemia and mutation of the bilirubin uridine diphosphate-glucuronosyltransferase gene: a common missense mutation among Japanese, Koreans and Chinese. Biochem. Mol. Biol. Int. 46, 21–26 (1998).
Khu, D. T, Le, L. T. & Partridge, J. C. Characteristics of newborns admitted for hyperbilirubinemia at a tertiary referral hospital in Northern Vietnam. In 2009 Pediatric Academic Societies Annual Meeting [Abstract] E-PAS2009:4600.7 (Pediatric Academic Societies, Baltimore, MD, 2009).
American Academy of Pediatrics Subcommittee on Hyperbilirubinemia. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics 114, 297–316 (2004).
Hall, D., Ybazeta, G., Destro-Bisol, G., Petzl-Erler, M. L. & Di Rienzo, A. Variability at the uridine diphosphate glucuronosyltransferase 1A1 promoter in human populations and primates. Pharmacogenetics 9, 591–599 (1999).
Yu, Z., Zhu, K., Wang, L., Liu, Y. & Sun, J. Association of neonatal hyperbilirubinemia with UGT1A1 gene polymorphisms: a meta-analysis. Med. Sci. Monit. 21, 3104–3114 (2015).
Gao, Z. Y., Zhong, D. N., Liu, Y., Liu, Y. N. & Wei, L. M. [Roles of UGT 1A1 gene mutation in the development of neonatal hyperbilirubinemia in Guangxi]. Zhonghua Er Ke Za Zhi 48, 646–649 (2010).
Hong, C., Danni, Z., Zongyan, G., Xiaojing, W. & Luming, W. Relationship between bilirubin uridine diphosphate-glucuronosyl transferase 1A1 gene mutation and susceptibility to neonatal jaudice. Shandong Med. J. 57, 22–25 (2017).
Wu, X. J., Zhong, D. N., Xie, X. Z., Ye, D. Z. & Gao, Z. Y. UGT1A1 gene mutations and neonatal hyperbilirubinemia in Guangxi Heiyi Zhuang and Han populations. Pediatr. Res. 78, 585–588 (2015).
Min, J., Jie, L., Caiyun, Y., Ying, L. & Xuefang, Y. Gene mutation in neonatal jaundice - mutations in UGT1A1 and OATP2 genes. Indian J. Pediatr. 83, 723–725 (2016).
Gui-ying, T., Fang-sheng, X., Feng-xia, Z., Chang-zhao, L. & Ying, H. Association of Gly71Arg mutation in gene of bilirubin uridine 5’-diphosphate-glucuronosyl transferase and neonatal jaundice. J. Appl. Clin. Pediatr. 2, 129–130+160 (2008).
Chou, H. C. et al. 211 G to a variation of UDP-glucuronosyl transferase 1A1 gene and neonatal breastfeeding jaundice. Pediatr. Res. 69, 170–174 (2011).
Huang, M. J. et al. Risk factors for severe hyperbilirubinemia in neonates. Pediatr. Res. 56, 682–689 (2004).
Kanai, M. et al. Neonatal hyperbilirubinemia and the bilirubin uridine diphosphate-glucuronosyltransferase gene: the common -3263T > G mutation of phenobarbital response enhancer module is not associated with the neonatal hyperbilirubinemia in Japanese. Pediatr. Int. 47, 137–141 (2005).
Prachukthum, S. et al. Genetic polymorphisms in Thai neonates with hyperbilirubinemia. Acta Paediatr. 98, 1106–1110 (2009).
Farheen, S. et al. Gilbert’s syndrome: high frequency of the (TA)7 TAA allele in India and its interaction with a novel CAT insertion in promoter of the gene for bilirubin UDP-glucuronosyltransferase 1 gene. World J. Gastroenterol. 12, 2269–2275 (2006).
Tiwari, P. K. et al. UGT1A1 gene variants and clinical risk factors modulate hyperbilirubinemia risk in newborns. J. Perinatol. 34, 120–124 (2014).
Watchko, J. F. et al. Complex multifactorial nature of significant hyperbilirubinemia in neonates. Pediatrics 124, e868–e877 (2009).
Travan, L. et al. Severe neonatal hyperbilirubinemia and UGT1A1 promoter polymorphism. J. Pediatr. 165, 42–45 (2014).
Sun, G., Wu, M., Cao, J. & Du, L. Cord blood bilirubin level in relation to bilirubin UDP-glucuronosyltransferase gene missense allele in Chinese neonates. Acta Paediatr. 96, 1622–1625 (2007).
Huang, C. S. et al. Relationship between bilirubin UDP-glucuronosyl transferase 1A1 gene and neonatal hyperbilirubinemia. Pediatr. Res. 52, 601–605 (2002).
Yamamoto, K., Sato, H., Fujiyama, Y., Doida, Y. & Bamba, T. Contribution of two missense mutations (G71R and Y486D) of the bilirubin UDP glycosyltransferase (UGT1A1) gene to phenotypes of Gilbert’s syndrome and Crigler-Najjar syndrome type II. Biochim. Biophys. Acta 1406, 267–273 (1998).
Zhou, Y. et al. Association of UGT1A1 variants and hyperbilirubinemia in breast-fed full-term Chinese infants. PLoS ONE 9, e104251 (2014).
Zhou, Y. et al. Quantitative trait analysis of polymorphisms in two bilirubin metabolism enzymes to physiologic bilirubin levels in Chinese newborns. J. Pediatr. 165, 1154–1160.e1151 (2014).
Sato, H., Adachi, Y. & Koiwai, O. The genetic basis of Gilbert’s syndrome. Lancet 347, 557–558 (1996).
Cappellini, M. D., Martinez di Montemuros, F., Sampietro, M., Tavazzi, D. & Fiorelli, G. The interaction between Gilbert’s syndrome and G6PD deficiency influences bilirubin levels. Br. J. Haematol. 104, 928–929 (1999).
Kaplan, M. et al. Gilbert syndrome and glucose-6-phosphate dehydrogenase deficiency: a dose-dependent genetic interaction crucial to neonatal hyperbilirubinemia. Proc. Natl Acad. Sci. USA 94, 12128–12132 (1997).
Huang, C. S., Chang, P. F., Huang, M. J., Chen, E. S. & Chen, W. C. Glucose-6-phosphate dehydrogenase deficiency, the UDP-glucuronosyl transferase 1A1 gene, and neonatal hyperbilirubinemia. Gastroenterology 123, 127–133 (2002).
Yang, H. et al. Multiple genetic modifiers of bilirubin metabolism involvement in significant neonatal hyperbilirubinemia in patients of Chinese descent. PLoS ONE 10, e0132034 (2015).
Acknowledgements
We highly appreciate the dedicated efforts by the staff of Binh Thuan General Hospital for providing the study subjects’ medical records. This study was supported by the National Natural Science Foundation of China (Grant 81460241).
Author information
Authors and Affiliations
Contributions
T.-T.N.: research design, data verification, and manuscript preparation; D.-N.Z.: providing guidance for the design of the research, revising the article critically for important intellectual content and is the guarantor for the paper; W.Z.: gene analysis; X.Y.: data recording.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Informed consent
Parents or guardians of children have been knowledgeable about all aspects of the study and agreed that their child or ward participate in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nguyen, TT., Zhao, W., Yang, X. et al. The relationship between hyperbilirubinemia and the promoter region and first exon of UGT1A1 gene polymorphisms in Vietnamese newborns. Pediatr Res 88, 940–944 (2020). https://doi.org/10.1038/s41390-020-0825-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-0825-6


