Abstract
The founder variant DHCR7:c.964-1G>C causing autosomal recessive Smith–Lemli–Opitz (SLOS) was introduced into the Israeli preconception carrier program for Ashkenazi Jews in 2017 because of the high carrier frequency in this population (2.3%). Other disease-causing variants in DHCR7 are relatively rare in Israeli population. Discrepancy between the carrier frequency and disease prevalence raises the question of the actual risks for affected offspring for couples detected by the screening program. We performed a literature review of all relevant publications regarding homozygous DHCR7:c.964-1G>C fetuses/patients. We also collected clinical data about couples identified in the national screening program, including reproductive history. Out of 32 homozygous fetuses, six died in utero, 11 pregnancies were terminated during second trimester, and 15 children were born. All died between first days of life till 3 months of age. Reproductive history of SLOS-at-risk couples showed that after correction for ascertainment bias, out of 61 pregnancies, there was an absence of affected fetuses/children and an excess of miscarriages even if assumed that all the homozygous fetuses were miscarried. Out of these, eight families were Israelis, they had a total of one sick child, 21 healthy children, and 21 miscarriages. Our observations support the previous knowledge that homozygosity for c.964-1G>C in DHCR7 leads to a severe phenotype or early miscarriage. An unexpected observation was the excess of early miscarriages. This phenomenon is unclear and awaits further studies.
Similar content being viewed by others
Introduction
Smith–Lemli–Opitz (SLOS, OMIM #270400) is an autosomal recessive disorder characterized by variable expression of phenotypes including multiple congenital malformations, dysmorphic features, metabolic errors, and intellectual disability [1,2,3]. The disease etiology is biallelic variants in the DHCR7 gene resulting in deficiency of 7-dehydrocholesterol reductase enzyme and impaired cholesterol metabolism. Upon evaluating genotype–phenotype correlation, it seems that the severe extreme phenotype is associated with biallelic null variants [4]. In many populations the carrier frequency of DHCR7 variants is relatively high; while the prevalence of SLOS patients is substantially lower than expected [5, 6]. An example is the founder splice variant DHCR7: c.964-1G>C (rs138659167, NM_001360.2:c.964-1G>C, chr11: 71146886-1G>C), previously named IVS8-1G>C, which is relatively frequent in various populations with the highest frequency among Ashkenazi Jews [3, 7] (http://gnomad-old.broadinstitute.org/variant/11-71146886-C-G). Since the variant DHCR7:c.964-1G>C was related in many cases with a severe phenotype it was included in universal screening panels [3]. The high carrier frequency among Ashkenazi Jews (2.3%) and the severity of the disease among homozygotes correspond to the criteria of the Israeli Medical Geneticists Association for preconception carrier screening [8]. Therefore, screening for DHCR7:c.964-1G>C was included in the recommendations which led to its inclusion to the national carrier screening program funded by the Israeli ministry of health since 2017. However, SLOS is not known to be one of the frequent diseases diagnosed among Ashkenazi Jews and this discrepancy with the variant carrier frequency raises the question of the actual risk for couples detected by the screening program to have an affected child. The present study was initiated in order to resolve this discrepancy and with the aim to provide accurate counseling to the couples identified through the screening program.
Methods
All the publications available to us via “Pubmed” regarding SLOS, in which phenotypic details were given about DHCR7:c.964-1G>C homozygous fetuses/patients were included. In addition, we aimed to reach every relevant article cited by one of these studies. We also collected data regarding at-risk couples in which the partners were both carriers for this variant and details about all their pregnancies were given.
All the Israeli medical geneticists received our request requiring information about cases diagnosed as homozygotes for DHCR7:c.964-1G>C or at-risk couples detected through the national carrier-screening program. Details on all the pregnancies of carrier couples were collected anonymously including year of birth of the parents, their ethnicity, and the reproductive history of every couple preceding molecular diagnosis of SLOS carrier state. This included number of pregnancies and the outcome of every pregnancy i.e., normal offspring, spontaneous miscarriage (and timing), or an offspring with SLOS.
The study was approved by our local institutional review board (number of approval 0083-18-HMO).
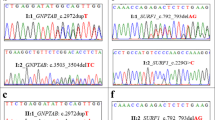
Data that were not yet submitted, were deposited in ClinVar. accession number for DHCR7 variant in ClinVar: SCV000998809.1 (there are another 37 citations regarding the variant at https://www.ncbi.nlm.nih.gov/clinvar/variation/93725/).
Results
Homozygosity for the DHCR7 c.964-1G>C variant
Out of 32 homozygotes (31 are from the literature, including one pair of dizygotic twins), 11 fetuses (34%) were terminated during the second trimester, six (19%) died in utero (intrauterine fetal death, IUFD), and 15 children (47%) were born (Supplementary Table 1).
