Abstract
Study design
Cross-sectional study.
Objective
To determine the prevalence and potential risk factors of vitamin D deficiency and insufficiency among Malaysian children with spina bifida.
Setting
Four Malaysian tertiary hospitals.
Methods
Children with spina bifida were assessed for potential demographic, disease severity and lifestyle risk factors for vitamin D deficiency and insufficiency. Blood for 25-hydroxy vitamin D (25(OH)D) was taken. Vitamin D deficiency was defined as 25(OH)D levels ≤ 37.5 nmol/L and insufficiency as 37.6–50 nmol/L.
Results
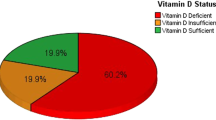
Eighty children aged 2–18 years (42 males) participated in the study. Vitamin D levels ranged from 14 to 105 nmol/L (mean 52.8, SD 19.1). Vitamin D deficiency was identified in 18 (22.5%) and insufficiency in 26 (32.5%) children. Logistic regression analysis showed that skin exposure to sunlight ≤ 21% body surface area (OR: 6.2, CI 1.7–22.9) and duration of sun exposure ≤ 35 min/day (OR: 4.0, CI 1.2–14.1) were significant risk factors for vitamin D deficiency and insufficiency, respectively.
Conclusions
Over half (55%) of Malaysian children with spina bifida seen in urban tertiary hospitals have vitamin D insufficiency and deficiency. Lifestyle sun exposure behaviours were risk factors for vitamin D deficiency and insufficiency.
Similar content being viewed by others
Introduction
Children with spina bifida are at risk for poor bone health, with a 11–30% frequency of fractures and lower bone mineral density (BMD) values compared with age- and gender-matched typically developing children [1]. The risk factors affecting bone health include non-modifiable intrinsic factors, such as genetic predisposition, gender and ethnicity, and modifiable factors, such as BMD, physical activity, sun exposure and dietary intake of calcium and vitamin D.
Vitamin D is a prohormone that is involved in bone health, and helps in the regulation of calcium and phosphorus metabolism. It plays an essential role in preventing nutritional rickets and impaired bone mass, particularly during the childhood period [2]. Failure to achieve an optimal peak bone mass in adolescence can lead to an increased risk of osteoporosis and fracture in adulthood [3]. In addition, vitamin D may also play a role in the prevention of non-skeletal disorders, including cancer, heart disease, type-2 diabetes and autoimmune diseases [4]. Thus, ensuring optimal vitamin D levels in children with spina bifida is important as they have additional pre-existing risk factors for impaired bone health.
Despite Malaysia being a tropical country (latitude 3° north) in Southeast Asia located at the equator with sunshine all year round, there is a high prevalence of vitamin D deficiency and insufficiency even among the normal healthy paediatric population with reported prevalence ranging from 33 to 93% [5,6,7,8]. The wide variation in prevalence rates between studies could have been due to the differences in the age groups of the study population, geographical location (performed in either the urban or rural region) and cut-off values used to define vitamin D deficiency and insufficiency. There are no published data of prevalence rates of vitamin D deficiency and insufficiency among children with spina bifida in the tropical Asian region. To our knowledge, there are only four published studies that have evaluated vitamin D levels in children with spina bifida—two from America (in Houston latitude 29° north and California latitude 36° north), one from Rome (latitude 42° north) and one from Poland (latitude 52° north) [9,10,11,12]. These studies have relatively small sample sizes of between 28 and 49 children, and none of them evaluated thoroughly potential behavioural lifestyle risk factors. Therefore, the aims of this study were to assess the prevalence and potential risk factors of vitamin D deficiency and insufficiency in Malaysian children with spina bifida.
Methods
Participant recruitment
A cross-sectional study was carried out in four urban Malaysian tertiary hospitals at University Malaya Medical Centre Kuala Lumpur, Hospital Tuanku Ja’afar Seremban, Hospital Melaka and Women & Children’s Hospital Kuala Lumpur, respectively. All children with spina bifida between the ages of 2 and 18 years old seen in these hospitals over a 2-year period from September 2016 to September 2018 were recruited.
Exclusion criteria were children with spina bifida with any of the following: (1) co-existing disorders that can impact vitamin D levels, including chronic hepatic, chronic kidney disease, endocrine or gastrointestinal malabsorption disorders; (2) on long-term steroid therapy, vitamin D or calcium supplements. Parents or caregivers of all eligible subjects were provided with a patient information sheet, and written consent was obtained prior to their enrolment.
