Abstract
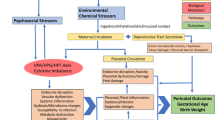
The Environmental Influences on Child Health Outcomes (ECHO) Program will evaluate environmental factors affecting children’s health (perinatal, neurodevelopmental, obesity, respiratory, and positive health outcomes) by pooling cohorts composed of >50,000 children in the largest US study of its kind. Our objective was to identify opportunities for studying chemicals and child health using existing or future ECHO chemical exposure data. We described chemical-related information collected by ECHO cohorts and reviewed ECHO-relevant literature on exposure routes, sources, and environmental and human monitoring. Fifty-six ECHO cohorts have existing or planned chemical biomonitoring data for mothers or children. Environmental phenols/parabens, phthalates, metals/metalloids, and tobacco biomarkers are each being measured by ≥15 cohorts, predominantly during pregnancy and childhood, indicating ample opportunities to study child health outcomes. Cohorts are collecting questionnaire data on multiple exposure sources and conducting environmental monitoring including air, dust, and water sample collection that could be used for exposure assessment studies. To supplement existing chemical data, we recommend biomonitoring of emerging chemicals, nontargeted analysis to identify novel chemicals, and expanded measurement of chemicals in alternative biological matrices and dust samples. ECHO’s rich data and samples represent an unprecedented opportunity to accelerate environmental chemical research to improve the health of US children.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
American College of Obstetricians and Gynecologists Committee on Health Care for Underserved Women, American Society for Reproductive Medicine Practice Committee, The University of California San Francisco Program on Reproductive Health and the Environment. Exposure to toxic environmental agents. Washington, D.C.: The American College of Obstetricians and Gynecologists; 2013. No. 575.
Diamanti-Kandarakis E, Bourguignon J-P, Giudice LC, Hauser R, Prins GS, Soto AM, et al. Endocrine-disrupting chemicals: an endocrine society scientific statement. Endocr Rev. 2009;30:293–342.
President’s Cancer Panel. Reducing environmental cancer risk: what we can do now. Bethesda, MD: U.S. Department of Health and Human Services; 2010.
American Academy of Pediatrics. Pediatric environmental health. Itasca, IL: American Academy of Pediatrics Council on Environmental Health; 2018.
ACOG Committee Opinion No. 575. Exposure to toxic environmental agents. Obstet Gynecol. 2013;122:931–5.
National Research Council. Science and decisions: advancing risk assessment. Washington, D.C.: National Academies Press; 2009.
National Research Council. Phthalates and cumulative risk assessment: the task ahead. Washington, D.C.: National Academies Press; 2008.
OECD (Organisation for Economic Co-operation and Development). 40 years of chemical safety at OECD: quality and efficiency. Paris, France: OECD; 2011.
EPA (US Environmental Protection Agency). 2016 chemical data reporting results. EPA; 2016. https://www.epa.gov/chemical-data-reporting/2016-chemical-data-reporting-results.
Woodruff TJ, Zota AR, Schwartz JM. Environmental chemicals in pregnant women in the United States: NHANES 2003- 2004. Environ Health Perspect. 2011;119:878–85.
CDC (U.S. Centers for Disease Control and Prevention). Fourth national report on human exposure to environmental chemicals-updated tables, January 2019. Atlanta, GA: U.S. Centers for Disease Control and Prevention; 2019.
Swan SH, Main KM, Liu F, Stewart SL, Kruse RL, Calafat AM, et al. Decrease in anogenital distance among male infants with prenatal phthalate exposure. Environ Health Perspect. 2005;113:1056–61.
Lam J, Koustas E, Sutton P, Johnson PI, Atchley DS, Sen S, et al. The navigation guide - evidence-based medicine meets environmental health: integration of animal and human evidence for PFOA effects on fetal growth. Environ Health Perspect. 2014;122:1040–51.
Lederman SA, Jones RL, Caldwell KL, Rauh V, Sheets SE, Tang D, et al. Relation between cord blood mercury levels and early child development in a World Trade Center cohort. Environ Health Perspect. 2008;116:1085–91.
Herbstman JB, Sjödin A, Kurzon M, Lederman SA, Jones RS, Rauh V, et al. Prenatal exposure to PBDEs and neurodevelopment. Environ Health Perspect. 2010;118:712–9.
Chevrier J, Eskenazi B, Holland N, Bradman A, Barr DB. Effects of exposure to polychlorinated biphenyls and organochlorine pesticides on thyroid function during pregnancy. Am J Epidemiol. 2008;168:298–310.
Zota AR, Rudel RA, Morello-Frosch RA, Brody JG. Elevated house dust and serum concentrations of PBDEs in California: unintended consequences of furniture flammability standards? Environ Sci Technol. 2008;42:8158–64.
Nelson JW, Scammell MK, Hatch EE, Webster TF. Social disparities in exposures to bisphenol A and polyfluoroalkyl chemicals: a cross-sectional study within NHANES 2003–2006. Environ Health. 2012;11:10.
Calafat AM, Wong LY, Kuklenyik Z, Reidy JA, Needham LL. Polyfluoroalkyl chemicals in the U.S. population: data from the National Health and Nutrition Examination Survey (NHANES) 2003-2004 and comparisons with NHANES 1999–2000. Environ Health Perspect. 2007;115:1596–602.
Calafat AM, Ye X, Wong L-Y, Reidy JA, Needham LL. Exposure of the U.S. population to bisphenol A and 4-tertiary-octylphenol: 2003–2004. Environ Health Perspect. 2008;116:39–44.
Sjodin A, Wong LY, Jones RS, Park A, Zhang Y, Hodge C, et al. Serum concentrations of polybrominated diphenyl ethers (PBDEs) and polyhrominated biphenyl (PBB) in the United States population: 2003–2004. Environ Sci Technol. 2008;42:1377–84.
EPA (US Environmental Protection Agency). Child-specific exposure factors handbook. Washington, DC: National Center for Environmental Assessment; 2002.
National Institutes of Health (NIH). Environmental influences on child health outcomes (ECHO)-wide cohort data collection protocol, version 1.2. National Institutes of Health; 2018. https://echochildren.org/wp-content/uploads/2019/06/ECHO-Wide-Cohort-Data-Collection-Protocol-Approved-v01.201.pdf.
Wright RO, Teitelbaum S, Thompson C, Balshaw D, Network C. The child health exposure analysis resource as a vehicle to measure environment in the environmental influences on child health outcomes program. Curr Opin Pediatr. 2018;30:285–91.
Pellizzari ED, Woodruff TJ, Boyles RR, Kannan K, Beamer PI, Buckley JP, et al. Identifying and prioritizing chemicals with uncertain burden of exposure: opportunities for biomonitoring and health-related research. Environ Health Perspect. 2019;127:126001.
Adgate JL, Church TR, Ryan AD, Ramachandran G, Fredrickson AL, Stock TH, et al. Outdoor, indoor, and personal exposure to VOCs in children. Environ Health Perspect. 2004;112:1386–92.
Choi H, Perera F, Pac A, Wang L, Flak E, Mroz E, et al. Estimating individual-level exposure to airborne polycyclic aromatic hydrocarbons throughout the gestational period based on personal, indoor, and outdoor monitoring. Environ Health Perspect. 2008;116:1509–18.
Chuang JC, Callahan PJ, Lyu CW, Wilson NK. Polycyclic aromatic hydrocarbon exposures of children in low-income families. J Expo Anal Environ Epidemiol. 1999;9:85–98.
Andrew Clayton C, Pellizzari ED, Whitmore RW, Quackenboss JJ, Adgate J, Sefton K. Distributions, associations, and partial aggregate exposure of pesticides and polynuclear aromatic hydrocarbons in the Minnesota Children’s Pesticide Exposure Study (MNCPES). J Expo Anal Environ Epidemiol. 2003;13:100–11.
Delfino RJ, Staimer N, Tjoa T. Personal endotoxin exposure in a panel study of school children with asthma. Environ Health. 2011;10:69.
