Abstract
Study design
Cross-sectional survey.
Objectives
Most studies on neurological recovery after traumatic spinal cord injury (tSCI) assess treatment effects using the American Spinal Injury Association Impairment Scale (AIS grade) or motor points recovery. To what extent neurological recovery is considered clinically meaningful is unknown. This study investigated the perceived clinical benefit of various degrees of neurological recovery one year after C5 AIS-A tSCI.
Setting
The Netherlands.
Methods
By means of a web-based survey SCI patients and physicians evaluated the benefit of various scenarios of neurological recovery on a scale from 0 to 100% (0% no benefit to 100% major benefit). Recovery to AIS-C and D, was split into C/C+ and D/D+, which was defined by the lower and upper limit of recovery for each grade.
Results
A total of 79 patients and 77 physicians participated in the survey. Each AIS grade improvement from AIS-A was considered significant benefit (all p < 0.05), ranging from 47.8% (SD 26.1) for AIS-B to 86.8% (SD 24.3) for AIS-D+. Motor level lowering was also considered significant benefit (p < 0.05), ranging from 66.1% (SD 22.3) for C6 to 81.7% (SD 26.0) for C8.
Conclusions
Meaningful recovery can be achieved without improving in AIS grade, since the recovery of functional motor levels appears to be as important as improving in AIS grade by both patients and physicians. Moreover, minor neurological improvements within AIS-C and D are also considered clinically meaningful. Future studies should incorporate more detailed neurological outcomes to prevent potential underestimation of neurological recovery by only using the AIS grade.
Similar content being viewed by others
Introduction
The initial severity of spinal cord injury is related to the neurological outcome, where patients with a complete traumatic spinal cord injury (tSCI) may have less neurological recovery than patients with an incomplete tSCI [1, 2]. Although patients can learn to adapt to their condition over time, late complications such as pressure ulcers, respiratory, cardiovascular, and urinary and bowel complications can cause great morbidity and even mortality [3, 4].
Many studies have investigated the effect of early surgical decompression on neurological recovery in patients with tSCI [5,6,7]. This effect is often evaluated with an improvement in American Spinal Injury Association Impairment Scale (AIS grade) or motor score points, which are frequently used as primary outcome measures. Whilst some studies define at least one AIS grade improvement as a success [5, 8], others consider at least two AIS grades improvement as a success [6, 7]. It is however unknown whether this improvement in AIS grade or motor score points translates into clinically meaningful recovery from the patients’ and physicians’ perspective [9].
In order to define clinically meaningful recovery, some studies have evaluated the priorities of neurological recovery in patients with tSCI. The priorities of neurological improvement differ for persons with paraplegia or tetraplegia. Persons with paraplegia have a higher priority of regaining locomotion compared with patients with tetraplegia [10, 11]. Conversely, persons with tetraplegia have a high priority of regaining hand function, which does not necessarily have to coincide with an improvement in AIS grade but could also occur with a decrease in the motor level of injury.
When determining a successful treatment, it is important to define the minimal threshold of recovery that is considered clinically relevant. Since the definition of clinically meaningful recovery after complete cervical tSCI is unclear, we investigated the experienced value of various degrees of neurological recovery by SCI patients and physicians who are involved in treatment of tSCI patients.
Methods
Procedures
We set up a multidisciplinary team of specialists involved in the care of patients with tSCI, consisting of one rehabilitation specialist and one psychologist, who exclusively treat SCI patients, two orthopedic surgeons and two neurosurgeons from level I academic trauma centers. The survey was constructed jointly and tested internally. Approval by the Medical Ethical Research Council was granted.
Participants
The survey was sent to all 138 Dutch neurosurgeons, member of the Dutch Society of Neurological Surgeons, of which 59 were also member of the Dutch Spine Society (DSS). In addition, the survey was sent to all 88 orthopedic surgeons who are members of the DSS and to 34 rehabilitation specialists who are members of the Dutch-Flemish Spinal Cord Society. The survey was also sent to the members of the Dutch Spinal Cord Injury Association, which were contacted through the monthly newsletter. All participants provided informed electronic consent to participate on the survey.
