Abstract
Purpose
To assess the longitudinal associations between maternal total bile acid (TBA) levels during early mid-pregnancy and the subsequent risk of gestational diabetes mellitus (GDM).
Methods
In a prospective cohort study, pregnant women who were enrolled prior to gestational week 16 were followed until delivery. TBA levels were tested during weeks 14–18 of gestation. Using logistic regression, we analyzed the associations between quartiles of TBA and GDM based on a 75-g oral glucose tolerance test (OGTT) at 24–28 gestational weeks.
Results
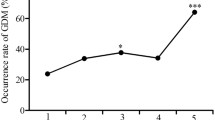
The GDM rate was 7.9% (114/1441). The mean TBA level was higher in women with GDM than in those without GDM (2.1 ± 2.0 vs 1.5 ± 1.0 µmol/L, P = 0.000). The highest TBA level quartile (2.1–10.7 µmol/L) had a 1.78-fold (95% CI 1.01, 3.14) increased risk of GDM compared with that of the lowest quartile (0.0–0.8 µmol/L) after adjusting for pre-pregnancy body mass index (BMI), gestational, age at TBA test and other confounders. High TBA levels were involved in the fasting glucose level rather than that at 1 h and 2 h after OGTT in all participants.
Conclusions
Pregnant women with higher serum TBA levels during early mid-pregnancy have a higher risk of developing GDM. TBA may be a new risk factor for GDM.
Similar content being viewed by others
References
American Diabetes Association (2010) Executive summary (2010): standards of medical care in diabetes—2010. Diabetes Care 33(Suppl 1): S4–S10
Retnakaran R et al (2008) (2008), Glucose intolerance in pregnancy and future risk of pre-diabetes or diabetes. Diabetes Care 31(10):2026–2031
Group HSCR et al (2008) Hyperglycemia and adverse pregnancy outcomes. N Engl J Med 358(19):1991–2002
Catalano PM et al (2012) The hyperglycemia and adverse pregnancy outcome study: associations of GDM and obesity with pregnancy outcomes. Diabetes Care 35(4):780–786
Kubo A et al (2014) (2014), Maternal hyperglycemia during pregnancy predicts adiposity of the offspring. Diabetes Care 37(11):2996–3002
Hou W et al (2016) Elevated first-trimester total bile acid is associated with the risk of subsequent gestational diabetes. Sci Rep 6:34070
Russell DW (2003) The enzymes, regulation, and genetics of bile acid synthesis. Annu Rev Biochem 72:137–174
Catoi AF et al (2015) Metabolic mechanisms in obesity and type 2 diabetes: insights from bariatric/metabolic surgery. Obes Facts 8(6):350–363
Ma H, Patti ME (2014) Bile acids, obesity, and the metabolic syndrome. Best Pract Res Clin Gastroenterol 28(4):573–583
Kuipers F et al (2007) Bile acids, farnesoid X receptor, atherosclerosis and metabolic control. Curr Opin Lipidol 18(3):289–297
Lefebvre P et al (2009) Role of bile acids and bile acid receptors in metabolic regulation. Physiol Rev 89(1):147–191
Haeusler RA et al (2013) Human insulin resistance is associated with increased plasma levels of 12alpha-hydroxylated bile acids. Diabetes 62(12):4184–4191
Brufau G et al (2010) Improved glycemic control with colesevelam treatment in patients with type 2 diabetes is not directly associated with changes in bile acid metabolism. Hepatology 52(4):1455–1464
Goldfine AB (2008) Modulating LDL cholesterol and glucose in patients with type 2 diabetes mellitus: targeting the bile acid pathway. Curr Opin Cardiol 23(5):502–511
Ferrannini E et al (2015) Increased bile acid synthesis and deconjugation after biliopancreatic diversion. Diabetes 64(10):3377–3385
Maghsoodi N et al (2019) Bile acid metabolism is altered in those with insulin resistance after gestational diabetes mellitus. Clin Biochem 64:12–17
Kong M et al (2018) Higher level of GGT during mid-pregnancy is associated with increased risk of gestational diabetes mellitus. Clin Endocrinol (Oxf) 88(5):700–705