Delfino RJ, Staimer N, Tjoa T, Gillen D, Kleinman MT, Sioutas C, et al. Personal and ambient air pollution exposures and lung function decrements in children with asthma. Environ Health Perspect. 2008;116:550–8.
Geyh AS, Xue J, Ozkaynak H, Spengler JD. The Harvard Southern California Chronic Ozone Exposure Study: assessing ozone exposure of grade-school-age children in two Southern California communities. Environ Health Perspect. 2000;108:265–70.
Gordon SM, Callahan PJ, Nishioka MG, Brinkman MC, O’Rourke MK, Lebowitz MD, et al. Residential environmental measurements in the national human exposure assessment survey (NHEXAS) pilot study in Arizona: preliminary results for pesticides and VOCs. J Expo Anal Environ Epidemiol. 1999;9:456–70.
Hoh E, Hites RA. Brominated flame retardants in the atmosphere of the East-Central United States. Environ Sci Technol. 2005;39:7794–802.
Kim JH, Stevens RC, MacCoss MJ, Goodlett DR, Scherl A, Richter RJ, et al. Identification and characterization of biomarkers of organophosphorus exposures in humans. In: Reddy S, editors. Paraoxonases in inflammation, infection, and toxicology. New York: Humana Press; 2010. p. 61–71.
Kinney PL, Chillrud SN, Ramstrom S, Ross J, Spengler JD. Exposures to multiple air toxics in New York City. Environ Health Perspect. 2002;110 Suppl 4:539–46.
La Guardia MJ, Schreder ED, Uding N, Hale RC. Human indoor exposure to airborne halogenated flame retardants: influence of airborne particle size. Int J Environ Res Public Health. 2017;14:507.
Lee T, Grinshpun SA, Martuzevicius D, Adhikari A, Crawford CM, Reponen T. Culturability and concentration of indoor and outdoor airborne fungi in six single-family homes. Atmos Environ. 1994;2006:2902–10.
Lioy PJ, Fan Z, Zhang J, Georgopoulos P, Wang SW, Ohman-Strickland P. et al. Personal and ambient exposures to air toxics in Camden, New Jersey. Boston, MA: Health Effects Research Institute; 2011. Report no.: 1041–5505.
O’Rourke MK, Van de Water PK, Jin S, Rogan SP, Weiss AD, Gordon SM, et al. Evaluations of primary metals from NHEXAS Arizona: distributions and preliminary exposures. National Human Exposure Assessment Survey. J Expo Anal Environ Epidemiol. 1999;9:435–45.
Payne-Sturges DC, Burke TA, Breysse P, Diener-West M, Buckley TJ. Personal exposure meets risk assessment: a comparison of measured and modeled exposures and risks in an urban community. Environ Health Perspect. 2004;112:589–98.
Ryan PH, Brokamp C, Fan ZH, Rao MB. Analysis of personal and home characteristics associated with the elemental composition of PM2.5 in indoor, outdoor, and personal air in the RIOPA Study. Res Rep Health Eff Inst. 2015;185:3–40.
Sheldon L, Clayton A, Keever J, Perritt R, Whitaker D. PTEAM: monitoring of phthalates and PAHs in indoor and outdoor air samples in Riverside, California. Durham, NC: Research Triangle Institute; 1992. Report no.: No. PB-93-205649/XA.
Shendell DG, Winer AM, Stock TH, Zhang L, Zhang JJ, Maberti S, et al. Air concentrations of VOCs in portable and traditional classrooms: results of a pilot study in Los Angeles county. J Expo Anal Environ Epidemiol. 2004;14:44–59.
Suh H, Koutrakis P, Chang L-T. Characterization of the composition of personal, indoor, and outdoor particulate exposures. Sacramento, CA: California Air Resources Board; 2003. https://ww3.arb.ca.gov/research/apr/past/98-330.pdf.
Wilson NK, Chuang JC, Morgan MK, Lordo RA, Sheldon LS. An observational study of the potential exposures of preschool children to pentachlorophenol, bisphenol-A, and nonylphenol at home and daycare. Environ Res. 2007;103:9–20.
Venier M, Audy O, Vojta Š, Bečanová J, Romanak K, Melymuk L, et al. Brominated flame retardants in the indoor environment—Comparative study of indoor contamination from three countries. Environ Int. 2016;94:150–60.
Wilson NK, Chuang JC, Lyu C. Levels of persistent organic pollutants in several child day care centers. J Expo Anal Environ Epidemiol. 2001;11:449–58.
Batterman S, Su F-C, Li S, Mukherjee B, Jia C. Personal exposure to mixtures of volatile organic compounds: modeling and further analysis of the RIOPA data. Res Rep Health Eff Inst. 2014;181:3.
Pellizzari ED, Clayton CA, Rodes CE, Mason RE, Piper LL, Fort B, et al. Particulate matter and manganese exposures in Indianapolis, Indiana. J Expo Anal Environ Epidemiol. 2001;11:423–40.
Tonne CC, Whyatt RM, Camann DE, Perera FP, Kinney PL. Predictors of personal polycyclic aromatic hydrocarbon exposures among pregnant minority women in New York City. Environ Health Perspect. 2004;112:754–9.
Weisel CP. Assessing exposure to air toxics relative to asthma. Environ Health Perspect. 2002;110 Suppl 4:527–37.
Whyatt RM, Barr DB, Camann DE, Kinney PL, Barr JR, Andrews HF, et al. Contemporary-use pesticides in personal air samples during pregnancy and blood samples at delivery among urban minority mothers and newborns. Environ Health Perspect. 2003;111:749–56.
Williams MK, Rundle A, Holmes D, Reyes M, Hoepner LA, Barr DB, et al. Changes in pest infestation levels, self-reported pesticide use, and permethrin exposure during pregnancy after the 2000–2001 US Environmental Protection Agency restriction of organophosphates. Environ Health Perspect. 2008;116:1681–8.
Imm P, Knobeloch L, Buelow C, Anderson HA. Household exposures to polybrominated diphenyl ethers (PBDEs) in a Wisconsin Cohort. Environ Health Perspect. 2009;117:1890–5.
Kanazawa A, Saito I, Araki A, Takeda M, Ma M, Saijo Y, et al. Association between indoor exposure to semi-volatile organic compounds and building-related symptoms among the occupants of residential dwellings. Indoor Air. 2010;20:72–84.
Kim JL, Elfman L, Mi Y, Wieslander G, Smedje G, Norback D. Indoor molds, bacteria, microbial volatile organic compounds and plasticizers in schools–associations with asthma and respiratory symptoms in pupils. Indoor Air. 2007;17:153–63.
Mandin C, Mercier F, Rarnalho O, Lucas JP, Gilles E, Blanchard O, et al. Semi-volatile organic compounds in the particulate phase in dwellings: a nationwide survey in France. Atmos Environ. 2016;136:82–94.
Otake T, Yoshinaga J, Yanagisawa Y. Exposure to phthalate esters from indoor environment. J Expo Anal Environ Epidemiol. 2004;14:524–8.
Pang Y, MacIntosh DL, Camann DE, Ryan PB. Analysis of aggregate exposure to chlorpyrifos in the NHEXAS-Maryland investigation. Environ Health Perspect. 2002;110:235–40.
Rudel RA, Camann DE, Spengler JD, Korn LR, Brody JG. Phthalates, alkylphenols, pesticides, polybrominated diphenyl ethers, and other endocrine-disrupting compounds in indoor air and dust. Environ Sci Technol. 2003;37:4543–53.
Stapleton HM, Allen JG, Kelly SM, Konstantinov A, Klosterhaus S, Watkins D, et al. Alternate and new brominated flame retardants detected in U.S. house dust. Environ Sci Technol. 2008;42:6910–6.
Zota AR, Schaider LA, Ettinger AS, Wright RO, Shine JP, Spengler JD. Metal sources and exposures in the homes of young children living near a mining-impacted Superfund site. J Expo Sci Environ Epidemiol. 2011;21:495–505.
