Abstract
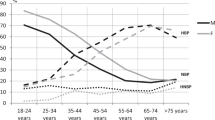
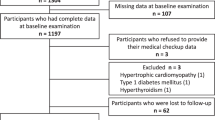
In obesity, cardiometabolic risk markers show worsening trends with increasing blood pressure (BP). We assumed that risk markers show similar trends across BP categories (normotension, high normal BP, hypertension) in metabolic abnormalities-free subjects (without obesity, insulin resistance, atherogenic dyslipidemia, hyperuricemia, microinflammation) and those presenting them. Data from 2547 (48.1% males) subjects aged 16–23 years were analyzed. The prevalence of males increased across BP categories. Forty-seven percent of individuals with elevated BP were metabolic abnormalities-free. Among 1461 metabolic abnormalities-free subjects, 9% had high normal BP, and 4% hypertension; among 1086 individuals presenting metabolic abnormalities, the prevalence reached 13% and 6%, respectively, (p < 0.001). Both groups displayed similar BP values in corresponding BP categories and significant trends in markers of adiposity, insulin resistance, HDL-cholesterol, atherogenic index of plasma, uric acid, adiponectinemia, and antioxidant capacity of plasma across BP categories. In metabolic abnormalities-free individuals, also significant trends in soluble receptors for advanced glycation end products were revealed. Continuous metabolic syndrome score, a measure of cardiometabolic risk, increased across BP categories regardless of presence or absence of metabolic abnormalities. Multivariate regression models selected male gender, fat-free mass, and uric acid as significant independent predictors for determining BP. Our data emphasize that having a BP outside the normal range significantly worsens risk for cardiometabolic disease in young individuals even if the thresholds for any of the risk factors are not exceeded. Longitudinal studies are needed to assess whether in patients with elevated BP the prognosis of adverse outcomes differs between those presenting and not presenting metabolic abnormalities.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Psaty BM, Furberg CD, Kuller LH, Cushman M, Savage PJ, Levine D, et al. Association between blood pressure level and the risk of myocardial infarction, stroke, and total mortality: the cardiovascular health study. Arch Intern Med. 2001;161:1183–92.
Lauer RM, Clarke WR. Childhood risk factors for high adult blood pressure: the Muscatine Study. Pediatrics. 1989;84:633–41.
Kelly RK, Magnussen CG, Sabin MA, Cheung M, Juonala M. Development of hypertension in overweight adolescents: a review. Adolesc Health Med Ther. 2015;6:171–87.
Noronha JA, Medeiros CC, Cardoso Ada S, Gonzaga NC, Ramos AT, Ramos AL. C-reactive protein and its relation to high blood pressure in overweight or obese children and adolescents. Rev Paul Pediatr. 2013;31:331–7.
Freedman DS, Dietz WH, Srinivasan SR, Berenson GS. The relation of overweight to cardiovascular risk factors among children and adolescents: the Bogalusa Heart Study. Pediatrics. 1999;103:1175–82.
De Las Heras J, Lee S, Bacha F, Tfayli H, Arslanian S. Cross-sectional association between blood pressure, in vivo insulin sensitivity and adiponectin in overweight adolescents. Horm Res Paediatr. 2011;76:379–85.
Mokan M, Galajda P, Pridavkova D, Tomaskova V, Sutarik L, Krucinska L, et al. Prevalence of diabetes mellitus and metabolic syndrome in Slovakia. Diabetes Res Clin Pr. 2008;81:238–42.
Gurecka R, Koborova I, Sebek J, Sebekova K. Presence of cardiometabolic risk factors is not associated with microalbuminuria in 14-to-20-years old Slovak adolescents: a cross-sectional, population study. PLoS ONE. 2015;10:e0129311.
Sidoti A, Nigrelli S, Rosati A, Bigazzi R, Caprioli R, Fanelli R, et al. Body mass index, fat free mass, uric acid, and renal function as blood pressure levels determinants in young adults. Nephrology. 2017;22:279–85.
Dobiasova M, Frohlich J. The plasma parameter log (TG/HDL-C) as an atherogenic index: correlation with lipoprotein particle size and esterification rate in apoB-lipoprotein-depleted plasma (FER(HDL)). Clin Biochem. 2001;34:583–8.
Karlik M, Valkovic P, Hancinova V, Krizova L, Tothova L, Celec P. Markers of oxidative stress in plasma and saliva in patients with multiple sclerosis. Clin Biochem. 2015;48:24–8.
Lurbe E, Agabiti-Rosei E, Cruickshank JK, Dominiczak A, Erdine S, Hirth A, et al. 2016 European Society of Hypertension guidelines for the management of high blood pressure in children and adolescents. J Hypertens. 2016;34:1887–920.
Soldatovic I, Vukovic R, Culafic D, Gajic M, Dimitrijevic-Sreckovic V. siMS score: simple method for quantifying metabolic syndrome. PLoS ONE. 2016;11:e0146143.
McNiece KL, Poffenbarger TS, Turner JL, Franco KD, Sorof JM, Portman RJ. Prevalence of hypertension and pre-hypertension among adolescents. J Pediatr. 2007;150:640–4. 644.e1.
Dulskiene V, Kuciene R, Medzioniene J, Benetis R. Association between obesity and high blood pressure among Lithuanian adolescents: a cross-sectional study. Ital J Pediatr. 2014;40:102.