Data collection
Clinical data of participants were obtained by using standard proforma questionnaires together with a review of medical notes, which included
-
(1)
Demographic data: age, gender, ethnicity, skin pigmentation and pubertal status. Skin pigmentation was assessed based on the skin tone by American Academy of Dermatology criteria, which was categorized into six types of skin pigmentation, ranged from lightest (Type 1) to darkest (Type 6) [13]. Pubertal assessments were based on Tanner staging with the pubertal onset of boys defined as a testicular volume more than 4 ml, and Tanner breast stage more than 2 for girls.
-
(2)
Anthropometric measurements: weight, height and body mass index (BMI). Height was calculated using crown-to-heel measurements for ambulators and arm span measurements for non-ambulators. Arm span measurements were multiplied by 0.90 for those with thoracic functional motor level and by 0.95 for those with mid-lumbar functional motor level [14]. BMI was categorized according to the World Health Organisation BMI-for-age indicators (underweight for BMI-for-age Z score was <−2.0, normal for Z score was between −2.0 and +1.0 and overweight or obese for Z score was >+1.0) [15].
-
(3)
Spina bifida details: the level of spinal defect (cervical, thoracic, lumbar and sacral), motor level (thoracic, high lumbar (L1–L2), mid–low lumbar (L3–L5) and sacral), ambulatory status and presence of other comorbidities, such as past history of fractures, hydrocephalus, epilepsy and bladder or bowel incontinence. Individuals who walked independently in all settings or for short distances were considered ambulant, while those who were full-time wheelchair users or walked with aids in therapeutic settings were considered non-ambulant.
Parents or caregivers were also interviewed using validated questionnaires in assessing possible lifestyle risk factors of low vitamin D level. The questionnaires used were
-
(1)
Physical activity was assessed using the Children Physical Activity Questionnaire [16], which has been validated for Malaysian children [17]. Parents reported on the frequency and duration of their childrens’ physical and sedentary activities across school, organized activity and leisure time over the past 7 days. The responses were scored to yield a measure of metabolic intensity of physical activities, the metabolic physical activity weekly score [16].
-
(2)
Sun exposure practices were evaluated using a questionnaire adapted from Barger-Lux and Heaney [18]. Questions were asked about the duration of daily sun exposure during weekdays and weekends, and the usual attire worn outdoors to estimate the amount of skin exposure to sunlight (calculated as % body surface area).
-
(3)
Dietary intake was assessed using a detailed 7-day dietary recall [19]. Values for daily intake of vitamin D (μg/day) and calcium (mg/day) were calculated using Nutritionist ProTM Software (Axxya System, First Databank, Inc., San Bruno, CA, USA) based on “Nutrient Composition of Malaysian Foods” [20]. Inadequate dietary intake of vitamin D and calcium was based on the values of the Recommended Nutrient Intakes (RNI) for Malaysia [21].
Blood sampling and biochemical analyses
Venous blood samples were taken to determine serum calcium, phosphate, albumin, alkaline phosphatase, alanine transaminase, parathyroid hormone (PTH) and serum 25-hydroxy vitamin D (25(OH)D) levels after the interview. All serum 25(OH)D and PTH levels were measured using electrochemiluminescence immunoassay autoanalyzer Cobas e411 (Roche, Basel, Switzerland) in a quality-controlled accredited laboratory. The interassay coefficient of variance (CV) of 25(OH)D was 3.0% at 170.5 nmol/L (68.2 ng/ml) and 3.6% at 57 nmol/L (22.8 ng/ml). The interassay CV of PTH was 6.2% at 20.2 ng/ml and 4.1% at 58 ng/ml.
25(OH)D concentrations werex classified based on the recommended cut-off points [22], which had been used in other Malaysian studies [5,6,7]: vitamin D insufficiency was defined as 25(OH)D levels of 37.6–50 nmol/L, and vitamin D deficiency was defined as 25(OH)D level of ≤37.5 nmol/L. Reference values for PTH in our laboratory were between 1.0 and 7.0 pmol/L.
Statistical analysis
The sample size calculation for this study was based on a normal Malaysian children prevalence of 20% for vitamin D deficiency [9] and a conservative predicted spina bifida population prevalence of 38% for vitamin D deficiency [10]. The sample size (alpha 5%, beta 20%) required to obtain the predicted spina bifida prevalence of 38% for vitamin D deficiency was 70 subjects with a predicted 20% dropout.