Xue J, Wan Y, Kannan K. Occurrence of bisphenols, bisphenol A diglycidyl ethers (BADGEs), and novolac glycidyl ethers (NOGEs) in indoor air from Albany, New York, USA, and its implications for inhalation exposure. Chemosphere. 2016;151:1–8.
Li H, Lydy MJ, You J. Pyrethroids in indoor air during application of various mosquito repellents: occurrence, dissipation and potential exposure risk. Chemosphere. 2016;144:2427–35.
Abb M, Stahl B, Lorenz W. Analysis of brominated flame retardants in house dust. Chemosphere. 2011;85:1657–63.
Abou-Elwafa Abdallah M, Pawar G, Harrad S. Human dermal absorption of chlorinated organophosphate flame retardants; implications for human exposure. Toxicol Appl Pharm. 2016;291:28–37.
Abdallah MA, Harrad S. Personal exposure to HBCDs and its degradation products via ingestion of indoor dust. Environ Int. 2009;35:870–6.
Abraham JH, Gold DR, Dockery DW, Ryan L, Park JH, Milton DK. Within-home versus between-home variability of house dust endotoxin in a birth cohort. Environ Health Perspect. 2005;113:1516–21.
Bjorklund JA, Sellstrom U, de Wit CA, Aune M, Lignell S, Darnerud PO. Comparisons of polybrominated diphenyl ether and hexabromocyclododecane concentrations in dust collected with two sampling methods and matched breast milk samples. Indoor Air. 2012;22:279–88.
Boros K, Fortin D, Jayawardene I, Chenier M, Levesque C, Rasmussen PE. Comparison of gastric versus gastrointestinal PBET extractions for estimating oral bioaccessibility of metals in house dust. Int J Environ Res Public Health. 2017;14:92.
Castorina R, Butt C, Stapleton HM, Avery D, Harley KG, Holland N, et al. Flame retardants and their metabolites in the homes and urine of pregnant women residing in California (the CHAMACOS cohort). Chemosphere. 2017;179:159–66.
Cowell WJ, Stapleton HM, Holmes D, Calero L, Tobon C, Perzanowski M, et al. Prevalence of historical and replacement brominated flame retardant chemicals in New York City homes. Emerg Contam. 2017;3:32–39.
Deutschle T, Reiter R, Butte W, Heinzow B, Keck T, Riechelmann H. A controlled challenge study on di(2-ethylhexyl) phthalate (DEHP) in house dust and the immune response in human nasal mucosa of allergic subjects. Environ Health Perspect. 2008;116:1487–93.
Deziel NC, Colt JS, Kent EE, Gunier RB, Reynolds P, Booth B, et al. Associations between self-reported pest treatments and pesticide concentrations in carpet dust. Environ Health. 2015;14:27.
Dodge LE, Williams PL, Williams MA, Missmer SA, Toth TL, Calafat AM, et al. Paternal urinary concentrations of parabens and other phenols in relation to reproductive outcomes among couples from a fertility clinic. Environ Health Perspect. 2015;123:665–71.
Fang M, Webster TF, Gooden D, Cooper EM, McClean MD, Carignan C, et al. Investigating a novel flame retardant known as V6: measurements in baby products, house dust, and car dust. Environ Sci Technol. 2013;47:4449–54.
Horick N, Weller E, Milton DK, Gold DR, Li RF, Spiegelman D. Home endotoxin exposure and wheeze in infants: correction for bias due to exposure measurement error. Environ Health Perspect. 2006;114:135–40.
Johnson PI, Stapleton HM, Mukherjee B, Hauser R, Meeker JD. Associations between brominated flame retardants in house dust and hormone levels in men. Sci Total Environ. 2013;445:177–84.
Johnson-Restrepo B, Kannan K. An assessment of sources and pathways of human exposure to polybrominated diphenyl ethers in the United States. Chemosphere. 2009;76:542–8.
Kubwabo C, Stewart B, Zhu J, Marro L. Occurrence of perfluorosulfonates and other perfluorochemicals in dust from selected homes in the city of Ottawa, Canada. J Environ Monit. 2005;7:1074–8.
Lioy PJ, Freeman NCG, Millette JR. Dust: a metric for use in residential and building exposure assessment and source characterization. Environ Health Perspect. 2002;110:969–83.
Meeker JD, Johnson PI, Camann D, Hauser R. Polybrominated diphenyl ether (PBDE) concentrations in house dust are related to hormone levels in men. Sci Total Environ. 2009;407:3425–9.
Park JH, Spiegelman DL, Burge HA, Gold DR, Chew GL, Milton DK. Longitudinal study of dust and airborne endotoxin in the home. Environ Health Perspect. 2000;108:1023–8.
Robertson GL, Lebowitz M, O’Rourke M, Gordon S, Moschandreas D. The National Human Exposure Assessment Survey (NHEXAS) study in Arizona—introduction and preliminary results. J Expo Anal Environ Epidemiol. 1999;9:427–34.
Sahlstrom LM, Sellstrom U, de Wit CA, Lignell S, Darnerud PO. Estimated intakes of brominated flame retardants via diet and dust compared to internal concentrations in a Swedish mother-toddler cohort. Int J Hyg Environ Health. 2015;218:422–32.
Sordillo JE, Alwis UK, Hoffman E, Gold DR, Milton DK. Home characteristics as predictors of bacterial and fungal microbial biomarkers in house dust. Environ Health Perspect. 2011;119:189–95.
Ward MH, Colt JS, Deziel NC, Whitehead TP, Reynolds P, Gunier RB, et al. Residential levels of polybrominated diphenyl ethers and risk of childhood acute lymphoblastic leukemia in California. Environ Health Perspect. 2014;122:1110–6.
Wu N, Herrmann T, Paepke O, Tickner J, Hale R, Harvey LE, et al. Human exposure to PBDEs: associations of PBDE body burdens with food consumption and house dust concentrations. Environ Sci Technol. 2007;41:1584–9.
Dodson RE, Van den Eede N, Covaci A, Perovich LJ, Brody JG, Rudel RA. Urinary biomonitoring of phosphate flame retardants: levels in California adults and recommendations for future studies. Environ Sci Technol. 2014;48:13625–33.
Kubwabo C, Kosarac I, Lalonde K. Determination of selected perfluorinated compounds and polyfluoroalkyl phosphate surfactants in human milk. Chemosphere. 2013;91:771–7.
Camann D, Colt J, Teitelbaum S, Rudel R, Hart R, Gammon M, editors. Pesticide and PAH distributions in house dust from seven areas of USA. Nashville, TN: Society of Environmental Toxicology and Chemistry; 2000. Paper 570.
Larsson K, Berglund M. Children’s exposure to chemicals in indoor environments-a literature survey of chemicals in dust. Swedish Environmental Protection Agency, 2018. http://www.diva-portal.org/smash/get/diva2:1220692/FULLTEXT01.pdf.
Karásková P, Venier M, Melymuk L, Bečanová J, Vojta Š, Prokeš R, et al. Perfluorinated alkyl substances (PFASs) in household dust in Central Europe and North America. Environ Int. 2016;94:315–24.
Subedi B, Sullivan KD, Dhungana B. Phthalate and non-phthalate plasticizers in indoor dust from childcare facilities, salons, and homes across the USA. Environ Pollut. 2017;230:701–8.
Kumarathilaka P, Oze C, Indraratne S, Vithanage M. Perchlorate as an emerging contaminant in soil, water and food. Chemosphere. 2016;150:667–77.
Benotti M, Fisher S, Terracciano S. Occurrence of pharmaceuticals in shallow ground water of Suffolk County, New York, 2002-2005. U.S. geological survey open-file report 2006–1297; 2006. https://pubs.usgs.gov/of/2006/1297/OFR2006-1297.pdf.