Weinert LS (2010) International Association of Diabetes and Pregnancy Study Groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy: comment to the International Association of Diabetes and Pregnancy Study Groups Consensus Panel. Diabetes Care 33(7):e97 (author reply e98)
Cariou B et al (2011) Fasting plasma chenodeoxycholic acid and cholic acid concentrations are inversely correlated with insulin sensitivity in adults. Nutr Metab (Lond) 8(1):48
Shaham O et al (2008) Metabolic profiling of the human response to a glucose challenge reveals distinct axes of insulin sensitivity. Mol Syst Biol 4:214
Meng XM et al (2017) Metformin improves the glucose and lipid metabolism via influencing the level of serum total bile acids in rats with streptozotocin-induced type 2 diabetes mellitus. Eur Rev Med Pharmacol Sci 21(9):2232–2237
Prawitt J, Caron S, Staels B (2011) Bile acid metabolism and the pathogenesis of type 2 diabetes. Curr Diabetes Rep 11(3):160–166
Ding L et al (2015) Effects of preventative application of metformin on bile acid metabolism in high fat-fed/streptozotocin-diabetic rats. Int J Clin Exp Pathol 8(5):5450–5456
Martineau MG et al (2015) The metabolic profile of intrahepatic cholestasis of pregnancy is associated with impaired glucose tolerance, dyslipidemia, and increased fetal growth. Diabetes Care 38(2):243–248
Fiorucci S et al (2009) Bile-acid-activated receptors: targeting TGR5 and farnesoid-X-receptor in lipid and glucose disorders. Trends Pharmacol Sci 30(11):570–580
Sharma R, Long A, Gilmer JF (2011) Advances in bile acid medicinal chemistry. Curr Med Chem 18(26):4029–4052
Staels B, Fonseca VA (2009) Bile acids and metabolic regulation: mechanisms and clinical responses to bile acid sequestration. Diabetes Care 32(Suppl 2):S237–S245
Duran-Sandoval D et al (2004) Glucose regulates the expression of the farnesoid X receptor in liver. Diabetes 53(4):890–898
Michael MD et al (2000) Loss of insulin signaling in hepatocytes leads to severe insulin resistance and progressive hepatic dysfunction. Mol Cell 6(1):87–97
Katsuma S, Hirasawa A, Tsujimoto G (2005) Bile acids promote glucagon-like peptide-1 secretion through TGR5 in a murine enteroendocrine cell line STC-1. Biochem Biophys Res Commun 329(1):386–390
Holst JJ (2007) The physiology of glucagon-like peptide 1. Physiol Rev 87(4):1409–1439
Thomas C et al (2009) TGR5-mediated bile acid sensing controls glucose homeostasis. Cell Metab 10(3):167–177
Budak MS et al (2019) Maternal abdominal subcutaneous fat thickness as a simple predictor for gestational diabetes mellitus. J Perinat Med 47(6):605–610
Acknowledgements
The authors thank the women who participated in this study and the clinics that allowed us access to their databases.
Funding
Funding was received from the National Program on Basic Research Project of China, Ministry of Science and Technology (2013FY114200 for Nianhong Yang).
Author information
Authors and Affiliations
Contributions
NHY designed the study; MK, ZXL, CRX, XZZ, RJC, GPX, XFY and LPH researched the data; and MK drafted the manuscript. All authors approved the final version of the manuscript. NHY is the guarantor of this work and thus had full access to all study data and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
Approval was obtained from Tongji Medical College of Huazhong University of Science and Technology Committee.
Informed consent
For this type of study formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kong, M., Lu, Z., Zhong, C. et al. A higher level of total bile acid in early mid-pregnancy is associated with an increased risk of gestational diabetes mellitus: a prospective cohort study in Wuhan, China. J Endocrinol Invest 43, 1097–1103 (2020). https://doi.org/10.1007/s40618-020-01196-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-020-01196-7