Statistical analysis was performed using IBM® SPSS® Statistics Version 22.0.0.0 for Mac (SPSS Inc., Chicago, IL, USA). Vitamin D levels were categorized as normal (>50 nmol/L), insufficient (37.6–50 nmol/L) and deficient (≤37.5 nmol/L). The results are presented as mean with standard deviation (SD) for normally distributed data, and median with interquartile range (IQR) for non-normally distributed data. Bivariate analysis of the potential risk factors against patients with vitamin D insufficiency (comparing with patients who were vitamin D sufficient) and vitamin D deficiency (comparing with patients who were vitamin D non-deficient) was performed using Pearson chi-square test to identify candidate risk factors (Table 1) for the multivariate analysis. Multiple logistic regression analyses were then separately performed on the risk factors that showed a statistically significant association with 25(OH)D deficiency and insufficiency to further identify which of these factors independently were associated with low vitamin D status. Odds ratio (OR) with 95% confidence interval (CI) was calculated, and a p value < 0.05 was considered as statistically significant.
Results
Participant characteristics
A total of 81 children with spina bifida were recruited; one patient was excluded due to incomplete blood investigations, leaving 80 children (42 males and 38 females) with complete data for analysis. The children consisted of 41 Malay, 23 Chinese and 16 Indian. The age of the study population ranged from 2 to 18 years (median 7.5 years, IQR 5–10). Weight ranged from 7.9 to 57 kg (median 21.3 kg, IQR 14.4–31.7), and 62 children (77.5%) were pre-pubertal. The median BMI was 15.8 kg/m2 (IQR 14.2–19.0). Fifty-two children (65%) of the cohort had a normal BMI and 11 children had a BMI in the overweight or obese category (13.8%). Results of the participants’ demographic, anthropometry, spina bifida disease and lifestyle behaviour are presented in Table 1.
The vitamin D levels in our study population range from 14 to 105 nmol/L with a mean value of 52.8 nmol/L (SD 19.1). Vitamin D insufficiency was found in 26 children (32.5%), while 18 (22.5%) had vitamin D deficiency. Elevated PTH levels (range 7.1–12.6 pmol/L) were reported in five patients, of which one patient had vitamin D insufficiency and two patients had vitamin D deficiency. The rest of the blood biochemical markers were not associated with vitamin D insufficiency or deficiency. None of our patients were on vitamin D supplementation.
Factors predicting vitamin D status
In the bivariate analysis as shown in Table 1, duration of sun exposure ≤ 35 min/day and degree of skin exposure to sunlight ≤ 21% of body surface area were significant risk factors for vitamin D insufficiency (p < 0.05). Age ≥ 8 years old, pubertal status and degree of skin exposure to sunlight ≤ 21% of body surface area were significant risk factors for vitamin D deficiency (p < 0.05).
All these factors (pubertal status, age > 8 years group, duration of sun exposure ≤ 35 min/day and degree of skin exposure to sunlight ≤ 21% of body surface area) were then entered into a multiple logistic regression model to determine independent risk factors associated with vitamin D insufficiency (Table 2) and deficiency (Table 3). A shorter duration of sun exposure (≤35 min/day) (OR: 4.0, CI 1.2–14.1) was significantly associated with vitamin D insufficiency. For vitamin D deficiency, less skin exposure to sunlight ≤ 21% body surface area (OR: 6.2, CI 1.7–22.9) was the only statistically significant risk factor.
Discussion
Our study shows that children with spina bifida seen in urban Malaysian tertiary hospitals, despite living in a tropical country, have a high prevalence of low vitamin D levels with 26 (32.5%) having vitamin D insufficiency and 18 (22.5%) vitamin D deficiency. Children with spina bifida who had a shorter duration of daily sun exposure and less skin exposure to sunlight were at a greater risk of suboptimal vitamin D status. Our study showed a prevalence of 55% vitamin D insufficiency and deficiency (<50 nmol/L), which was higher than the prevalence of 38–43% reported in the studies from America [10, 11], and much lower than 97% reported in the study from Poland [12]. It is probable that the different geographical location between tropical Malaysia with Poland, which is a central European country with a continental climate, would have accounted for the higher prevalence of low vitamin D levels in Poland [12].