Blomquist JD, Denis JM, Cowles J, Hetrick JA, Jones RD, Birchfield NB. Pesticides in selected water-supply reservoirs and finished drinking water, 1999–2000: summary of results from a pilot monitoring program. US geological survey open-file report 2001-456: Washington, DC; 2001. https://pubs.er.usgs.gov/publication/ofr01456.
Hu XC, Andrews DQ, Lindstrom AB, Bruton TA, Schaider LA, Grandjean P, et al. Detection of poly-and perfluoroalkyl substances (PFASs) in US drinking water linked to industrial sites, military fire training areas, and wastewater treatment plants. Environ Sci Technol Lett. 2016;3:344–50.
Moran MJ, Lapham WW, Rowe BL, Zogorski JS. Volatile organic compounds in ground water from rural private wells, 1986 to 1999. J Am Water Resour Assoc. 2004;40:1141–57.
Rowe BL, Toccalino PL, Moran MJ, Zogorski JS, Price CV. Occurrence and potential human-health relevance of volatile organic compounds in drinking water from domestic wells in the United States. Environ Health Perspect. 2007;115:1539–46.
EPA (US Environmental Protection Agency). Compliance monitoring data. Washington, DC: Environmental Protection Agency; 1993–2006. https://www.epa.gov/dwsixyearreview/six-year-review-3-compliance-monitoring-data-2006-2011.
USDA (U.S. Department of Agriculture). Pesticide data program 2010-2015. Washington, DC: U.S. Department of Agriculture National Organic Program; 2012. https://www.ams.usda.gov/datasets/pdp.
USDA (U.S. Department of Agriculture). Pesticide data program: databases and annual summary reports, 2010-2016. Washington, DC: US Department of Agriculture; 2017. https://www.ams.usda.gov/datasets/pdp/pdpdata.
Guo J, Romanak K, Westenbroek S, Hites RA, Venier M. Current-use flame retardants in the water of Lake Michigan tributaries. Environ Sci Technol. 2017;51:9960–9.
EPA (US Environmental Protection Agency). Six-year review 1, 2 and 3 compliance monitoring data. Washington, DC: US Environmental Protection Agency, Office of Water, 2016. https://www.epa.gov/dwsixyearreview/six-year-review-3-compliance-monitoring-data-2006-2011.
FDA (US Food and Drug Administration). Total diet study market baskets 2004-1 through 2005-4. College Park, MD: U.S. Food and Drug Administration, Center for Food Safety and Applied Nutrition. https://www.fda.gov/downloads/Food/FoodScienceResearch/TotalDietStudy/UCM291685.pdf.
Roszko M, Szterk A, Szymczyk K, Waszkiewicz-Robak B. PAHs, PCBs, PBDEs and pesticides in cold-pressed vegetable oils. J Am Oil Chem. 2012;89:389–400.
Schecter A, Colacino J, Haffner D, Patel K, Opel M, Päpke O, et al. Perfluorinated compounds, polychlorinated biphenyls, and organochlorine pesticide contamination in composite food samples from Dallas, Texas, USA. Environ Health Perspect. 2010;118:796–802.
Schecter A, Haffner D, Colacino J, Patel K, Päpke O, Opel M, et al. Polybrominated diphenyl ethers (PBDEs) and hexabromocyclodecane (HBCD) in composite US food samples. Environ Health Perspect. 2010;118:357–62.
Schecter A, Lorber M, Guo Y, Wu Q, Yun SH, Kannan K, et al. Phthalate concentrations and dietary exposure from food purchased in New York State. Environ Health Perspect. 2013;121:473–94.
Schecter A, Päpke O, Harris TR, Tung K, Musumba A, Olson J, et al. Polybrominated diphenyl ether (PBDE) levels in an expanded market basket survey of US food and estimated PBDE dietary intake by age and sex. Environ Health Perspect. 2006;114:1515–20.
Schecter A, Szabo DT, Miller J, Gent TL, Malik-Bass N, Petersen M, et al. Hexabromocyclododecane (HBCD) stereoisomers in U.S. food from Dallas, Texas. Environ Health Perspect. 2012;120:1260–4.
FDA (US Food and Drug Administration). Total diet study. U.S. Food and Drug Administration: Washington, DC. https://www.fda.gov/Food/FoodScienceResearch/TotalDietStudy/ucm184293.htm.
CDC (U.S. Centers for Disease Control and Prevention). Biomonitoring Summaries. Atlanta, GA: CDC; 2017.
Ferguson KK, Colacino JA, Lewis RC, Meeker JD. Personal care product use among adults in NHANES: associations between urinary phthalate metabolites and phenols and use of mouthwash and sunscreen. J Expo Sci Environ Epidemiol. 2017;27:326–32.
Vandenberg LN, Hauser R, Marcus M, Olea N, Welshons WV. Human exposure to bisphenol A (BPA). Reprod Toxicol. 2007;24:139–77.
Calafat AM. Contemporary issues in exposure assessment using biomonitoring. Curr Epidemiol Rep. 2016;3:145–53.
Guidry VT, Longnecker MP, Aase H, Eggesbo M, Zeiner P, Reichborn-Kjennerud T, et al. Measurement of total and free urinary phenol and paraben concentrations over the course of pregnancy: assessing reliability and contamination of specimens in the Norwegian Mother and Child Cohort Study. Environ Health Perspect. 2015;123:705–11.
Rodriguez-Gomez R, Martin J, Zafra-Gomez A, Alonso E, Vilchez JL, Navalon A. Biomonitoring of 21 endocrine disrupting chemicals in human hair samples using ultra-high performance liquid chromatography-tandem mass spectrometry. Chemosphere. 2017;168:676–84.
FDA (US Food and Drug Administration). Safety and effectiveness of consumer antiseptics; topical antimicrobial drug products for over-the-counter human use. Final rule. Fed Regist. 2016;81:61106–30.
Ye X, Wong LY, Kramer J, Zhou X, Jia T, Calafat AM. Urinary concentrations of Bisphenol A and three other bisphenols in convenience samples of U.S. adults during 2000-2014. Environ Sci Technol. 2015;49:11834–9.
Giovanoulis G, Bui T, Xu F, Papadopoulou E, Padilla-Sanchez JA, Covaci A, et al. Multi-pathway human exposure assessment of phthalate esters and DINCH. Environ Int. 2018;112:115–26.
Johns LE, Cooper GS, Galizia A, Meeker JD. Exposure assessment issues in epidemiology studies of phthalates. Environ Int. 2015;85:27–39.
Consumer Product Safety Commission. Rule 82 FR 49938. Prohibition of children’s toys and child care articles containing specified phthalates. Bethesda, MD: Consumer Product Safety Commission; 2017.
Consumer Product Safety Commission. Public law 110 - 314 - Consumer Product Safety Improvement Act of 2008. Bethesda, MD: Consumer Product Safety Commission; 2008.
Renner R. Growing concern over perfluorinated chemicals. Environ Sci Technol. 2001;35:154A–60A.
OECD (Organisation for Economic Co-operation and Development). Potential designated chemicals: perfluoroalkyl and polyfluoroalkyl substances (PFASs). OECD; 2015. https://biomonitoring.ca.gov/sites/default/files/downloads/PotenDesigPFASs_031315.pdf.
Winkens K, Vestergren R, Berger U, Cousins IT. Early life exposure to per- and polyfluoroalkyl substances (PFASs): a critical review. Emerg Contam. 2017;3:55–68.
3M Company. Phase-out plan for POSF-based products. Letter from William Weppner (3M Company) to Charles Auer (U.S. EPA). 7 July 2000. U.S. EPA docket AR-226-0600: Washington, DC; 2000. http://www.fluoridealert.org/wp-content/pesticides/pfos.fr.final.docket.0009.pdf.
EPA (US Environmental Protection Agency). Fact sheet: 2010/2015 PFOA Stewardship Program. Washington, DC: EPA; 2018.
Ritter S. Fluorochemicals go short. Chem Eng N. 2010;88:12–17.
CDC (U.S. Centers for Disease Control and Prevention). An overview of perfluoroalkyl and polyfluoroalkyl substances and interim guidance for clinicians responding to patient exposure concerns. Atlanta, GA: CDC; 2017.
