Abstract
Background
Craniopharyngioma is a benign tumor that commonly develops within the suprasellar region. The tumor and treatment can have debilitating consequences for pediatric and adult patients, including vision loss and pituitary/hypothalamic dysfunction. Most craniopharyngioma series focus on treatment of the pediatric population. We evaluated the outcomes of all adult craniopharyngioma patients treated at our institution using proton therapy to report outcomes for disease control, treatment-related toxicity, and tumor response.
Methods
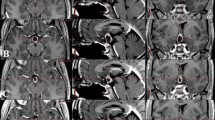
We analyzed 14 adult patients (≥ 22 years old). All patients had gross disease at the time of radiotherapy. Five were treated for de novo disease and 9 for recurrent disease. Patients received double-scattered conformal proton therapy to a mean dose of 54 GyRBE in 1.8 GyRBE/fraction (range 52.2–54 GyRBE). Weekly magnetic resonance imaging (MRI) helped to evaluate tumor changes during radiotherapy.
Results
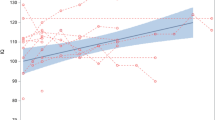
With median clinical and radiographic follow-up of 29 and 26 months, respectively, the 3-year local control and overall survival rates were both 100%. There were no grade 3 or greater acute or late radiotherapy-related side effects. There was no radiotherapy-related vision loss or optic neuropathy. No patients required intervention or treatment replanning due to tumor changes during radiotherapy. Two patients experienced transient cyst expansion at their first post-radiotherapy MRI. Both patients were followed closely clinically and radiographically and had subsequent dramatic tumor/cyst regression, requiring no interventions.
Conclusions
Our data support the safety and efficacy of proton therapy in the treatment of adult craniopharyngioma as part of primary or salvage treatment. We recommend early consideration of radiotherapy.

Similar content being viewed by others
Change history
22 March 2021
A Correction to this paper has been published: https://doi.org/10.1007/s11060-021-03740-8
References
Bunin GR, Surawicz TS, Witman PA, Preston-Martin S, Davis F, Bruner JM (1997) The descriptive epidemiology of craniopharyngioma. Neurosurg Focus 3(6):e1
Moon SH, Kim IH, Park SW et al (2005) Early adjuvant radiotherapy toward long-term survival and better quality of life for craniopharyngiomas—a study in single institute. Childs Nerv Syst 21(8–9):799–807
Harrabi SB, Adeberg S, Welzel T et al (2014) Long term results after fractionated stereotactic radiotherapy (FSRT) in patients with craniopharyngioma: maximal tumor control with minimal side effects. Radiat Oncol 9:203
Lo AC, Howard AF, Nichol A et al (2014) Long-term outcomes and complications in patients with craniopharyngioma: the British Columbia Cancer Agency experience. Int J Radiat Oncol Biol Phys 88(5):1011–1018
Regine WF, Mohiuddin M, Kramer S (1993) Long-term results of pediatric and adult craniopharyngiomas treated with combined surgery and radiation. Radiother Oncol 27(1):13–21
Merchant TE, Kun LE, Hua CH et al (2013) Disease control after reduced volume conformal and intensity modulated radiation therapy for childhood craniopharyngioma. Int J Radiat Oncol Biol Phys 85(4):e187–e192
Zhang C, Verma V, Lyden ER et al (2018) The role of definitive radiotherapy in craniopharyngioma: a SEER analysis. Am J Clin Oncol 41(8):807–812
Rao YJ, Hassanzadeh C, Fischer-Valuck B et al (2017) Patterns of care and treatment outcomes of patients with craniopharyngioma in the national cancer database. J Neurooncol 132(1):109–117
Fitzek MM, Linggood RM, Adams J, Munzenrider JE (2006) Combined proton and photon irradiation for craniopharyngioma: long-term results of the early cohort of patients treated at Harvard Cyclotron Laboratory and Massachusetts General Hospital. Int J Radiat Oncol Biol Phys 64(5):1348–1354
Puget S, Garnett M, Wray A et al (2007) Pediatric craniopharyngiomas: classification and treatment according to the degree of hypothalamic involvement. J Neurosurg 106(1 Suppl):3–12
Muller HL (2015) Craniopharyngioma: long-term consequences of a chronic disease. Expert Rev Neurother 15(11):1241–1244
Schoenfeld A, Pekmezci M, Barnes MJ et al (2012) The superiority of conservative resection and adjuvant radiation for craniopharyngiomas. J Neurooncol 108(1):133–139
Clark AJ, Cage TA, Aranda D et al (2013) A systematic review of the results of surgery and radiotherapy on tumor control for pediatric craniopharyngioma. Childs Nerv Syst 29(2):231–238
Boehling NS, Grosshans DR, Bluett JB et al (2012) Dosimetric comparison of three-dimensional conformal proton radiotherapy, intensity-modulated proton therapy, and intensity-modulated radiotherapy for treatment of pediatric craniopharyngiomas. Int J Radiat Oncol Biol Phys 82(2):643–652
Beltran C, Roca M, Merchant TE (2012) On the benefits and risks of proton therapy in pediatric craniopharyngioma. Int J Radiat Oncol Biol Phys 82(2):e281–e287
Yeung D, McKenzie C, Indelicato DJ (2014) A dosimetric comparison of intensity-modulated proton therapy optimization techniques for pediatric craniopharyngiomas: a clinical case study. Pediatr Blood Cancer 61(1):89–94