Our study is the first from a tropical country and the largest to date to evaluate the vitamin D status among children with spina bifida. The other strength of our study is that we comprehensively evaluated potential lifestyle risk factors, such as physical activity, sun exposure and dietary intake, which may affect vitamin D status. Half of our Malaysian children with spina bifida have suboptimal vitamin D levels during the important bone accrual childhood period, emphasizing the need for clinicians to be vigilant in monitoring vitamin D levels in this population. Our results can be applicable to other South Asian tropical countries with a similar multi-ethnic population. Our findings also support other studies that have shown low vitamin D levels among other children with neurodisability including spinal cord injury and cerebral palsy [23, 24].
Comparison with other published Malaysian vitamin D studies of healthy children yielded mixed results. The prevalence of suboptimal vitamin D status of <50 nmol/L was lower in a study of 869 children 2–12 years old from all over Malaysia (43.7%) [5] and among 1061 secondary school students in the northern and central regions (33%) [8]. This is in keeping with other studies that have reported that children with spina bifida have lower vitamin D levels than the control comparison group [9, 11]. In contrast, there were two local studies of healthy children showing a higher prevalence of vitamin D insufficiency and deficiency; a study of 1361 healthy adolescents age 13 years old from the central and northern regions reported a prevalence of 92.6% [6] and the other of 402 primary school children in urban Kuala Lumpur reported a prevalence of 72.4% [7]. The discrepant results may be due to the varying age ranges, geographical coverage (with the resultant alteration of ethnic and rural composition) and prevalence of obesity, which are potentially important determinants of vitamin D level.
This study showed that sun exposure lifestyle behaviours, in particular duration of sun exposure (≤35 min daily) and proportion of skin exposure (≤21% body surface area exposed to sunlight, equivalent to the face and hands up to short sleeves), were important risk factors for low vitamin D levels among Malaysian children with spina bifida. Local studies on healthy school children [8] and children with epilepsy [25] have found similar associations. Vitamin D is primarily synthesized from skin exposure to sunlight and adopting healthy sun exposure practices is easy to implement as Malaysia has sunshine all year round. Furthermore, there are additional benefits in spending time outdoors for patients with spina bifida, as they are more likely to be physically active and walking, which is beneficial for building bone mass and reducing the risk of obesity. Holick et al. recommended that sunshine exposure of arms and legs (equivalent to 20–25% of body surface area) at 5–15 min three times a week was required for a Caucasian adult, and a duration of three to five times longer was required for adults with darker skin pigmentation [26]. As 60% of our study population had skin types 4–6 indicates that there is a need for longer sun exposure compared with fair-skinned individuals. Our study findings are similar to another study in India which estimated that a daily sun exposure of 30–35 min would be sufficient for acquiring optimal vitamin D, considering the common skin type (Skin Type 5) and culturally appropriate exposure of body surface area of 10% [27].
A significant proportion of our study population did not meet the recommended requirement of dietary calcium and vitamin D intake. Almost half of the subjects (43.8%) had an insufficient dietary calcium intake, while almost all (95%) had vitamin D intake below the Malaysian RNI for gender and age. We did not find a significant association between low dietary intake of calcium or vitamin D and vitamin D status. This is likely due to the small number of subjects with adequate dietary intake of vitamin D (n = 5) which precluded meaningful analysis. As calcium and vitamin D play an important role in bone health, physicians need to provide advice about commonly consumed staple foods that are rich in calcium and vitamin D. However, consumption of vitamin D-rich foods is dictated by local dietary practices, and many local Malaysian foods (with the exception of pasteurized milk) are not fortified with vitamin D. Additional vitamin D supplementation, as recommended by the American Academy of Paediatrics may be a more pragmatic measure [3, 28].