Alves A, Jacobs G, Vanermen G, Covaci A, Voorspoels S. New approach for assessing human perfluoroalkyl exposure via hair. Talanta. 2015;144:574–83.
Wang Y, Zhong Y, Li J, Zhang J, Lyu B, Zhao Y, et al. Occurrence of perfluoroalkyl substances in matched human serum, urine, hair and nail. J Environ Sci. 2018;67:191–7.
Ritscher A, Wang Z, Scheringer M, Boucher JM, Ahrens L, Berger U, et al. Zurich statement on future actions on per- and polyfluoroalkyl substances (PFASs). Environ Health Perspect. 2018;126:84502.
EPA (US Environmental Protection Agency). Development of a relative potency factor (Rpf) approach for polycyclic aromatic hydrocrabon (PAH) mixtures (external review draft). Washington, DC: EPA; 2010.
Costa LG. Organophosphorus compounds at 80: some old and new issues. Toxicol Sci. 2018;162:24–35.
Hertz-Picciotto I, Sass JB, Engel S, Bennett DH, Bradman A, Eskenazi B, et al. Organophosphate exposures during pregnancy and child neurodevelopment: recommendations for essential policy reforms. PLoS Med. 2018;15:e1002671.
Needham LL. Assessing exposure to organophosphorus pesticides by biomonitoring in epidemiologic studies of birth outcomes. Environ Health Perspect. 2005;113:494–8.
Beamer PI, Canales RA, Ferguson AC, Leckie JO, Bradman A. Relative pesticide and exposure route contribution to aggregate and cumulative dose in young farmworker children. Int J Environ Res Public Health. 2012;9:73–96.
Silva MJ, Wong LY, Samandar E, Preau JL Jr., Jia LT, Calafat AM. Exposure to di-2-ethylhexyl terephthalate in the U.S. general population from the 2015-2016 National Health and Nutrition Examination Survey. Environ Int. 2019;123:141–7.
Silva MJ, Jia T, Samandar E, Preau JL Jr., Calafat AM. Environmental exposure to the plasticizer 1,2-cyclohexane dicarboxylic acid, diisononyl ester (DINCH) in U.S. adults (2000-2012). Environ Res. 2013;126:159–63.
BASF. BASF doubles production capacity of Hexamoll DINCH to 200,000 metric tons. BASF; 2014. https://www.basf.com/en/company/news-and-media/news-releases/2014/05/p-14-231.html.
Silva MJ, Wong LY, Samandar E, Preau JL, Calafat AM, Ye X. Exposure to di-2-ethylhexyl terephthalate in a convenience sample of U.S. adults from 2000 to 2016. Arch Toxicol. 2017;91:3287–91.
Covaci A, Harrad S, Abdallah MA, Ali N, Law RJ, Herzke D, et al. Novel brominated flame retardants: a review of their analysis, environmental fate and behaviour. Environ Int. 2011;37:532–56.
van der Veen I, de Boer J. Phosphorus flame retardants: properties, production, environmental occurrence, toxicity and analysis. Chemosphere. 2012;88:1119–53.
Stapleton HM, Klosterhaus S, Eagle S, Fuh J, Meeker JD, Blum A, et al. Detection of organophosphate flame retardants in furniture foam and U.S. house dust. Environ Sci Technol. 2009;43:7490–5.
de Boer J, Ballesteros-Gómez A, Leslie HA, Brandsma SH, Leonards PEG. Flame retardants: dust - and not food - might be the risk. Chemosphere. 2016;150:461–4.
Hoffman K, Garantziotis S, Birnbaum LS, Stapleton HM. Monitoring indoor exposure to organophosphate flame retardants: hand wipes and house dust. Environ Health Perspect. 2015;123:160–5.
Hoffman K, Butt CM, Chen A, Limkakeng AT, Stapleton HM. High exposure to organophosphate flame retardants in infants: associations with baby products. Environ Sci Technol. 2015;49:14554–9.
Wei GL, Li DQ, Zhuo MN, Liao YS, Xie ZY, Guo TL, et al. Organophosphorus flame retardants and plasticizers: sources, occurrence, toxicity and human exposure. Environ Pollut. 2015;196:29–46.
Schreder ED, Uding N, La Guardia MJ. Inhalation a significant exposure route for chlorinated organophosphate flame retardants. Chemosphere. 2016;150:499–504.
Liu X, Yu G, Cao Z, Wang B, Huang J, Deng S, et al. Occurrence of organophosphorus flame retardants on skin wipes: Insight into human exposure from dermal absorption. Environ Int. 2017;98:113–9.
Xu F, Tay JH, Covaci A, Padilla-Sánchez JA, Papadopoulou E, Haug LS, et al. Assessment of dietary exposure to organohalogen contaminants, legacy and emerging flame retardants in a Norwegian cohort. Environ Int. 2017;102:236–43.
Shi Z, Zhang L, Li J, Zhao Y, Sun Z, Zhou X, et al. Novel brominated flame retardants in food composites and human milk from the Chinese Total Diet Study in 2011: Concentrations and a dietary exposure assessment. Environ Int. 2016;96:82–90.
Zhang X, Zou W, Mu L, Chen Y, Ren C, Hu X, et al. Rice ingestion is a major pathway for human exposure to organophosphate flame retardants (OPFRs) in China. J Hazard Mater. 2016;318:686–93.
Butt C, Congleton J, Hoffman K, Fang M, Stapleton HM. Metabolites of organophosphate flame retardants and 2-ethylhexyl tetrabromobenzoate (EH-TBB) in urine from paired mothers and toddlers. Environ Sci Technol. 2014. https://doi.org/10.1021/es5025299.
Hoffman K, Daniels JL, Stapleton HM. Urinary metabolites of organophosphate flame retardants and their variability in pregnant women. Environ Int. 2014;63:169–72.
Hoffman K, Fang M, Horman B, Patisaul HB, Garantziotis S, Birnbaum LS, et al. Urinary tetrabromobenzoic acid (TBBA) as a biomarker of exposure to the flame retardant mixture Firemaster® 550. Environ Health Perspect. 2014;122:963–9.
Meeker JD, Cooper EM, Stapleton HM, Hauser R. Exploratory analysis of urinary metabolites of phosphorus-containing flame retardants in relation to markers of male reproductive health. Endocr Disruptors (Austin). 2013;1:e26306.
Crump D, Chiu S, Kennedy SW. Effects of tris(1,3-dichloro-2-propyl) phosphate and tris(1-chloropropyl) phosphate on cytotoxicity and mRNA expression in primary cultures of avian hepatocytes and neuronal cells. Toxicol Sci. 2012;126:140–8.
Hoffman K, Butt CM, Webster TF, Preston EV, Hammel SC, Makey C, et al. Temporal trends in exposure to organophosphate flame retardants in the United States. Environ Sci Technol Lett. 2017;4:112–8.
Urbansky E. Perchlorate chemistry: implications for analysis and remediation. Bioremediation J. 1998;2:81–95.
El Aribi H, Le Blanc YJ, Antonsen S, Sakuma T. Analysis of perchlorate in foods and beverages by ion chromatography coupled with tandem mass spectrometry (IC-ESI-MS/MS). Anal Chim Acta. 2006;567:39–47.
Dyke JV, Ito K, Obitsu T, Hisamatsu Y, Dasgupta PK, Blount BC. Perchlorate in dairy milk. Comparison of Japan versus the United States. Environ Sci Technol. 2007;41:88–92.
Kirk AB, Dyke JV, Martin CF, Dasgupta PK. Temporal patterns in perchlorate, thiocyanate, and iodide excretion in human milk. Environ Health Perspect. 2007;115:182–6.
Guruge KS, Wu Q, Kannan K. Occurrence and exposure assessment of perchlorate, iodide and nitrate ions from dairy milk and water in Japan and Sri Lanka. J Environ Monit. 2011;13:2312–20.