Eleven terminations of pregnancies
Three fetuses had a severe phenotype without specific details [4]. The other eight fetuses are described in details with severe multiple various malformations [4, 9,10,11,12,13]. Three had thickened nuchal translucency (3, 3.2, and 4.2 mm), while in the other five fetuses it was not reported (Supplementary Table 2).
Among the various fetal malformations, intrauterine growth restriction was described in six out of eight (75%) fetuses and limbs anomalies in seven out of eight (87%). Lung lobulation anomalies and renal anomalies were described in six each out of those eight (75%, 75%). Alobar holoprosencephaly was reported in two fetuses (2/8, 25%). In three male fetuses ambiguous genitalia was described but fetal sex is not mentioned for all fetuses.
Fifteen affected children born
Fourteen children homozygous for DHCR7:c.964-1G>C were previously reported in the literature [4, 12,13,14,15,16,17,18] and one child is reported in the present study. Among these, nine patients were described to have multiple malformations, two are described to have “severe” phenotype without further details and another four have no clinical description except for age at death (Supplementary Table 3).
The age of death was available for 14 children with a range of 1 day to 3 months (median 1 month). The longest survival was reported for an Israeli child that died at the age of 3 months following toxic megacolon. Four other children died due to either electrolyte abnormalities together with necrotizing enterocolitis (NEC), respiratory insufficiency with constant vomiting, congestive heart failure together with NEC, or pneumonia. For other cases, the cause of death was not reported.
Reproductive history of carrier couples
Couples with SLOS fetuses/offspring
Details regarding reproductive history were available for eight couples in whom a diagnosis of an affected SLOS fetus/child was made (Table 1). Out of 21 pregnancies excluding the pregnancy in which SLOS was diagnosed, there were nine healthy offspring and 12 early miscarriages (Supplementary Table 4).
An additional Israeli carrier couple (IL7) was not included in the calculations since SLOS was not suspected and the diagnosis was done following exome sequencing of a spontaneously miscarried fetus performed to investigate a possible etiology for seven previous sequential spontaneous early miscarriages with no children (in three cases the pregnancy was with a surrogate mother). In a spontaneous pregnancy following this diagnosis, amniocentesis was negative for SLOS (by molecular test) and a healthy child was born.
Carrier couples from Israel diagnosed in the screening program
There were ten couples diagnosed in the screening program. In five couples (Table 2), 33 pregnancies were reported before determining that the couple was at risk, 14 were first or early second trimester miscarriages, and 19 were of children not affected with SLOS. In the other five couples, no pregnancies were reported, or the diagnosis was made during the ongoing first pregnancy.
Incidence of SLOS due to homozygosity for the DHCR7 c.964-1G>C variant among Ashkenazi Jews in Israel
Since the molecular diagnosis of SLOS is possible a single homozygous child and one homozygous miscarried fetus were diagnosed in Israel. Approximately one million Ashkenazi Jewish newborn were born in Israel in 1999–2018 (out of more than 2.2 million Jewish babies some 40–50% of them being Ashkenazi) [19].
Discussion
The data presented here support the previous knowledge that homozygosity for c.964-1G>C in DHCR7 leads to either early spontaneous miscarriage and IUFD, or a severe phenotype including severe fetal malformations, most of which are diagnosed during pregnancy. The homozygous children died in early infancy but it is plausible that with medical support some may live longer. Conversely, a totally unexpected observation was made among 14,614 individuals examined in UK10K project, since two were homozygous for 964-1G>C in DHCR7 with no reported clinical manifestations of the disease [20]. However, the results could not be validated due to insufficient remaining DNA from the samples and, out of hundreds of thousands of adults being sequenced or screened for DHCR7 variants none were found to be homozygous for c.964-1G>C in DHCR7.
The results presented here confirm that in couples who are carriers of c.964-1G>C, the actual risk for an affected child to be born is significantly less than 25%. It was calculated that according to the carrier frequency of the variants in diverse populations, some 43–88% of the DHCR7 homozygotes are miscarried [3]. Among the eight families diagnosed as the result of an affected fetus/child, in the 21 additional pregnancies there were no other affected children. However, the sample is too small to allow calculating the actual risk for an affected child to be born and we were not able to recruit additional families with affected probands through enquiries made to several investigators around the world that published SLOS family studies. The data regarding families detected through the screening program in Israel, in which the pregnancies before the diagnosis were investigated, are obviously biased since a priori they are couples at risk that did not have an affected child.