We recognize that there are limitations to our study. Vitamin D level was only assessed at a single point in time in our study, whereas in reality it is the long-term exposure of low vitamin D levels that is important for children; future studies should consider doing serial vitamin D levels. Unlike other studies, we did not find an association between suboptimal vitamin D levels and ethnicity [6, 8, 10] or obesity [6,7,8, 11, 12]. The number of children categorized as obese and into specific ethnic groups in this study may have been insufficient to demonstrate such an association. Type I or II errors during statistical hypothesis testing due to the relatively small numbers of children who had suboptimal vitamin D levels could also be a reason why the duration of sun exposure was a risk factor for vitamin D insufficiency but not vitamin D deficiency in this study. BMD measurements, another indicator of bone fragility, were not performed on our patients. Some of the lifestyle factors, such as sun exposure and physical activities, were acquired through questionnaires that may be subjected to recall biases. Parents or caregivers might also not be fully aware of their children activities or diet and this could cause an inaccurate data being collected. Ideally, studies assessing these lifestyle factors can be performed by using a more objective measurement for these risk factors, such as pedometer for physical activity and “minimal erythemal doses” or “standard erythema doses” from the national meteorological agencies to quantify sun exposure. We have tried to ensure that our patients are representative of the Malaysian spina bifida population by recruiting consecutively over a 2-year period of patients seen from the four main tertiary centres that provide multidisciplinary spina bifida services in West (Peninsular) Malaysia; however, we acknowledge that it is possible that our study group may not be representative of the entire Malaysian spina bifida population as there may be a bias towards the more severe spectrum of the disorder in urban tertiary hospitals. Future causal studies using causal directed acyclic graphs or confirmatory research testing a priori hypotheses should be done to evaluate the relationship between children with spina bifida and low vitamin D levels.
Conclusion
Our study shows that 55% of Malaysian children with spina bifida seen in urban tertiary hospitals have vitamin D insufficiency and deficiency despite living in a tropical country. We identified important risk factors of sun exposure ≤ 35 min daily and skin exposure to sunlight ≤ 21% body surface area for low vitamin D levels. We recommend vitamin D supplementation and subsequent monitoring of vitamin D levels in children with these additional risk factors. Clinicians need to advocate healthy sunlight exposure lifestyle behaviour to children with spina bifida.
Data availability
The datasets generated and analyzed during this study are available from the corresponding author on reasonable request.
References
Marreiros H. Update on bone fragility in spina bifida. J Pediatr Rehabil Med. 2018;11:265–81.
Saggese G, Vierucci F, Boot AM, Czech-Kowalska J, Weber G, Camargo CA Jr, et al. Vitamin D in childhood and adolescence: an expert position statement. Eur J Pediatr. 2015;174:565–76.
NIH Consensus Development Panel on Osteoporosis Prevention. Diagnosis, and therapy, March 7-29, 2000: highlights of the conference. South Med J. 2001;94:569–73.
Rosen CJ, Adams JS, Bikle DD, Black DM, Dernay MB, Manson JE, et al. The nonskeletal effects of vitamin D: an Endocrine Society scientific statement. Endocri Rev. 2012;31:456–92.
Poh BK, Rojroongwasinkul N, Nguyen BK, Sandjaja, Ruzita AT, Yamborisut U, et al. 25-hydroxy-vitamin D demography and the risk of vitamin D insufficiency in the South East Asian Nutrition Surveys (SEANUTS). Asia Pac J Clin Nutr. 2016;25:538–48.
Al-Sadat N, Majid HA, Sim PY, Su TT, Dahlui M, Abu Bakar MF, et al. Vitamin D deficiency in Malaysian adolescents aged 13 years: findings from the Malaysian Health and Adolescents Longitudinal Research Team study (MyHeARTs). BMJ Open. 2016;6:e010689.
Khor GL, Chee WS, Shariff ZM, Poh BK, Arumugam M, Rahman JA, et al. High prevalence of vitamin D insufficiency and its association with BMI-for-age among primary school children in Kuala Lumpur, Malaysia. BMC Public Health. 2011;11:95.
Quah SW, Abdul Majid H, Al-Sadat N, Yahya A, Su TT, Jalaludin MY. Risk factors of vitamin D deficiency among 15-year-old adolescents participating in the Malaysian Health and Adolescents Longitudinal Research Team Study (MyHeARTs). PLoS ONE. 2018;13:e0200736.
Martinelli V, Dell’Atti C, Ausili E, Federici E, Magarelli N, Leone A, et al. Risk of fracture prevention in spina bifida patients: correlation between bone mineral density, vitamin D, and electrolyte values. Child Nerv Syst. 2015;31:1361–5.
Mazur LJ, Wilsford LD, Rosas L, Sullivan E. Low 25-hydroxyvitamin D levels in children with spina bifida. South Med J. 2016;109:31–5.
Van Speybroeck A, Mueske NM, Mittelman SD, Kremer RK, Ryan DD, Wren TA. Fasting serum blood measures of bone and lipid metabolism in children with myelomeningocele for early detection of cardiovascular and bone fragility risk factors. J Spinal Cord Med. 2017;40:193–200.
Okurowska-Zawada B, Kozerska A, Żelazowska B, Kułak W, Wasilewska A, Wysocka J. Serum 25-hydroxyvitamin D, osteocalcin, and parathormone status in children with meningomyelocele. Neuropediatrics. 2012;43:314–9.