Bishop AJ, Greenfield B, Mahajan A et al (2014) Proton beam therapy versus conformal photon radiation therapy for childhood craniopharyngioma: multi-institutional analysis of outcomes, cyst dynamics, and toxicity. Int J Radiat Oncol Biol Phys 90(2):354–361
Luu QT, Loredo LN, Archambeau JO, Yonemoto LT, Slater JM, Slater JD (2006) Fractionated proton radiation treatment for pediatric craniopharyngioma: preliminary report. Cancer J 12(2):155–159
Ajithkumar T, Mazhari AL, Stickan-Verfurth M et al (2018) Proton therapy for craniopharyngioma—an early report from a single European centre. Clin Oncol (R Coll Radiol) 30(5):307–316
Lamiman K, Wong KK, Tamrazi B et al (2016) A quantitative analysis of craniopharyngioma cyst expansion during and after radiation therapy and surgical implications. Neurosurg Focus 41(6):E15
Winkfield KM, Linsenmeier C, Yock TI et al (2009) Surveillance of craniopharyngioma cyst growth in children treated with proton radiotherapy. Int J Radiat Oncol Biol Phys 73(3):716–721
Constine LS, Randall SH, Rubin P, McDonald J (1989) Craniopharyngiomas: fluctuation in cyst size following surgery and radiation therapy. Neurosurgery 24(1):53–59
Shi Z, Esiashvili N, Janss AJ et al (2012) Transient enlargement of craniopharyngioma after radiation therapy: pattern of magnetic resonance imaging response following radiation. J Neurooncol 109(2):349–355
Masson-Cote L, Masucci GL, Atenafu EG et al (2013) Long-term outcomes for adult craniopharyngioma following radiation therapy. Acta Oncol 52(1):153–158
Kim T, Flynn MR (1991) Airflow pattern around a worker in a uniform freestream. Am Ind Hyg Assoc J 52(7):287–296
Pemberton LS, Dougal M, Magee B, Gattamaneni HR (2005) Experience of external beam radiotherapy given adjuvantly or at relapse following surgery for craniopharyngioma. Radiother Oncol 77(1):99–104
Muller HL, Bruhnken G, Emser A et al (2005) Longitudinal study on quality of life in 102 survivors of childhood craniopharyngioma. Childs Nerv Syst 21(11):975–980
Van Effenterre R, Boch AL (2002) Craniopharyngioma in adults and children: a study of 122 surgical cases. J Neurosurg 97(1):3–11
Stripp DC, Maity A, Janss AJ et al (2004) Surgery with or without radiation therapy in the management of craniopharyngiomas in children and young adults. Int J Radiat Oncol Biol Phys 58(3):714–720
Kalapurakal JA, Goldman S, Hsieh YC, Tomita T, Marymont MH (2003) Clinical outcome in children with craniopharyngioma treated with primary surgery and radiotherapy deferred until relapse. Med Pediatr Oncol 40(4):214–218
Toussaint L, Indelicato DJ, Muren LP et al (2019) Temporal lobe sparing radiotherapy with photons or protons for cognitive function preservation in paediatric craniopharyngioma. Radiother Oncol 142:140–146
Gondi V, Deshmukh S, Brown PD et al (2019) NRG Oncology CC001: a phase III trial of hippocampal avoidance (HA) in addition to whole-brain radiotherapy (WBRT) plus memantine to preserve neurocognitive function (NCF) in patients with brain metastases (BM). J Clin Oncol 37(15 Suppl):2009
Brastianos PK, Shankar GM, Gill CM et al (2016) Dramatic response of BRAF V600E mutant papillary craniopharyngioma to targeted therapy. J Natl Cancer Inst. https://doi.org/10.1093/jnci/djv310
Alliance for Clinical Trials in Oncology. Vemurafenib and cobimetinib in treating patients with BRAF V600E mutation positive craniopharyngioma. https://clinicaltrials.gov/ct2/show/NCT03224767. ClinicalTrials.gov Identifier: NCT03224767. Accessed 3 Dec 2019
Author information
Authors and Affiliations
Contributions
Study design, MSR; Data Collection, MSR; Statistical Analysis, CGM; Data Interpretation, MSR, RLR, DR, ALH, DJI, SH, WMM; Drafting Manuscript, MSR; Final Approval of Manuscript, MSR, RLR, DR, ALH, DJI, SH, WMM.
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article has been revised: The Abstract has been corrected.
Electronic supplementary material
Below is the link to the electronic supplementary material.
11060_2020_3432_MOESM2_ESM.tif
Supplementary file2 (TIF 475 kb) Supplementary Fig. 1. Intensity-modulated radiation therapy (IMRT) and 3-dimensional (3D) conformal proton radiotherapy treatment plan comparison for adult craniopharyngioma. A representative case of treatment planning comparison between 7-field IMRT (left images) and 3D conformal passively scattered proton radiotherapy (right images). The planning target volume (PTV) delineated by the green line and PTV coverage is the same for both plans. Shaded colorwash shows doses ranging from 10 GyRBE to the maximum dose for each plan. Low dose (10 GyRBE in blue) and intermediate dose (30 GyRBE in teal) spread far beyond the target volume and extend further into normal brain and eyes with the IMRT plan compared to the proton plan. The prescription dose and high dose radiation (yellow and red) are similar between both treatment modalities
Rights and permissions
About this article
Cite this article
Rutenberg, M.S., Rotondo, R.L., Rao, D. et al. Clinical outcomes following proton therapy for adult craniopharyngioma: a single-institution cohort study. J Neurooncol 147, 387–395 (2020). https://doi.org/10.1007/s11060-020-03432-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-020-03432-9