Survey
The survey was conducted between June 2019 and October 2019 and consisted of three sections. The first section included questions on respondent characteristics (Supplementary 1). The second section of the survey contained five questions regarding a hypothetical case with initially a complete C5 AIS-A tSCI. Patients and physicians were asked to give their opinion on the perceived clinical benefit of neurological recovery in a case where the AIS grade remained the same, i.e., AIS-A, but the level of motor injury lowered to C6, 7, and 8 specifically. The cases were accompanied by a brief description of the consequences of the neurological recovery on motor function, mobility, independence in eating, and independence in making transfers [12, 13]. For each scenario, they were asked to indicate how large the benefit of a lower motor level would be compared with the baseline, e.g., C6 compared with C5, C7 compared with C5, or C8 compared with C5. The magnitude of the difference was measured on a continuous scale where 0% defined no clinical benefit and 100% defined major clinical benefit. A difference of 50% was translated to a moderate benefit.
The third section of the survey consisted of seven similar questions regarding the same hypothetical case but now the scenario was improvement in AIS grade instead of motor level. Because there is a wide variation in functionality within the grades AIS-C and D, we described the situation for the lower and upper limit of recovery for each grade, thus creating a C and C+ grade and a D and D+ grade.
Statistical analysis
Difference in importance between and within AIS grades and motor level improvements were calculated with paired t-tests using all responses. Secondly, differences of importance of improvement between physicians and patients were calculated with independent t-tests and Welch’s t-test where appropriate. Levene’s test was used to assess equality of variances. Thirdly, subgroup analyses were performed to investigate possible differences in opinion between (1) surgeons and physiatrists, (2) paraplegic and tetraplegic patients, as well as (3) recent SCI (≤5 years ago) and long-term SCI (>5 years ago). P values < 0.05 were considered statistically significant. Statistical analyses and data visualization were conducted using R version 3.6.0 (R Core Team, 2019).
Results
A total of 156 persons participated in the study: 79 patients and 77 physicians. The mean age of patients was 53.9 ± 16.6 years. Most patients were tetraplegic (64.1%). The majority of patients (68.4%) were long-term SCI patients (>5 years). There were 14 rehabilitation specialists, 35 neurosurgeons, 22 orthopedic surgeons and six other physicians of whom two resident neurosurgery, two resident orthopedic surgery, and two physician assistants. The overall response rate of rehabilitation specialists was 41.2%, 25.4% for neurosurgeons, and 25.0% for orthopedic surgeons. Characteristics of respondents are summarized in Table 1.
AIS improvement
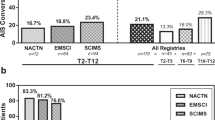
In a range from 0 to 100%, all respondents considered the clinical benefit for recovering from AIS-A to AIS-B 47.8% (SD 26.1), to AIS-C 55.0% (SD 22.2), to AIS-C+ 70.0% (23.5), to AIS-D 81.4% (SD 23.7), and to AIS-D+ 86.8% (SD 24.3, Fig. 1). Every consecutive improvement in AIS grade was perceived as a significant beneficial improvement. Also, neurological recovery within motor incomplete grades AIS-C/C+ and D/D+ was regarded as significant improvement. The importance of the functional improvement per AIS grade improvement was supported when respondents were asked to compare neurological recovery to AIS-B or C. The benefit associated with the difference in neurological recovery between both grades was regarded 53.9% (SD 23.1), which indicates a moderate difference. When respondents were asked to compare recovery to AIS-C+ or D, the difference between recovering to AIS-C+ or D was regarded 72.5% (SD 25.1), which indicates a more than moderate difference in neurological recovery between the two.
Motor level improvement
The perceived success of neurological recovery increased per motor level gained and was significant for all levels (Fig. 1). The clinical benefit from motor level lowering from C5 to C6 was considered 66.1% (SD 22.3), to C7 74.0% (SD 24.2), and to C8 81.7% (SD 26.0). The difference between recovering to C7 instead of C6 was considered clinically different, i.e., 67.3% (SD 25.1), which indicates a more than moderate difference. The difference between neurological recovery to C8 instead of C7 was considered 69.4% (SD 27.1). The clinical benefit of motor level lowering to C6 scored higher than AIS improvement to AIS-B or C (Fig. 1). In addition, recovery to C7 scored higher than recovery to AIS-C+ or lower and C8 higher than recovery to AIS-D or lower.