Fitzpatrick TB. The validity and practicality of sun-reactive skin types I through IV. Arch Dermatol. 1988;124:869–71.
Jarzem PF, Gledhill RB. Predicting height from arm measurements. J Pediatr Orthop. 1993;13:761–5.
World Health Organization. The WHO child growth standards, 2006. http://www.who.int/childgrowth/en/. Assessed 1 Sept 2019.
Kemper HC, Bakker I, Twisk JW, van Mechelen W. Validation of a physical activity questionnaire to measure the effect of mechanical strain on bone mass. Bone. 2002;30:799–804.
Nor Aini J, Poh BK, Chee WS. Validity of a children’s physical activity questionnaire (cPAQ) for the study of bone health. Pediatr Int. 2013;55:223–8.
Barger-Lux MJ, Heaney RP. Effects of above average summer sun exposure on serum 25-hydroxyvitamin D and calcium absorption. J Clin Endocrinol Metab. 2002;87:4952–6.
Shahar S, Earland J, Abdulrahman S. Validation of a Dietary History Questionnaire against a 7-D Weighed Record for Estimating Nutrient Intake among Rural Elderly Malays. Malays J Nutr. 2000;6:33–44.
Tee ES, Ismail MN, Nasir MA, Khatijah I. Nutrient composition of Malaysian foods. 4th ed. Kuala Lumpur: Institute for Medical Research; 1997.
National Coordinating Committee on Food and Nutrition. Recommended nutrient intakes of Malaysia. A report of the technical working group on Nutritional Guidelines. Putrajaya: Ministry of Health Malaysia; 2017.
Misra M, Pacaud D, Petryk A, Collett-Solberg PF, Kappy M, Drug and Therapeutics Committee of the Lawson Wilkins Pediatric Endocrine Society. Vitamin D deficiency in children and its management: review of current knowledge and recommendations. Pediatrics. 2008;122:398–417.
Coskun Benlidayi I, Basaran S, Seydaoglu G, Guzel R. Vitamin D profile of patients with spinal cord injury and post-stroke hemiplegia: all in the same boat. J Back Musculoskelet Rehabil. 2016;29:2015–210.
Seth A, Aneja S, Singh R, Majumdar R, Sharma N, Gopinath M. Effect of impaired ambulation and anti-epileptic drug intake on vitamin D status of children with cerebral palsy. Paediatr Int Child Health. 2017;37:193–8.
Fong CY, Kong AN, Poh BK, Mohamed AR, Khoo TB, Ng RL, et al. Vitamin D deficiency and its risk factors in Malaysian children with epilepsy. Epilepsia. 2016;57:1271–9.
Holick MF. The D-lightful vitamin D for child health. J Parenter Enter Nutr. 2012;36 Suppl 1:9S–19S.
Augustine LF, Madhavan KN, Kulkarni B. Optimal duration of sun exposure for adequate cutaneous synthesis of vitamin D in Indian cities: an estimate using satellite-based ultraviolet index data. Biomed J Sci Tech Res. 2018;6:5073–7.
Wagner CL, Greer FR, American Academy of Pediatrics Section on Breastfeeding; American Academy of Pediatrics Committee on Nutrition. Prevention of rickets and vitamin D deficiency in infants, children, and adolescents. Pediatrics. 2008;122:1142–52.
Acknowledgements
We would like to thank all the participating children and their parents for the cooperation in conducting the interviews. We would express our gratitude to all the clinicians, clinical staff and nurses of the participating hospital for their help.
Funding
This research study received funding from the University of Malaya research grant (PG 166 2015A).
Author information
Authors and Affiliations
Contributions
CYF was responsible for the overall study, designing the study protocol, patient recruitment, data analysis and writing of the paper. FNO, LCO, TBK and MLL were responsible for patient recruitment, data analysis and writing of the paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics statement
Ethical approval of the study was given by the ethics committee of University Malaya Medical Centre (Ref: 2016717-4029) and Malaysia Medical Research and Ethics Committee (Ref: NMRR-16-1363-31714).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fong, C.Y., Ong, F.N., Ong, L.C. et al. Vitamin D deficiency and insufficiency in Malaysian children with spina bifida. Spinal Cord 58, 1030–1036 (2020). https://doi.org/10.1038/s41393-020-0441-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-020-0441-7