ATSDR (Agency for Toxic Substances and Disease Registry). Nitrates/nitrites poisoning: patient education care instruction sheet. ATSDR; 2013. http://www.atsdr.cdc.gov/csem/nitrate_2013/docs/nitrate_patient-education.pdf.
Zil -a- Rubab, Rahman MA. Serum thiocyanate levels in smokers, passive smokers and never smokers. J Pak Med Assoc. 2006;56:323–6.
Crump KS, Gibbs JP. Benchmark calculations for perchlorate from three human cohorts. Environ Health Perspect. 2005;113:1001–8.
Oldi JF, Kannan K. Analysis of perchlorate in human saliva by liquid chromatography-tandem mass spectrometry. Environ Sci Technol. 2009;43:142–7.
Oldi JF, Kannan K. Perchlorate in human blood serum and plasma: relationship to concentrations in saliva. Chemosphere. 2009;77:43–47.
Kirk AB, Martinelango PK, Tian K, Dutta A, Smith EE, Dasgupta PK. Perchlorate and iodide in dairy and breast milk. Environ Sci Technol. 2005;39:2011–7.
EPA (US Environmental Protection Agency). Pyrethrins and pyrethroids. EPA; 2017. https://www.epa.gov/ingredients-used-pesticide-products/pyrethrins-and-pyrethroids.
EPA (US Environmental Protection Agency). Revaluation: pyrethrins and pyrethroids. Pesticides: regulating pesticides. EPA; 2010. http://www.epa.gov/oppsrrd1/reevaluation/pyrethroids-pyrethrins.html.
Trunnelle KJ, Bennett DH, Tulve N, Clifton MS, Davis M, Calafat A, et al. Urinary pyrethroid and chlorpyrifos metabolite concentrations in northern California families and their relationship to indoor residential insecticide levels, part of SUPERB. Environ Sci Technol. 2014;48:1931–9.
Parsons PJ. Atomic spectrometry in clinical chemistry. In: Evenson MA, editors. Encyclopedia of analytical chemistry, applications, theory and instrumentation. Vol. 2. Chichester, UK: John Wiley & Sons, Inc.; 2000. p. 1091–123.
Parsons PJ, Barbosa F Jr. Atomic spectrometry and trends in clinical laboratory medicine. Spectrochim Acta Part B Spectrosc. 2007;62:992–1003.
Verdon CP, Caldwell KL, Fresquez MR, Jones RL. Determination of seven arsenic compounds in urine by HPLC-ICP-DRC-MS: a CDC population biomonitoring method. Anal Bioanal Chem. 2009;393:939–47.
Davis WC, Vander Pol SS, Schantz MM, Long SE, Day RD, Christopher SJ. An accurate and sensitive method for the determination of methylmercury in biological specimens using GC-ICP-MS with solid phase microextraction. J Anal Spectrom. 2004;19:1546–51.
McShane WJ, Steven Pappas R, Paschal D. Analysis of total arsenic, total selenium and total chromium in urine by inductively coupled plasma-dynamic reaction cell-mass spectrometry. J Anal Spectrom. 2007;22:630–5.
Jarrett JM, Xiao G, Caldwell KL, Henahan D, Shakirova G, Jones RL. Eliminating molybdenum oxide interference in urine cadmium biomonitoring using ICP-DRC-MS. J Anal Spectrom. 2008;23:962–7.
Praamsma ML, Arnason JG, Parsons PJ. Monitoring Mn in whole blood and urine: a comparison between electrothermal atomic absorption and inorganic mass spectrometry. J Anal Spectrom. 2011;26:1224–32.
Parsons PJ, Palmer CD, Caldwell KL, Jones RL. Determination of total mercury in urine by inductively coupled plasma mass spectrometry (ICP-MS). In: Holland G, Bandura D, editors. Plasma source mass spectrometry: proceedings of the 9th international conference on plasma source mass spectrometry. London: Royal Society of Chemistry; 2005. p. 59–71.
Taylor A, Jones R, Leblanc A, Mazarrasa O, Lee M-Y, Parsons P, et al. Instability of mercury in specimens of human urine for external quality assessment. Accredit Qual Assur. 2009;14:461–6.
Arora M, Austin C, Sarrafpour B, Hernandez-Avila M, Hu H, Wright RO, et al. Determining prenatal, early childhood and cumulative long-term lead exposure using micro-spatial deciduous dentine levels. PLoS One. 2014;9:e97805.
Matt GE, Quintana PJ, Destaillats H, Gundel LA, Sleiman M, Singer BC, et al. Thirdhand tobacco smoke: emerging evidence and arguments for a multidisciplinary research agenda. Environ Health Perspect. 2011;119:1218–26.
Llaquet H, Pichini S, Joya X, Papaseit E, Vall O, Klein J, et al. Biological matrices for the evaluation of exposure to environmental tobacco smoke during prenatal life and childhood. Anal Bioanal Chem. 2010;396:379–99.
Hecht SS, Stepanov I, Carmella SG. Exposure and metabolic activation biomarkers of carcinogenic tobacco-specific nitrosamines. Acc Chem Res. 2016;49:106–14.
Hukkanen J, Jacob P 3rd, Benowitz NL. Metabolism and disposition kinetics of nicotine. Pharm Rev. 2005;57:79–115.
Jones IA, St Helen G, Meyers MJ, Dempsey DA, Havel C, Jacob P 3rd, et al. Biomarkers of secondhand smoke exposure in automobiles. Tob Control. 2014;23:51–57.
Avila-Tang E, Al-Delaimy WK, Ashley DL, Benowitz N, Bernert JT, Kim S, et al. Assessing secondhand smoke using biological markers. Tob Control. 2013;22:164–71.
Wei B, Blount BC, Xia B, Wang L. Assessing exposure to tobacco-specific carcinogen NNK using its urinary metabolite NNAL measured in US population: 2011-2012. J Expo Sci Environ Epidemiol. 2016;26:249–56.
Li XF, Mitch WA. Drinking water disinfection byproducts (DBPs) and human health effects: multidisciplinary challenges and opportunities. Environ Sci Technol. 2018;52:1681–9.
ATSDR (Agency for Toxic Substances and Disease Registry). Toxicological profile for bromoform and chlorodibromomethane. Atlanta, GA: U.S. Department of Health and Human Services, Public Health Service; 2005. https://www.atsdr.cdc.gov/toxprofiles/tp.asp?id=713&tid=128.
Dick D, Ng KM, Sauder DN, Chu I. In vitro and in vivo percutaneous absorption of 14C-chloroform in humans. Hum Exp Toxicol. 1995;14:260–5.
Leavens TL, Blount BC, DeMarini DM, Madden MC, Valentine JL, Case MW, et al. Disposition of bromodichloromethane in humans following oral and dermal exposure. Toxicol Sci. 2007;99:432–45.
Bradman A, Whyatt RM. Characterizing exposures to nonpersistent pesticides during pregnancy and early childhood in the National Children’s Study: a review of monitoring and measurement methodologies. Environ Health Perspect. 2005;113:1092–9.
Bradman A, Barr DB, Claus Henn BG, Drumheller T, Curry C, Eskenazi B. Measurement of pesticides and other toxicants in amniotic fluid as a potential biomarker of prenatal exposure: a validation study. Environ Health Perspect. 2003;111:1779–82.
CDC (U.S. Centers for Disease Control and Prevention). Fourth national report on human exposure to environmental chemicals. Atlanta, GA; CDC; 2009.
Li YF, Venkatesh S, Li D. Modeling global emissions and residues of pesticides. Environ Model Assess. 2004;9:237–43.
Fromme H, Becher G, Hilger B, Volkel W. Brominated flame retardants - exposure and risk assessment for the general population. Int J Hyg Environ Health. 2016;219:1–23.
UNEP (United Nations Environment Programme). All POPs listed in the Stockholm Convention. UNEP; 2008. http://chm.pops.int/TheConvention/ThePOPs/AllPOPs/tabid/2509/Default.aspx.