In the present study we observed in addition to the shortage of nonaffected children an excess of early miscarriages. Among the eight families diagnosed as the result of an affected fetus/child, in the 21 additional pregnancies if assumed that all the homozygous fetuses were miscarried, the expected miscarriage number would have been five (instead of the 12 observed), and expected number of nonaffected children would be 16 (instead of nine observed) (χ2 = 3.500; p = 0.0614). A similar observation was made in the analysis of the pregnancies in couples detected through the screening: out of 32 pregnancies, the expected number would have been eight previous miscarriages (instead of the 14 observed) and 24 nonaffected children (instead of 18 observed) (χ2 = 2.4935; p = 0.1143). This excess of spontaneous early miscarriages was evident particularly in some of the couples and the Israeli family described above (IL7) that was not included in these calculations, in which the diagnosis was made by exome sequencing of a spontaneously miscarried fetus after having seven spontaneous miscarriages and later had a normal child. If all the data are aggregated out of 61 pregnancies, if it is assumed that all the homozygous fetuses were miscarried, 15 miscarriages were expected (instead of the 33 observed) and 46 nonaffected children (instead of 28 observed) (χ2 = 11.1284; p = 0.0008).
The reasons for the high rate of early first trimester spontaneous miscarriages in the couples at risk are not clear. One option may be that since in the general population miscarriages rate is up to 20% of the pregnancies [21,22,23], this may have caused the sense of an excess of miscarriages. In the aggregated data 12 spontaneous miscarriages out of 61 pregnancies would have been expected and out of the 49 other pregnancies, if assumed that all the homozygous fetuses were miscarried, 12 miscarriages were expected (instead of the 21 observed) and 37 nonaffected children (instead of 28 observed). Another possibility may be that the maternal carrier state alone is harmful for the developing embryo. It may be proposed that carrying the c.964-1G>C variant promotes a uterine environment that lacks cholesterol building blocks or increases abundant in toxic metabolites [24]. Moreover, SLOS as a consequence of these observations, testing for variants in DHCR7 gene should be considered to be added to the investigations performed in couples with recurrent early miscarriages in particular in populations in which variants in DCHR7 are relatively frequent.
In preconception genetic counseling, if prenatal diagnosis is the option preferred by the couple at risk, the fact that most affected fetuses are spontaneously miscarried early in pregnancy should be taken into account. In addition, because of the increased risk of early spontaneous miscarriages, amniocentesis may be a better option than chorionic villous sampling although it is performed later in pregnancy.
In the case of the c.964-1G>C variant in DHCR7, more data are needed to determine the actual risk for an affected child for couples at risk. Such study is ongoing and will include the prospective follow-up of the spontaneous pregnancies of the couples detected through the screening program.
References
Nowaczyk MJ, Irons MB. Smith–Lemli–Opitz syndrome: phenotype, natural history, and epidemiology. Am J Med Genet C Semin Med Genet. 2012;160C:250–62.
Jira PE, Waterham HR, Wanders RJ, Smeitink JA, Sengers RC, Wevers RA. Smith–Lemli–Opitz syndrome and the DHCR7 gene. Ann Hum Genet. 2003;67:269–80.
Lazarin GA, Haque IS, Evans EA, Goldberg JD. Smith–Lemli–Opitz syndrome carrier frequency and estimates of in utero mortality rates. Prenat Diagn. 2017;37:350–5.
Witsch-Baumgartner M, Fitzky BU, Ogorelkova M, Kraft HG, Moebius FF, Glossmann H, et al. Mutational spectrum in the Delta7-sterol reductase gene and genotype-phenotype correlation in 84 patients with Smith–Lemli–Opitz syndrome. Am J Hum Genet. 2000;66:402–12.
Nowaczyk MJ, Waye JS, Douketis JD. DHCR7 mutation carrier rates and prevalence of the RSH/Smith–Lemli–Opitz syndrome: where are the patients? Am J Med Genet A. 2006;140:2057–62.
Battaile KP, Battaile BC, Merkens LS, Maslen CL, Steiner RD. Carrier frequency of the common mutation IVS8-1G>C in DHCR7 and estimate of the expected incidence of Smith–Lemli–Opitz syndrome. Mol Genet Metab. 2001;72:67–71.
Lek M, Karczewski KJ, Minikel EV, Samocha KE, Banks E, Fennell T, et al. Analysis of protein-coding genetic variation in 60,706 humans. Nature. 2016;536:285–91.
Zlotogora J, Grotto I, Kaliner E, Gamzu R. The Israeli national population program of genetic carrier screening for reproductive purposes. Genet Med. 2016;18:203–6.
Quélin C, Loget P, Verloes A, Bazin A, Bessières B, Laquerrière A, et al. Phenotypic spectrum of fetal Smith–Lemli–Opitz syndrome. Eur J Med Genet. 2012;55:81–90.