Subgroup analysis
We observed a significant difference between patients and physicians for the considered value of all levels of motor improvement (Table 2). Physicians were more positive towards the benefit of motor level lowering (Fig. 2). There was no significant difference for AIS grade improvement between patients and physicians, except for recovery to AIS-D and D+ (Table 2 and Fig. 2). However, the variance in responses was significantly larger in patients compared with physicians for all hypothetical cases of neurological improvement. In patients specifically, there were no significant differences in responses based on their level, severity, or duration of SCI. Among physicians, a significant difference was observed between surgeons and physiatrists. Overall rehabilitation specialists were more positive about each type of neurological recovery compared with surgeons (Table 3).
Discussion
This study investigated the perceived success for various degrees of neurological recovery after complete cervical tSCI, both from patients’ and physicians’ perspectives. Not only an improvement in AIS grade, but also lowering of the motor level in complete cervical tSCI has a clinical benefit according to both patients and physicians. Meaningful recovery can therefore be achieved without improving in AIS grade, since regaining complete hand function while remaining AIS-A appeared to be as important as recovering from C5 AIS-A to AIS-D. In particular patients with complete cervical tSCI will recover less likely in AIS grade compared with patients with incomplete injuries [1, 2]. It is unknown whether currently available studies using the AIS grade could potentially underestimate clinically meaningful neurological recovery in these patients.
AIS grade recovery
Most studies in tSCI patients have focused their primary outcomes on AIS grade improvements. While the AIS grade is frequently used to compare treatment effects, the AIS grade by itself does not take into account whether patients who remained the same AIS grade experienced any motor level lowering or whether the improvement in AIS grade led to functional improvement [14]. In addition, cases have been described in which patients did improve neurologically, but paradoxically worsened in AIS grade [15]. Our study shows that AIS grade improvements are indeed considered meaningful by both patients and physicians. In addition, we found that there may even be substantial clinical benefit from smaller neurological improvements within an AIS grade C and D. This finding is particularly important when using the AIS grade as an outcome measure for recovery in patients with an initial AIS-D, since a ceiling effect in neurological recovery has been suggested that subsequently prevents them from further improvement in AIS grade [16, 17]. It is unclear whether currently available studies using the AIS grade as only outcome measure could potentially underestimate clinically meaningful neurological recovery. Other outcome measures have been developed to identify functional recovery in tSCI patients, such as the Spinal Cord Independence Measure (SCIM) and more recently the Spinal Cord Ability Ruler [18]. However, improvement in SCIM can sometimes be achieved by training, independent of any neurological recovery [19]. Therefore, defining relevant outcomes is crucial for designing and interpreting study results, especially in tSCI patients, since meaningful neurological recovery in this specific patient population may not always coincide with AIS grade improvement [16, 20].
Motor level recovery
The recovery of functional motor levels in complete cervical tSCI was found to be both as important as improving in AIS grade, in particular when hand function was regained. The importance of the latter has also been confirmed by two other studies. One of those asked 565 tetraplegic patients to compare certain types of neurological recovery and prioritize them for their expected improvement in quality of life [21]. Patients prioritized regaining hand function above improvement in standing function. The level of motor injury did not appear to affect their prioritization, since patients with C4, C5, C6, and C7 motor levels prioritized regaining hand function above standing. Comparably, another study in 151 tSCI patients asked patients to trade-off certain functions against one another [22]. Patients preferred hand function above walking, with an odds ratio of 1.47 (95% CI 1.38–1.57). The importance in motor level lowering in cervical tSCI was also confirmed by another study in complete (AIS-A) cervical tSCI patients [23]. A lowering of at least two motor levels was significantly associated with improvement in functional independence in these patients [24]. The improvement in motor level recovery can be overlooked when only motor score recovery is considered as outcome measure, since this does not necessarily have to correspond with regaining functional strength in certain muscle groups. Only few studies in cervical tSCI patients evaluated motor level recovery in addition to functional neurological recovery [23, 25]. One study in cervical tSCI patients evaluated motor level recovery in patients surgically treated within and after 24 h. When surgical decompression was performed within 24 h only 1/20 (5%) did not improve in motor level, 7/20 (35%) improved one motor level, 11/20 (55%) improved two motor levels, and one patient (5%) improved completely. In contrast, when surgery was performed after 24 h 4/12 (33%) did not improve in motor level, 6/12 (50%) improved one motor level, and 2/12 (17%) improved two motor levels [25]. As patients with complete cervical tSCI are less likely to recover in AIS grade [2, 16], it is important to evaluate whether early surgical decompression might have an impact on lowering of the motor level in these patients, especially since motor level recovery can also have a major impact on the reconstructive possibilities to regain partial hand function. Reconstructions are possible starting at C5 and more possibilities are present at every lower level of injury [26].
