Abstract
Background
Post-hepatectomy liver failure (PHLF) represents the most frequent complication after liver surgery, and the most common cause of morbidity and mortality. Aim of the study is to identify the predictors of PHLF after mini-invasive liver surgery in cirrhosis and chronic liver disease, and to develop a model for risk prediction.
Methods
The present study is a multicentric prospective cohort study on 490 consecutive patients who underwent mini-invasive liver resection from the Italian Registry of Mini-invasive Liver Surgery (I go MILS). Retrospective additional biochemical and clinical data were collected.
Results
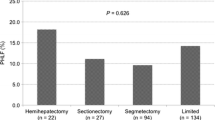
On 490 patients (26.5% females), PHLF occurred in 89 patients (18.2%). The only independent predictors of PHLF were Albumin-Bilirubin (ALBI) score (OR 3.213; 95% CI 1.661–6.215; p < .0.0001) and presence of ascites (OR 3.320; 95% CI 1.468–7.508; p = 0.004). Classification and regression tree (CART) modeling led to the identification of three risk groups: PHLF occurred in 23/217 patients with ALBI grade 1 (10.6%, low risk group), in 54/254 patients with ALBI score 2 or 3 and absence of ascites (21.3%, intermediate risk group) and in 12/19 patients with ALBI score 2 or 3 and evidence of ascites (63.2%, high risk group), p < 0.0001. The three groups showed a corresponding increase in postoperative complications (20.0%, 27.5% and 66.7%), Comprehensive Complication Index (5.1 ± 11.1, 6.0 ± 10.9 and 18.8 ± 18.9) and hospital stay (6.0 ± 4.0, 6.0 ± 6.0 and 8.0 ± 5.0 days).
Conclusion
The risk of PHLF can be stratified by determining two easily available preoperative factors: ALBI and ascites. This model of risk prediction offers an objective instrument for a correct clinical decision-making.

Similar content being viewed by others
Abbreviations
- PHLF:
-
Post-hepatectomy liver failure
- MILS:
-
Mini-invasive liver surgery
- HCC:
-
Hepatocellular carcinoma
- CCC:
-
Mass-forming cholangiocarcinoma
- ALBI:
-
Albumin-Bilirubin score
- LR:
-
Liver resection
- BMI:
-
Body Mass Index
- CART:
-
Classification and regression tree analysis
- ALPPS:
-
Associating liver partitioning and portal vein ligation for staged hepatectomy
- ISGLS:
-
International Study Group of Liver Surgery
- PH:
-
Portal hypertension
- MELD:
-
Model for end-stage liver disease
- DCC:
-
Dindo–Clavien classification
- CCI:
-
Comprehensive Complication Index
- IQR:
-
Interquartile range
- AUC:
-
Area under curve
- MCAR:
-
Missing completely at random
- CHAID:
-
Chi-square automatic interaction detector
References
Silberhumer GR, Paty PB, Temple LK et al (2015) Simultaneous resection for rectal cancer with synchronous liver metastasis is a safe procedure. Am J Surg 209:935–942
Sposito C, Di Sandro S, Brunero F et al (2016) Development of a prognostic scoring system for resectable hepatocellular carcinoma. World J Gastroenterol 22:8194–8202
Lafaro K, Buettner S, Maqsood H et al (2015) Defining post hepatectomy liver insufficiency: where do we stand? J Gastrointest Surg 19:2079–2092
van den Broek MA, Olde Damink SW, Dejong CH et al (2008) Liver failure after partial hepatic resection: definition, pathophysiology, risk factors and treatment. Liver Int 28:767–780
Skrzypczyk C, Truant S, Duhamel A et al (2014) Relevance of the ISGLS definition of posthepatectomy liver failure in early prediction of poor outcome after liver resection: study on 680 hepatectomies. Ann Surg 260:865–870
EASL-EORTC clinical practice guidelines (2012) management of hepatocellular carcinoma. J Hepatol 56:908–943
Citterio D, Facciorusso A, Sposito C et al (2016) Hierarchic interaction of factors associated with liver decompensation after resection for hepatocellular carcinoma. JAMA Surg 151:846–853
Delis SG, Bakoyiannis A, Biliatis I et al (2009) Model for end-stage liver disease (MELD) score, as a prognostic factor for post-operative morbidity and mortality in cirrhotic patients, undergoing hepatectomy for hepatocellular carcinoma. HPB (Oxford) 11:351–357
Nanashima A, Abo T, Arai J et al (2013) Functional liver reserve parameters predictive for posthepatectomy complications. J Surg Res 185:127–135