Parry E, Zota AR, Park JS, Woodruff TJ. Polybrominated diphenyl ethers (PBDEs) and hydroxylated PBDE metabolites (OH-PBDEs): a six-year temporal trend in Northern California pregnant women. Chemosphere. 2017;195:777–83.
Čechová E, Vojta Š, Kukučka P, Kočan A, Trnovec T, Murínová Ľ, et al. Legacy and alternative halogenated flame retardants in human milk in Europe: Implications for children’s health. Environ Int. 2017;108:137–45.
Abdallah MA, Harrad S. Dermal contact with furniture fabrics is a significant pathway of human exposure to brominated flame retardants. Environ Int. 2018;118:26–33.
Sjodin A, Patterson DG Jr., Bergman A. A review on human exposure to brominated flame retardants–particularly polybrominated diphenyl ethers. Environ Int. 2003;29:829–39.
ATSDR (Agency for Toxic Substances and Disease Registry). Toxicological profile for polychlorinated biphenyls (PCBs). Atlanta, GA: U.S. Department of Health and Human Services, Public Health Service; 2000. https://www.atsdr.cdc.gov/toxprofiles/tp.asp?id=142&tid=26.
Batterman SA, Chernyak S, Su FC. Measurement and comparison of organic compound concentrations in plasma, whole blood, and dried blood spot samples. Front Genet. 2016;7:64.
Grandjean P, Budtz-Jorgensen E, Barr DB, Needham LL, Weihe P, Heinzow B. Elimination half-lives of polychlorinated biphenyl congeners in children. Environ Sci Technol. 2008;42:6991–6.
Shirai JH, Kissel JC. Uncertainty in estimated half-lives of PCBS in humans: impact on exposure assessment. Sci Total Environ. 1996;187:199–210.
Tylavsky FA, Ferrara A, Catellier DJ, Oken E, Li X, Law A, et al. Understanding childhood obesity in the US: the NIH environmental influences on child health outcomes (ECHO) program. Int J Obes. 2019. https://doi.org/10.1038/s41366-019-0470-5.
Braun JM, Gennings C, Hauser R, Webster TF. What can epidemiological studies tell us about the impact of chemical mixtures on human health? Environ Health Perspect. 2016;124:A6–9.
Carlin DJ, Rider CV, Woychik R, Birnbaum LS. Unraveling the health effects of environmental mixtures: an NIEHS priority. Environ Health Perspect. 2013;121:A6–8.
Hamra GB, Buckley JP. Environmental exposure mixtures: questions and methods to address them. Curr Epidemiol Rep. 2018;5:160–5.
Stafoggia M, Breitner S, Hampel R, Basagana X. Statistical approaches to address multi-pollutant mixtures and multiple exposures: the state of the science. Curr Environ Health Rep. 2017;4:481–90.
Braun JM, Gray K. Challenges to studying the health effects of early life environmental chemical exposures on children’s health. PLoS Biol. 2017;15:e2002800.
Buckley JP, Hamra GB, Braun JM. Statistical approaches for investigating periods of susceptibility in children’s environmental health research. Curr Environ Health Rep. 2019;6:1–7.
Moschet C, Anumol T, Lew BM, Bennett DH, Young TM. Household dust as a repository of chemical accumulation: new insights from a comprehensive high-resolution mass spectrometric study. Environ Sci Technol. 2018;52:2878–87.
Buckley JP, Engel SM, Braun JM, Whyatt RM, Daniels JL, Mendez MA, et al. Prenatal phthalate exposures and body mass index among 4- to 7-year-old children: a pooled analysis. Epidemiology. 2016;27:449–58.
Engel SM, Bradman A, Wolff MS, Rauh VA, Harley KG, Yang JH, et al. Prenatal organophosphorus pesticide exposure and child neurodevelopment at 24 months: an analysis of four birth cohorts. Environ Health Perspect. 2016;124:822–30.
Harley KG, Engel SM, Vedar MG, Eskenazi B, Whyatt RM, Lanphear BP, et al. Prenatal exposure to organophosphorous pesticides and fetal growth: pooled results from four longitudinal birth cohort studies. Environ Health Perspect. 2016;124:1084–92.
Casas M, Nieuwenhuijsen M, Martinez D, Ballester F, Basagana X, Basterrechea M, et al. Prenatal exposure to PCB-153, p,p’-DDE and birth outcomes in 9000 mother-child pairs: exposure-response relationship and effect modifiers. Environ Int. 2015;74:23–31.
Iszatt N, Stigum H, Verner MA, White RA, Govarts E, Murinova LP, et al. Prenatal and postnatal exposure to persistent organic pollutants and infant growth: a pooled analysis of seven European birth cohorts. Environ Health Perspect. 2015;123:730–6.
Forns J, Stigum H, Hoyer BB, Sioen I, Sovcikova E, Nowack N, et al. Prenatal and postnatal exposure to persistent organic pollutants and attention-deficit and hyperactivity disorder: a pooled analysis of seven European birth cohort studies. Int J Epidemiol. 2018;47:1082–97.
Acknowledgements
The authors thank David Balshaw (National Institute of Environmental Health Sciences) for insightful contributions and Emma Alquist and Timothy Shields (ECHO Data Analysis Center, Johns Hopkins Bloomberg School of Public Health) for technical assistance.
Funding
Research reported in this publication was supported by the ECHO program, Office of The Director, NIH, under award numbers U2COD023375 (Coordinating Center), U24OD023382 (Data Analysis Center, JPB, GBH, EDP, MZ), UG3OD023305, UH3OD023305, UG3OD023271, UH3OD023271, and UG3OD023349, UH3OD023349 (ESB), UG3OD023282 (PIB), UG3OD023365, UH3OD023365 (DHB), UG3OD023316 (MSB), U2CES026544 (TRF), UG3OD023348, UH3OD023348 (RCF), U24OD023319-01 (Person-Reported Outcomes Core, WEF, RI), 3U2CES026533-01S1-3 (SSH), U2CES026542-01 (KK, PJP), UG3OD023275, UH3OD023275 (MPK, AJS-P), UG3OD023342, UH3OD023342 and 1U2COD023375-02 (KL), UG3OD023248, UH3OD023248 (APS), UG3OD023251, UH3OD023251 (DJW), UG3OD023272, UH3OD023272 (AW, TJW). This research was also supported by NIEHS P01ES022841 (TJW), NIEHS R01ES027051 (TJW), US EPA RD 83543301 (TJW), U2CES026542-01 (KK, PJP), P30 ES006694 (PIB), NIEHS P30 ES005022 (ESB), NIDDK R01DK076648 (APS), NIEHS R00ES025817 (APS), NIEHS P01ES022832 (MRK), and US EPA RD-83544201 (MRK). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
WEF is a founding partner in EnMed MicroAnalytics, a company that provides heavy metal screening for newborns and children. MSB has worked for ICF International as a paid consultant on the US EPA “IRIS Draft Toxicological Review of PCBs: Effects Other Than Cancer.” All other authors declare they have no actual or potential competing financial interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Members of the ECHO are listed in Appendix.
Supplementary information
Appendix
Appendix
The authors wish to thank our ECHO colleagues, the medical, nursing and program staff, as well as the children and families participating in the ECHO cohorts. We also acknowledge the contributions of the ECHO program collaborators.