Limitations and strengths
This study has several limitations. Firstly, surveys are subject to the respondents’ interpretation. As we observed a greater variation in the perceived success between patients compared with physicians, it is unknown whether a variation in interpretation of described neurological recovery played a role, or that actual slightly different opinions exist between patients and physicians. In addition, it is important to keep in mind that the perceived success by a group can be experienced differently by an individual. Secondly, the scenarios described in our survey are an unavoidable simplification of the complex and heterogeneous patters of neurological recovery that we see in our daily practice. The neurological recovery patterns in this study are limited to only a few scenarios of recovery after a C5 AIS-A tSCI. Frequently, neurological recovery in tSCI will be more heterogeneous and would consist of a combination of motor level lowering and AIS grade recovery. It is unknown whether certain combinations of these recovery patterns are considered more meaningful compared with others. Moreover, our comparison of motor level recovery over AIS grade improvement is impaired as we did not ask to rank their importance, nor did we ask respondent’s trade-off questions between them. Nonetheless, this study does show that meaningful recovery may be achieved even without improving in AIS grade according to patients and physicians. This could either be through minor neurological recovery within AIS-C or D or improvement in motor level. These findings put the assessment of outcome in complete tSCI patients into perspective. Currently, multiple questions regarding the optimal management of tSCI patients remain unanswered. Most of them are based on the AIS grade as a primary outcome measure. Only very few have incorporated motor score recovery or even motor level recovery. In addition, other functional recoveries which are prioritized by patients [27], such as bladder and bowel management, sexual functions and autonomic functions, should also be examined. Future studies should therefore be encouraged to further explore the field of such recoveries and incorporate more detailed neurological recoveries in order to improve study designs and interpretation of meaningful neurological recovery.
Conclusion
Motor level lowering in complete cervical tSCI patients is considered clinically meaningful neurological recovery in addition to AIS grade recovery. Moreover, minor neurological improvements within AIS-C and D are also considered valuable recovery. These opinions are shared by both physicians and patients. This study shows that meaningful recovery may be achieved even without improving in AIS grade. It is unknown whether the currently available studies using the AIS grade as only outcome measure could potentially underestimate clinically meaningful neurological recovery in these patients. Future studies should therefore not only focus on AIS grade improvement or motor score recovery, but should be encouraged to incorporate more detailed neurological and functional outcome measures.
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Khorasanizadeh M, Yousefifard M, Eskian M, Lu Y, Chalangari M, Harrop JS, et al. Neurological recovery following traumatic spinal cord injury: a systematic review and meta-analysis. J Neurosurg Spine. 2019:1–17. https://doi.org/10.3171/2018.10.SPINE18802.
El Tecle NE, Dahdaleh NS, Bydon M, Ray WZ, Torner JC, Hitchon PW. The natural history of complete spinal cord injury: a pooled analysis of 1162 patients and a meta-analysis of modern data. J Neurosurg Spine. 2018;28:436–43. https://doi.org/10.3171/2017.7.SPINE17107.
Brienza D, Krishnan S, Karg P, Sowa G, Allegretti AL. Predictors of pressure ulcer incidence following traumatic spinal cord injury: a secondary analysis of a prospective longitudinal study. Spinal Cord. 2018;56:28–34. https://doi.org/10.1038/sc.2017.96.
van den Berg ME, Castellote JM, de Pedro-Cuesta J, Mahillo-Fernandez I. Survival after spinal cord injury: a systematic review. J Neurotrauma. 2018;27:1517–28. https://doi.org/10.1089/neu.2009.1138.