Zou H, Yang X, Li QL et al (2018) A comparative study of albumin-bilirubin score with child-pugh score, model for end-stage liver disease score and indocyanine green R15 in predicting posthepatectomy liver failure for hepatocellular carcinoma patients. Dig Dis 36:236–243
European Association for the Study of the Liver (2018) EASL clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol 69:182–236
Morise Z, Ciria R, Cherqui D et al (2015) Can we expand the indications for laparoscopic liver resection? A systematic review and meta-analysis of laparoscopic liver resection for patients with hepatocellular carcinoma and chronic liver disease. J Hepatobiliary Pancreat Sci 22:342–352
Sposito C, Battiston C, Facciorusso A et al (2016) Propensity score analysis of outcomes following laparoscopic or open liver resection for hepatocellular carcinoma. Br J Surg 103:871–880
Han HS, Shehta A, Ahn S et al (2015) Laparoscopic versus open liver resection for hepatocellular carcinoma: case-matched study with propensity score matching. J Hepatol 63:643–650
Aldrighetti L, Guzzetti E, Pulitano C et al (2010) Case-matched analysis of totally laparoscopic versus open liver resection for HCC: short and middle term results. J Surg Oncol 102:82–86
Cheung TT, Dai WC, Tsang SH et al (2016) Pure laparoscopic hepatectomy versus open hepatectomy for hepatocellular carcinoma in 110 patients with liver cirrhosis: a propensity analysis at a single center. Ann Surg 264:612–620
Morise Z (2015) Perspective of laparoscopic liver resection for hepatocellular carcinoma. World J Gastrointest Surg 7:102–106
Aldrighetti L, Ratti F, Cillo U et al (2017) Diffusion, outcomes and implementation of minimally invasive liver surgery: a snapshot from the I Go MILS (Italian Group of Minimally Invasive Liver Surgery) Registry. Updates Surg 69:271–283
Rahbari NN, Garden OJ, Padbury R et al (2011) Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery 149:713–724
Bruix J, Sherman M (2011) Management of hepatocellular carcinoma: an update. Hepatology 53:1020–1022
Malinchoc M, Kamath PS, Gordon FD et al (2000) A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology 31:864–871
Johnson PJ, Berhane S, Kagebayashi C et al (2015) Assessment of liver function in patients with hepatocellular carcinoma: a new evidence-based approach-the ALBI grade. J Clin Oncol 33:550–558
Pang YY (2000) The Brisbane 2000 terminology of liver anatomy and resections. HPB 2:333–339. (HPB (Oxford) 2002; 4:99–100)
Kawaguchi Y, Fuks D, Kokudo N et al (2018) Difficulty of laparoscopic liver resection: proposal for a new classification. Ann Surg 267:13–17
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Slankamenac K, Nederlof N, Pessaux P et al (2014) The comprehensive complication index: a novel and more sensitive endpoint for assessing outcome and reducing sample size in randomized controlled trials. Ann Surg 260:757–762
Rubin DB (1987) Multiple imputation for nonresponse in surveys. Wiley, New York
Harper PR (2005) A review and comparison of classification algorithms for medical decision making. Health Policy 71:315–331
Cescon M, Colecchia A, Cucchetti A et al (2012) Value of transient elastography measured with FibroScan in predicting the outcome of hepatic resection for hepatocellular carcinoma. Ann Surg 256:706–712
Cipriani F, Fantini C, Ratti F et al (2018) Laparoscopic liver resections for hepatocellular carcinoma: can we extend the surgical indication in cirrhotic patients? Surg Endosc 32:617–626
Berardi G, Van CS, Fretland AA et al (2017) Evolution of laparoscopic liver surgery from innovation to implementation to mastery: perioperative and oncologic outcomes of 2,238 patients from 4 European Specialized Centers. J Am Coll Surg 225:639–649
Andreatos N, Amini N, Gani F et al (2017) Albumin-bilirubin score: predicting short-term outcomes including bile leak and post-hepatectomy liver failure following hepatic resection. J Gastrointest Surg 21:238–248
Acknowledgements
The authors thank The Italian Group of MILS (I Go MILS) registry and all collaborators who equally contributed to this work.