Travessa A, Dias P, Rocha P, Sousa AB. Prenatal diagnosis of holoprosencephaly associated with Smith–Lemli–Opitz syndrome (SLOS) in a 46,XX fetus. Taiwan J Obstet Gynecol. 2017;56:541–4.
Moosa S, Loeys B, Altmüller J, Mortier G, Nürnberg P, Li Y, et al. Metatarsal bony syndactyly in 2 fetuses with Smith–Lemli–Opitz syndrome: an under-recognized part of the clinical spectrum. Clin Genet. 2017;92:342–3.
Nowaczyk MJ, Farrell SA, Sirkin WL, Velsher L, Krakowiak PA, Waye JS, et al. Smith–Lemli–Opitz (RHS) syndrome: holoprosencephaly and homozygous IVS8-1G->C genotype. Am J Med Genet. 2001;103:75–80.
Goldenberg A, Chevy F, Bernard C, Wolf C, Cormier-Daire V. Clinical characteristics and diagnosis of Smith–Lemli–Opitz syndrome and tentative phenotype–genotype correlation: report of 45 cases. Arch Pediatr. 2003;10:4–10.
Jira PE, Wanders RJ, Smeitink JA, De Jong J, Wevers RA, Oostheim W, et al. Novel mutations in the 7-dehydrocholesterol reductase gene of 13 patients with Smith–Lemli–Opitz syndrome. Ann Hum Genet. 2001;65:229–36.
Lanthaler B, Steichen-Gersdorf E, Kollerits B, Zschocke J, Witsch-Baumgartner M. Maternal ABCA1 genotype is associated with severity of Smith–Lemli–Opitz syndrome and with viability of patients homozygous for null mutations. Eur J Hum Genet. 2013;21:286–93.
Balogh I, Koczok K, Szabó GP, Török O, Hadzsiev K, Csábi G, et al. Mutational spectrum of smith-lemli-opitz syndrome patients in hungary. Mol Syndromol. 2012;3:215–22.
Donoghue SE, Pitt JJ, Boneh A, White SM. Smith–Lemli–Opitz syndrome: clinical and biochemical correlates. J Pediatr Endocrinol Metab. 2018;31:451–9.
Scalco FB, Correa-Cerro LS, Wassif CA, Porter FD, Moretti-Ferreira D. DHCR7 mutations in Brazilian Smith–Lemli–Opitz syndrome patients. Am J Med Genet A. 2005;136:278–81.
Statistical Abstracts of Israel. Jerusalem: Central Bureau of Statistics; 2018.
Chen R, Shi L, Hakenberg J, Naughton B, Sklar P, Zhang J, et al. Analysis of 589,306 genomes identifies individuals resilient to severe Mendelian childhood diseases. Nat Biotechnol. 2016;34:531–8.
Rossen LM, Ahrens KA, Branum AM. Trends in risk of pregnancy loss among US women, 1990–2011. Paediatr Perinat Epidemiol. 2018;32:19–29.
Dhaded SM, Somannavar MS, Jacob JP, McClure EM, Vernekar SS, Yogesh Kumar S, et al. Early pregnancy loss in Belagavi, Karnataka, India 2014–2017: a prospective population-based observational study in a low-resource setting. Reprod Health. 2018;15(Suppl 1):95.
Ammon Avalos L, Galindo C, Li DK. A systematic review to calculate background miscarriage rates using life table analysis. Birth Defects Res A Clin Mol Teratol. 2012;94:417–23.
Korade Z, Genaro-Mattos TC, Tallman KA, Liu W, Garbett KA, Koczok K. et al. Vulnerability of DHCR7+/− mutation carriers to aripiprazole and trazodone exposure. J Lipid Res. 2017;58:2139–46.
Acknowledgements
We would like to thank our collaborators all across the country that searched for relevant data. Data that were not yet submitted, were deposited in ClinVar. accession number for DHCR7 variant in ClinVar: SCV000998809.1 (There are 38 citations regarding the variant at https://www.ncbi.nlm.nih.gov/clinvar/variation/93725/).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Daum, H., Meiner, V., Michaelson-Cohen, R. et al. Smith–Lemli–Opitz syndrome: what is the actual risk for couples carriers of the DHCR7:c.964-1G>C variant?. Eur J Hum Genet 28, 938–942 (2020). https://doi.org/10.1038/s41431-020-0577-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41431-020-0577-0
This article is cited by
-
Miscarriage risk assessment: a bioinformatic approach to identifying candidate lethal genes and variants
Human Genetics (2024)
-
Mendelian inheritance revisited: dominance and recessiveness in medical genetics
Nature Reviews Genetics (2023)
-
Deficit of homozygosity among 1.52 million individuals and genetic causes of recessive lethality
Nature Communications (2023)