Jug M, Kejžar N, Vesel M, Al Mawed S, Dobravec M, Herman S, et al. Neurological recovery after traumatic cervical spinal cord injury is superior if surgical decompression and instrumented fusion are performed within 8 hours versus 8 to 24 hours after injury: a single center experience. J Neurotrauma. 2015;32:1385–92. https://doi.org/10.1089/neu.2014.3767.
ter Wengel PV, de Witt Hamer PC, Pauptit JC, Van der Gaag NA, Oner FC, Vandertop WP. Early surgical decompression improves neurological outcome after complete traumatic cervical spinal cord injury: a meta-analysis. J Neurotrauma. 2018. https://doi.org/10.1089/neu.2018.5974.
Fehlings MG, Vaccaro A, Wilson JR, Singh A, W Cadotte D, Harrop JS, et al. Early versus delayed decompression for traumatic cervical spinal cord injury: results of the surgical timing in acute spinal cord injury study (STASCIS). PLoS ONE. 2012;7. https://doi.org/10.1371/journal.pone.0032037.
Mattiassich G, Gollwitzer M, Gaderer F, Blocher M, Osti M, Lill M, et al. Functional outcomes in individuals undergoing very early (<5 h) and early (5–24 h) surgical decompression in traumatic cervical spinal cord injury: analysis of neurological improvement from the Austrian Spinal Cord Injury Study. J Neurotrauma. 2017;3371. https://doi.org/10.1089/neu.2017.5132.
Van Hedel HJA, Dokladal P, Hotz-Boendermaker S. Mismatch between investigator-determined and patient-reported independence after spinal cord injury: consequences for rehabilitation and trials. Neurorehabil Neural Repair. 2011;25:855–64. https://doi.org/10.1177/1545968311407518.
Anderson KD. Targeting recovery: priorities of the spinal cord-injured population. J Neurotrauma. 2004;21:1371–83. https://doi.org/10.1089/neu.2004.21.1371.
Ditunno PL, Patrick M, Stineman M, Ditunno JF. Who wants to walk? Preferences for recovery after SCI: a longitudinal and cross-sectional study. Spinal Cord. 2008;46:500–6. https://doi.org/10.1038/sj.sc.3102172.
van Hedel HJ, Curt A. Fighting for each segment: estimating the clinical value of cervical and thoracic segments in SCI. J Neurotrauma. 2006;23:1621–31.
Osterthun R, Tjalma TA, Spijkerman DCM, Faber WXM, van Asbeck FWA, Adriaansen JJE, et al. Functional independence of persons with long-standing motor complete spinal cord injury in the Netherlands. J Spinal Cord Med. 2018;1–8. https://doi.org/10.1080/10790268.2018.1504427.
Van Middendorp JJ, Hosman AJF, Pouw MH, Van De Meent H. ASIA impairment scale conversion in traumatic SCI: is it related with the ability to walk? A descriptive comparison with functional ambulation outcome measures in 273 patients. Spinal Cord. 2009;47:555–60. https://doi.org/10.1038/sc.2008.162.
Gündoğdu İ, Akyüz M, Öztürk EA, Cakcı FA. Can spinal cord injury patients show a worsening in ASIA impairment scale classification despite actually having neurological improvement the limitation of ASIA impairment scale classification. Spinal Cord. 2014;52:667–70. https://doi.org/10.1038/sc.2014.89.
Fawcett JW, Curt A, Steeves JD, Coleman WP, Tuszynski MH, Lammertse D, et al. Guidelines for the conduct of clinical trials for spinal cord injury as developed by the ICCP panel: spontaneous recovery after spinal cord injury and statistical power needed for therapeutic clinical trials. Spinal Cord. 2007;45:190–205. https://doi.org/10.1038/sj.sc.3102007.
van Middendorp JJ. Letter to the editor regarding: “Early versus delayed decompression for traumatic cervical spinal cord injury: results of the surgical timing in Acute Spinal Cord Injury Study (STASCIS)”. Spine J. 2012;12:540. https://doi.org/10.1016/j.spinee.2012.06.007.