All Collaborators of the I Go MILS Group listed below are coworkers of the study and contributed to acquisition of data, article review for intellectual content and final approval of the version to be published:
Adelmo Antonucci (Policlinico di Monza, Monza, Italy, e-mail: adelmo.antonucci@policlinicodimonza.it), Francesco Ardito (A. Gemelli, IRCCS, Catholic University of the Sacred Heart, Rome, Italy, e-mail: francesco.ardito@unicatt.it), Carlo Battiston (Fondazione IRCCS Istituto Nazionale Tumori di Milano, Milan, Italy, e-mail: carlo.battiston@istitutotumori.mi.it), Giulio Belli (SM Loreto Nuovo Hospital, Naples, Italy, e-mail: giubelli@unina.it), Stefano Berti (Ospedale Civile S. Andrea, La Spezia, Italy, e-mail: stefano.berti@asl5.liguria.it), Ugo Boggi (AOU Pisana, Pisa, Italy, e-mail: u.boggi@med.unipi.it), Alberto Brolese (S. Chiara Hospital, Trento, Italy, e-mail: alberto.brolese@apss.tn.it), Fulvio Calise (Pinetagrande hospital, Castel Volturno, Italy, e-mail: fulvio.calise@aocardarelli.it), Graziano Ceccarelli, (San Donato Hospital, Arezzo, Italy, e-mail: graziano.ceccarelli@usl8.toscana.it), Michele Colledan (AO Papa Giovanni XXIII, Bergamo, Italy, e-mail: mcolledan@asst-pg23.it), Andrea Coratti (AOU Careggi, Florence, Italy, e-mail: corattia@aou-careggi.toscana.it), Stefano Di Sandro (ASST Grande Ospedale Metropolitano Niguarda, Milan, Italy, e-mail: stefano.disandro@ospedaleniguarda.it), Ludovica Ferrara (University of Parma, Parma, Italy), Antonio Floridi (AO Ospedale Maggiore, Crema, Italy), Antonio Frena (Central Hospital, Bolzano, Italy, e-mail: antonio.frena@asbz.it), Antonio Giuliani, (AO R. N. Cardarelli, Naples, Italy), Gian Luca Grazi (Istituto Nazionale Tumori Regina Elena, Rome, Italy, e-mail: glgrazi@chirurgiadelfegato.it), Enrico Gringeri (University of Padua, Padova, Italy, e-mail: enrico.gringeri@unipd.it), Guido Griseri (San Paolo Hospital, Savona, Italy, e-mail: g.griseri@asl2.liguria.it), Salvatore Gruttadauria (Mediterranean Institute for Transplantation and Specialization Therapies IRCCS-ISMETT, Palermo, Italy, e-mail: sgruttadauria@ismett.edu), Silvio Guerriero (San Martino Hospital, Belluno, Italy, e-mail: silvio.guerriero@ulss.belluno.it), Elio Jovine (Ospedale Maggiore, Bologna, Italy, e-mail: elio.jovine@ausl.bologna.it), Giovanni Battista Levi Sandri (S. Camillo Hospital, Rome, Italy, e-mail: gblevisandri@gmail.com), Paolo Magistri (University of Modena and Reggio Emilia, Italy, e-mail: paolo.magistri@unimore.it), Pietro Maida (Villa Betania Hospital, Napoli, Italy), Pietro Mezzatesta (Casa di Cura La Maddalena, Palermo, Italy, e-mail: mezzatesta@lamaddalenanet.it), Giuseppe Navarra (AOU Policlinico G. Martino, Messina, Italy, e-mail: giuseppe.navarra@polime.it), Amilcare Parisi (AO Santa Maria di Terni, Terni, Italy, e-mail: a.parisi@ospterni.it), Antonio Pinna (Digestive Disease Institute at Cleveland Clinic Abu Dhabi), Francesca Ratti, (IRCCS San Raffaele Hospital, Milan, Italy, e-mail: ratti.francesca@hsr.it), Paolo Reggiani, (IRCCS Ospedale Maggiore Policlinico di Milano, Milan, Italy, e-mail: paolo.reggiani@policlinico.mi.it), Raffaele Romito (Ospedale Maggiore Novara, Italy, e-mail: raffele.romito@maggioreosp.novara.it), Andrea Ruzzenente (University of Verona, Italy, e-mail: andrea.ruzzenente@univr.it), Nadia Russolillo (Mauriziano Umberto I Hospital, Torino, Italy, e-mail: nadia.russolillo@libero.it), Roberto Santambrogio (AO San Paolo, Milan, Italy, e-mail: roberto.santambrogio@asst-santipaolocarlo.it), Giovanni Sgroi (AO Treviglio-Caravaggio, Treviglio, Italy, e-mail: giovanni_sgroi@asst-bgovest.it), Abdallah Slim (AO Desio e Vimercate, Vimercate, Italy, e-mail: abdallah.slim@aovimercate.org), Guido Torzilli (Istituto Clinico Humanitas, Rozzano, Italy, e-mail: guido.torzilli@hunimed.eu), Leonardo Vincenti (AOU Consorziale Policlinico, Bari, Italy), Fausto Zamboni (Brotzu Hospital, Cagliari, Italy, e-mail: faustozamboni@yahoo.it).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Carlo Sposito, Michela Monteleone, Luca Aldrighetti, Umberto Cillo, Raffaele Dalla Valle, Alfredo Guglielmi, Giuseppe Maria Ettorre, Alessandro Ferrero, Fabrizio Di Benedetto, Giorgio Ettore Rossi, Luciano De Carlis, Felice Giuliante, and Vincenzo Mazzaferro have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sposito, C., Monteleone, M., Aldrighetti, L. et al. Preoperative predictors of liver decompensation after mini-invasive liver resection. Surg Endosc 35, 718–727 (2021). https://doi.org/10.1007/s00464-020-07438-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07438-2