Abstract
Introduction
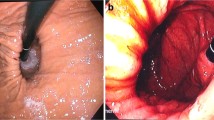
Hill’s classification provides a reproducible endoscopic grading system for esophagogastric junction morphology and competence, specifically whether the gastroesophageal flap valve (GEFV) is normal (grade I/II) or abnormal (grades III/IV). However, it is not routinely used in clinical practice. We report a systematic review and meta-analysis to determine association between abnormal GEFV and gastroesophageal reflux disorder (GERD).
Methods
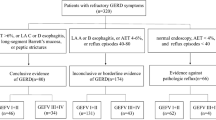
A comprehensive literature search of MEDLINE and Scopus databases was conducted to identify studies that reported the association between abnormal GEFV and GERD. The search and quality assessment were performed independently by two authors. Fixed- and random-effects meta-analyses were conducted using symptomatic GERD and erosive esophagitis as outcomes.
Results
A total of 11 studies met inclusion criteria that included a total of 5054 patients. In the general population, patients with abnormal GEFV had greater risk of symptomatic GERD compared to patients with a normal GEFV (risk ratio [RR] 1.88, 95% CI 1.57–2.24). Further, in patients with symptomatic GERD, patients with abnormal GEFV had greater risk of erosive esophagitis compared to patients with normal GEFV (RR 2.17, 95% CI 1.40–3.36). Finally, the specificity of abnormal GEFV for symptomatic GERD was 73.3% (95% CI 69.3–77.0%) and 75.7% (95% CI 65.9–83.4%) for erosive esophagitis in symptomatic GERD.
Conclusion
Our systematic review and meta-analysis showed consistent association between abnormal GEFV indicated by Hill’s classification III/IV and symptomatic GERD and erosive esophagitis. Our recommendation is to include Hill’s classification in routine endoscopy reports and workup for GERD.



Similar content being viewed by others
References
El-Serag HB, Sweet S, Winchester CC, Dent J. Update on the epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut. 2014;63:871–880.
Gyawali CP, Kahrilas PJ, Savarino E, et al. Modern diagnosis of GERD: the Lyon Consensus. Gut. 2018;67:1351–1362.
Hill LD, Kozarek RA, Kraemer SJ, et al. The gastroesophageal flap valve: in vitro and in vivo observations. Gastrointest Endosc. 1996;44:541–547.
Hansdotter I, Bjor O, Andreasson A, et al. Hill classification is superior to the axial length of a hiatal hernia for assessment of the mechanical anti-reflux barrier at the gastroesophageal junction. Endosc Int Open. 2016;4:E311–E317.
Weijenborg PW, van Hoeij FB, Smout AJ, Bredenoord AJ. Accuracy of hiatal hernia detection with esophageal high-resolution manometry. Neurogastroenterol Motil. 2015;27:293–299.
Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–2012.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535.
Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P (2009). http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 16 June 2019.
Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R, Global Consensus G. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006;101:1900–1920. quiz 43.
Kaplan M, Tanoglu A, Erkul E, Kara M, Yazgan Y. Association of reflux symptom index scores with gastroesophageal flap valve status. Auris Nasus Larynx.. 2014;41:543–547.
Koch OO, Spaun G, Antoniou SA, et al. Endoscopic grading of the gastroesophageal flap valve is correlated with reflux activity and can predict the size of the esophageal hiatus in patients with gastroesophageal reflux disease. Surg Endosc.. 2013;27:4590–4595.
Lin BR, Wong JM, Chang MC, et al. Abnormal gastroesophageal flap valve is highly associated with gastroesophageal reflux disease among subjects undergoing routine endoscopy in Taiwan. J Gastroenterol Hepatol.. 2006;21:556–562.
Inoue H, Imoto I, Taguchi Y, et al. Reflux esophagitis after eradication of Helicobacter pylori is associated with the degree of hiatal hernia. Scand J Gastroenterol.. 2004;39:1061–1065.
Kayaoglu HA. Correlation of the gastroesophageal flap valve grade with the surgery rate in patients with gastroesophageal reflux disease. Surg Endosc.. 2013;27:801–807.
Keskin O, Kalkan C, Yaman A, Tuzun A, Soykan I. The association between gastroesophageal flap valve function and gastroesophageal reflux symptoms. Acta Gastroenterol Belg.. 2017;80:471–475.
Navarathne NM, Abeysuriya V, Ileperuma A, Thoufeek UL. Endoscopic observations around the gastroesophageal junction in patients with symptomatic gastroesophageal reflux disease in South Asia. Indian J Gastroenterol.. 2010;29:184–186.
Oberg S, Peters JH, DeMeester TR, et al. Endoscopic grading of the gastroesophageal valve in patients with symptoms of gastroesophageal reflux disease (GERD). Surg Endosc.. 1999;13:1184–1188.
Quach DT, Nguyen TT, Hiyama T. Abnormal gastroesophageal flap valve is associated with high gastresophageal reflux disease questionnaire score and the severity of gastroesophageal reflux disease in vietnamese patients with upper gastrointestinal symptoms. J Neurogastroenterol Motil. 2018;24:226–232.
Xie C, Li Y, Zhang N, Xiong L, Chen M, Xiao Y. Gastroesophageal flap valve reflected EGJ morphology and correlated to acid reflux. BMC Gastroenterol. 2017;17:118.
Sonnenberg A, Amorosi SL, Lacey MJ, Lieberman DA. Patterns of endoscopy in the United States: analysis of data from the Centers for Medicare and Medicaid Services and the National Endoscopic Database. Gastrointest Endosc.. 2008;67:489–496.
Beg S, Ragunath K, Wyman A, et al. Quality standards in upper gastrointestinal endoscopy: a position statement of the British Society of Gastroenterology (BSG) and Association of Upper Gastrointestinal Surgeons of Great Britain and Ireland (AUGIS). Gut. 2017;66:1886–1899.
Park EY, Choi MG, Baeg M, et al. The value of early wireless esophageal pH monitoring in diagnosing functional heartburn in refractory gastroesophageal reflux disease. Dig Dis Sci. 2013;58:2933–2939.
Cheong JH, Kim GH, Lee BE, et al. Endoscopic grading of gastroesophageal flap valve helps predict proton pump inhibitor response in patients with gastroesophageal reflux disease. Scand J Gastroenterol. 2011;46:789–796.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Osman, A., Albashir, M.M., Nandipati, K. et al. Esophagogastric Junction Morphology on Hill’s Classification Predicts Gastroesophageal Reflux with Good Accuracy and Consistency. Dig Dis Sci 66, 151–159 (2021). https://doi.org/10.1007/s10620-020-06146-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-020-06146-0