Catz A, Itzkovich M, Agranov E, Ring H, Tamir A. SCIM—spinal cord independence measure: a new disability scale for patients with spinal cord lesions. Spinal Cord. 1997;35:850–6. https://doi.org/10.1038/sj.sc.3100504.
Scivoletto G, Tamburella F, Laurenza L, Molinari M. The spinal cord independence measure: How much change is clinically significant for spinal cord injury subjects. Disabil Rehabil. 2013;35:1808–13. https://doi.org/10.3109/09638288.2012.756942.
Geisler FH, Coleman WP, Grieco G, Poonian D, Sygen Study Group Measurements and recovery patterns in a multicenter study of acute spinal cord injury. Spine (Philos Pa 1976). 2001;26:S68–86. http://www.ncbi.nlm.nih.gov/pubmed/11805613.
Snoek GJ, Ijzerman MJ, Hermens HJ, Maxwell D, Biering-Sorensen F. Survey of the needs of patients with spinal cord injury: impact and priority for improvement in hand function in tetraplegics. Spinal Cord. 2004;42:526–32. https://doi.org/10.1038/sj.sc.3101638.
Lo C, Tran Y, Anderson K, Craig A, Middleton J. Functional priorities in persons with spinal cord injury: using discrete choice experiments to determine preferences. J Neurotrauma. 2016;33:1958–68. https://doi.org/10.1089/neu.2016.4423.
Cotler JM, Herbison GJ, Nasuti JF, Ditunno JF, An H, Wolff BE. Closed reduction of traumatic cervical spine dislocation using traction weights up to 140 pounds. Spine (Philos Pa 1976). 1993;18:386–90. https://doi.org/10.1097/00007632-199303000-00015.
Kramer JLK, Lammertse DP, Schubert M, Curt A, Steeves JD. Relationship between motor recovery and independence after sensorimotor-complete cervical spinal cord injury. Neurorehabil Neural Repair. 2012;26:1064–71. https://doi.org/10.1177/1545968312447306.
Levi L, Wolf A, Rigamonti D, Ragheb J, Mirvis S, Robinson W. Anterior decompression in cervical spine trauma: does the timing of surgery affect the outcome? Neurosurgery. 1991;29:216–22.
Fox IK, Miller AK, Curtin CM. Nerve and tendon transfer surgery in cervical spinal cord injury: Individualized choices to optimize function. Top Spinal Cord Inj Rehabil. 2018;24:275–87. https://doi.org/10.1310/sci2403-275.
Simpson LA, Eng JJ, Hsieh JTC, Wolfe DL. The health and life priorities of individuals with spinal cord injury: a systematiuc review. 2013;29:1548–55. https://doi.org/10.1089/neu.2011.2226.
Author information
Authors and Affiliations
Contributions
PVTW was responsible for the study conceptualization, survey creation, data acquisition, analysis and interpretation of data, writing of the paper, and final approval of the manuscript. MWMP contributed to study conceptualization, survey creation, interpretation of data, critical revision of the paper, and final approval of the manuscript. EM was responsible for survey creation, data acquisition, analysis and interpretation of the data, critical revision of the paper, and final approval of the manuscript. JSS contributed to study conceptualization, survey creation, interpretation of data, critical revision of the paper, and final approval of the manuscript. AJFH contributed to study conceptualization, interpretation of data, critical revision of the paper, and final approval of the manuscript. SS contributed to study conceptualization, interpretation of data, critical revision of the paper, and final approval of the manuscript. WPV contributed to study conceptualization, interpretation of data, critical revision of the paper, and final approval of the manuscript. FCO contributed to study conceptualization, interpretation of data, critical revision of the paper, final approval of the manuscript, and study supervision.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics statement
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
ter Wengel, P.V., Post, M.W.M., Martin, E. et al. Neurological recovery after traumatic spinal cord injury: what is meaningful? A patients’ and physicians’ perspective. Spinal Cord 58, 865–872 (2020). https://doi.org/10.1038/s41393-020-0436-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-020-0436-4
This article is cited by
-
Wavelet coherence as a measure of trunk stabilizer muscle activation in wheelchair fencers
BMC Sports Science, Medicine and Rehabilitation (2021)