ECHO components: Coordinating Center: Duke Clinical Research Institute, Durham, North Carolina: P. B. Smith, K. L. Newby, D. K. Benjamin. Data Analysis Center: Johns Hopkins University Bloomberg School of Public Health, Baltimore, Maryland: L. P. Jacobson; Research Triangle Institute, Durham, North Carolina: C. B. Parker. Person-Reported Outcomes Core: Northwestern University, Evanston, IL, USA: R. Gershon, D. Cella. Children’s Health and Exposure Analysis Resource: Icahn School of Medicine at Mount Sinai, New York City, NY, USA: S. L. Teitelbaum, R. O. Wright; Wadsworth Center, Albany, NY, USA: K. M. Aldous. RTI International, Research Triangle Park, NC, USA: T. Fennell; University of Minnesota, Minneapolis, MN, USA: S. S. Hecht, L. Peterson; Westat, Inc., Rockville, MD, USA: B. O’Brien. Idea States Pediatric Clinical Trials Network (ISPCTN): University of Arkansas for Medical Sciences, Little Rock, AR, USA: J. Y. Lee, J. Snowden. ISPCTN Data Coordinating and Operations Center: University of Arkansas for Medical Sciences, Little Rock, AR, USA. Pediatric Cohorts: See below under ECHO cohort awardees and cohort sites. ECHO Cohort Awardees
Albert Einstein College of Medicine, Bronx, NY, USA: J. L. Aschner
Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, USA: B. Poindexter
Icahn School of Medicine at Mount Sinai, New York, NY, USA: S. L. Teitelbaum, A. Stroustrup, C. Grennings, S. Andra, M. Arora
University of Buffalo, Buffalo, NY, USA: A. M. Reynolds
University of Florida, Gainesville, FL, USA: M. Hudak
University of Rochester, Rochester, NY, USA: G. Pryhuber
Vanderbilt University Medical Center, Nashville, TN, USA: P. Moore
Wake Forest University Health Sciences, Winston Salem, NC, USA: L. Washburn, J. Helderman
Avera McKennan Hospital and University Health Center, Sioux Falls, SD, USA: A. J. Elliott
The Trustees of Columbia University, New York, NY, USA: W. Fifer, J. Isler, M. Myers, M. Perzanowski, V. Rauh
Brigham & Women’s Hospital, Boston, MA, USA: A. A. Litonjua, S. T. Weiss
Columbia University, New York, NY, USA: F. P. Perer, J. B. Herbstman
Dartmouth College, Hanover, NH, USA: M. R. Karagas
Pennsylvania State University, State College, PA, USA: C. J. Newschaffer
Children’s Hospital of Philadelphia, Philadelphia, PA, USA: R. T. Schultz
Johns Hopkins University, Baltimore, MD, USA: H. E. Volk
Kaiser Permanente, Oakland, CA, USA: L. A. Croen
Kennedy Krieger Institute, Baltimore, MD, USA: R. J. Landa
University of California, Davis, Davis, CA, USA: R. J. Schmidt, S. Ozonoff
University of North Carolina, Chapel Hill, Chapel Hill, NC, USA: J. Piven
University of Washington, Seattle, WA, USA: S. R. Dager, D. Mayock
Emory University, Atlanta, GA, USA: A. L. Dunlop, P. A. Brennan, E. J. Corwin
Harvard Pilgrim Health Care, Boston, MA, USA: E. Oken, K. P. Kleinman
Icahn School of Medicine at Mount Sinai, Boston, MA, USA: R. J. Wright, R. O. Wright
Boston Children’s Hospital, Boston, MA, USA: M. B. Enlow
Kaiser Permanente, Oakland, CA, USA: A. Ferrara, L. A. Croen
Massachusetts General Hospital, Boston, MA, USA: C. A. Camargo
Michigan State University, East Lansing, MI, USA: N. Paneth, M. R. Elliott, P. McKane, J. M. Kerver, D. M. Ruden
Henry Ford Health System, Detroit, MI, USA: C. Barone
Wayne State University, Detroit, MI, USA: R. M. Douglas
Memorial Hospital of Rhode Island, Pawtucket, RI, USA: S. Deoni, V. A. D’Sa
Brown University, Providence, RI, USA: J. Braun
Johns Hopkins University School of Medicine, Baltimore, MD, USA: S. Carnell
The Translational Genomics Research Institute, Phoenix, AZ, USA: M. Huentelman
University of California, Davis, Davis, CA, USA: H. G. Mueller, J. L. Wang
University of Colorado Boulder, Boulder, CO, USA: M. LeBourgeois
Wellesley College, Wellesley, MA, USA: V. Klepac-Ceraj
Women & Infants Hospital, Providence, RI, USA: K. Matteson
New York State Psychiatric Institute at Columbia University, New York, NY, USA: C. S. Duarte, G. J. Canino, C. E. Monk, J. E. Posner
New York University, New York, NY, USA: C. B. Blair
New York University School of Medicine, New York, NY, USA: L. Trasande
Northeastern University, Boston, MA, USA: A. N. Alshawabkeh
Oregon Health & Science University, Portland, OR, USA: C. T. McEvoy, E. R. Spindel
University of California, Davis, CA, USA: I. Hertz-Picciotto, D. H. Bennett, J. B. Schweitzer
University of Colorado Anschutz Medical Campus, Aurora, CO, USA: D. Dabelea
University of Illinois, Urbana, Champaign, IL, USA: S. L. Schantz
University of California, San Francisco, CA, USA: T. Woodruff
University of New Mexico, Albuquerque, NM, USA: J. L. Lewis
University of North Carolina, Chapel Hill, Chapel Hill, NC, USA: M. O’Shea, R. Fry
University of Oregon, Eugene, OR, USA: L. D. Leve
George Washington University, Washington, DC, USA: J. M. Ganiban
Penn State, University Park, PA, USA: J. M. Neiderhiser
University of Pittsburgh, Pittsburgh, PA, USA: A. E. Hipwell, K. E. Keenan
University of Rochester, New York, NY, USA: T. G. O’Connor, C. Buss, R. K. Miller, P. D. Wadhwa
Magee-Women’s Hospital, University of Pittsburgh, Pittsburgh, PA, USA: H. N. Simhan
University of Southern California, Los Angeles, CA, USA: F. D. Gilliland, C. V. Breton
University of Utah, Salt Lake City, UT, USA: J. B. Stanford, E. B. Clark, C. Porucznik
University of Washington, Seattle, WA, USA: C. Karr, S. Sathyanarayana
University of California, San Francisco, CA, USA: K. Z. Lewinn, N. R. Bush
University of Tennessee Health Sciences Center, Memphis, TN, USA: F. A. Tylavsky
University of Wisconsin-Madison, Madison, WI, USA: J. Gern
Boston University, Boston, MA, USA: G. O’Connor
Brigham & Women’s Hospital, Boston, MA, USA: D. Gold
Columbia University, New York, NY, USA: R. Miller
Henry Ford Health System, Detroit, MI, USA: C. Johnson, D. Ownby, E. Zoratti
Johns Hopkins University, Baltimore, MD, USA: R. Wood
Marshfield Clinic Research Foundation, Marshfield, WI, USA: C. Bendixsen
University of Cincinnati, Cincinnati, OH, USA: G. K. Hershey
Vanderbilt University Medical Center, Nashville, TN, USA: T. Hartert
Washington University, St. Louis, MO, USA: L. Bacharier
Women & Infants Hospital of Rhode Island, Providence, RI, USA: B. Lester
Emory University, Atlanta, GA, USA: C. J. Marsit
Rights and permissions
About this article
Cite this article
Buckley, J.P., Barrett, E.S., Beamer, P.I. et al. Opportunities for evaluating chemical exposures and child health in the United States: the Environmental influences on Child Health Outcomes (ECHO) Program. J Expo Sci Environ Epidemiol 30, 397–419 (2020). https://doi.org/10.1038/s41370-020-0211-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41370-020-0211-9
Keywords
This article is cited by
-
Geochemical Investigation of OCPs in the Rivers Along with Drains and Groundwater Sources of Eastern Punjab, Pakistan
Exposure and Health (2024)
-
Addressing systemic problems with exposure assessments to protect the public’s health
Environmental Health (2023)
-
A state-of-the-science review and guide for measuring environmental exposure biomarkers in dried blood spots
Journal of Exposure Science & Environmental Epidemiology (2023)
-
Epigenomic signatures reveal mechanistic clues and predictive markers for autism spectrum disorder
Molecular Psychiatry (2023)
-
Linking complex disease and exposure data—insights from an environmental and occupational health study
Journal of Exposure Science & Environmental Epidemiology (2023)