Menghetti E, Strisciuglio P, Spagnolo A, Carletti M, Paciotti G, Muzzi G, et al. Hypertension and obesity in Italian school children: the role of diet, lifestyle and family history. Nutr Metab Cardiovasc Dis. 2015;25:602–7.
Sebekova K, Sebek J. Continuous metabolic syndrome score (siMS) enables quantification of severity of cardiometabolic affliction in individuals not presenting with metabolic syndrome. Bratisl Lek Listy. 2018;119:675–8.
DeBoer MD, Gurka MJ, Woo JG, Morrison JA. Severity of metabolic syndrome as a predictor of cardiovascular disease between childhood and adulthood: the Princeton Lipid Research Cohort Study. J Am Coll Cardiol. 2015;66:755–7.
Pandit D, Chiplonkar S, Khadilkar A, Kinare A, Khadilkar V. Efficacy of a continuous metabolic syndrome score in Indian children for detecting subclinical atherosclerotic risk. Int J Obes. 2011;35:1318–24.
Jung KJ, Jee YH, Jee SH. Metabolic risk score and vascular mortality among Korean adults. Asia Pac J Public Health. 2017;29:122–31.
DeBoer MD, Gurka MJ. Clinical utility of metabolic syndrome severity scores: considerations for practitioners. Diabetes Metab Syndr Obes. 2017;10:65–72.
Feig DI, Johnson RJ. The role of uric acid in pediatric hypertension. J Ren Nutr. 2007;17:79–83.
King C, Lanaspa MA, Jensen T, Tolan DR, Sanchez-Lozada LG, Johnson RJ. Uric acid as a cause of the metabolic syndrome. Contrib Nephrol. 2018;192:88–102.
Kuwabara M, Borghi C, Cicero AFG, Hisatome I, Niwa K, Ohno M, et al. Elevated serum uric acid increases risks for developing high LDL cholesterol and hypertriglyceridemia: a five-year cohort study in Japan. Int J Cardiol. 2018;261:183–8.
Rochlani Y, Pothineni NV, Mehta JL. Metabolic syndrome: does it differ between women and men? Cardiovasc Drugs Ther. 2015;29:329–38.
Brambilla P, Antolini L, Street ME, Giussani M, Galbiati S, Valsecchi MG, et al. Adiponectin and hypertension in normal-weight and obese children. Am J Hypertens. 2013;26:257–64.
Dinh QN, Drummond GR, Sobey CG, Chrissobolis S. Roles of inflammation, oxidative stress, and vascular dysfunction in hypertension. Biomed Res Int. 2014;2014:406960.
Litwin M, Michalkiewicz J, Niemirska A, Gackowska L, Kubiszewska I, Wierzbicka A, et al. Inflammatory activation in children with primary hypertension. Pediatr Nephrol. 2010;25:1711–8.
Turi S, Friedman A, Bereczki C, Papp F, Kovacs J, Karg E, et al. Oxidative stress in juvenile essential hypertension. J Hypertens. 2003;21:145–52.
Papatheodorou L, Weiss N. Vascular oxidant stress and inflammation in hyperhomocysteinemia. Antioxid Redox Signal. 2007;9:1941–58.
Hudson BI, Carter AM, Harja E, Kalea AZ, Arriero M, Yang H, et al. Identification, classification, and expression of RAGE gene splice variants. FASEB J. 2008;22:1572–80.
Stern D, Yan SD, Yan SF, Schmidt AM. Receptor for advanced glycation endproducts: a multiligand receptor magnifying cell stress in diverse pathologic settings. Adv Drug Deliv Rev. 2002;54:1615–25.
Sebekova K, Krivosikova Z, Gajdos M. Total plasma Nepsilon-(carboxymethyl)lysine and sRAGE levels are inversely associated with a number of metabolic syndrome risk factors in non-diabetic young-to-middle-aged medication-free subjects. Clin Chem Lab Med. 2014;52:139–49.
Geroldi D, Falcone C, Emanuele E, D’Angelo A, Calcagnino M, Buzzi MP, et al. Decreased plasma levels of soluble receptor for advanced glycation end-products in patients with essential hypertension. J Hypertens. 2005;23:1725–9.
Selvin E, Halushka MK, Rawlings AM, Hoogeveen RC, Ballantyne CM, Coresh J, et al. sRAGE and risk of diabetes, cardiovascular disease, and death. Diabetes. 2013;62:2116–21.
Acknowledgements
The authors wish to thank all those who put their effort toward the accomplishment of the Respect for Health study.
Funding
This study was funded by the Scientific Grant Agency of the Ministry of Education, Science, Research and Sport of the Slovak Republic and the Slovak Academy of Sciences (VEGA), grant no. 1/0637/13; the Slovak Research and Development Agency (APVV), grant no. 0447–12; and Bratislava Self-Governing Region. The sponsors had no role in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
All authors were involved in developing the study concept, interpretation of results, editing, revising the article critically, and have approved the final version of this submission. RG, MCs and IK contributed to acquisition of data and helped to establish the database. JS undertook all the statistical analysis of the data. KS contributed to study design and wrote the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Šebeková, K., Gurecká, R., Csongová, M. et al. Elevated blood pressure-associated cardiometabolic risk factors and biomarkers in 16–23 years old students with or without metabolic abnormalities. J Hum Hypertens 35, 37–48 (2021). https://doi.org/10.1038/s41371-020-0309-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-020-0309-5