Abstract
Objectives
To compare the dynamic visual acuity (DVA) following implantation of trifocal with monofocal intraocular lenses (IOL) and using a novel test system.
Methods
The present research was a retrospective, multicenter clinical study. Two hundred and ten eyes of 149 patients that underwent cataract phacoemulsification and IOL implantation were enrolled. One hundred and ten eyes of patients received trifocal (AT LISA tri839MP, Carl Zeiss Meditec, Germany) and 100 eyes received monofocal (Tecnis ZCB00, Abbott, United States) lenses and were evaluated 3 months after implantation. Outcome measures included monocular uncorrected distance (UDVA), intermediate (UIVA) and near (UNVA) visual acuity and best corrected distance visual acuity (BCDVA; logMAR units); contrast sensitivity under photopic, mesopic, with glare conditions; and dynamic visual acuity using a self-developed system.
Results
There was no statistically significant difference in baseline characteristics between groups. Monocular UDVA, UIVA, and UNVA were significantly better (all p < 0.001) in the trifocal IOL group, but not BCDVA. The trifocal IOL group showed better contrast sensitivity under photopic, mesopic, with or without glare conditions (p < 0.05) and statistically significantly better dynamic vision at 15, 30, 60, and 90 degrees per second (dps) compared with the monofocal group (all p < 0.001). The strength of positive association only between UIVA and dynamic visual acuity increased as the velocity increased, but not UDVA or UNVA.
Conclusions
Diffractive trifocal IOL provides better postoperative full range vision acuity, contrast sensitivity, and dynamic vision compared with monofocal IOLs. And intermediate visual acuity is increasingly associated with DVA as the velocity increasing.
Similar content being viewed by others
Introduction
Globally, cataract is the leading cause of blindness [1]. Phacoemulsification and intraocular lens (IOL) implantation are routinely considered the standard of care for surgical management of cataracts [2]. As surgical techniques and IOL designs have improved, cataract surgery has evolved from a procedure with the simple goal of preventing blindness, to improving both vision, and quality of life for patients [3]. Traditional cataract management has primarily focused on improving static visual acuity (VA), however, rising patient expectations in the postoperative period have also increased the demand for enhanced vision, as an extension of quality of life relevant to improved dynamic visual acuity (DVA). DVA differs from static vision in that it describes the ability to identify the detail of an object as it moves relative to the observer [4]. DVA is transmitted through magnocellular pathways, unlike static vision [5]. DVA performance is known to decline with increasing age [6]. DVA degeneration is associated with an increased difficulty in completing everyday life tasks including sports activities and driving [7]. Our previous research has demonstrated greater loss in DVA for cataract patients and significant improvement of DVA following cataract surgery [8]. However, the contribution of different intraocular lens for enhanced DVA improvement were not investigated or compared before.
Conventional IOLs offer a specific field of focus often allowing for clear vision at near or distance, but rarely both [9]. Whereas multifocal IOLs provide better uncorrected clear VA at distance, intermediate and near [10]. The AT LISA tri 839MP (Carl Zeiss Meditec, Jena, Germany) is a diffractive IOL with a trifocal design [11]. Although previous studies have demonstrated that the AT LISA tri 839MP provides sustainable restoration of VA at near, intermediate, and distance following cataract surgery [12, 13], whether this all-distance VA improvement contributes to increased DVA following IOL implantation is unknown. Therefore, this study aims to compare DVA following intraocular implantation of either a diffractive trifocal or monofocal IOL following cataract phacoemulsification.
Materials and methods
Eligible patients with age-related cataract were enrolled from six referral centers. These included patients from the Peking University Third Hospital, Beijing, (68 patients with 100 eyes), and Hebei Eye Hospital, Hebei, (13 patients with 18 eyes) from the north, Chengdu Aier Eye Hospital, Sichuan, (11 patients with 19 eyes) from the southwest, Lanzhou Bright Eye Hospital, Gansu, (19 patients with 24 eyes), and Gansu Province Hospital Rehabilitation Center, Gansu, (12 patients with 19 eyes) from the northwest, and Daqing Oilfield General Hospital, Heilongjiang, (26 patients with 30 eyes), from the northeast. All patients underwent phacoemulsification cataract surgery by experienced surgeons and were implanted either trifocal (AT LISA tri 839MP, Carl Zeiss Meditec, Jena, Germany), (81 patients with 110 eyes) or monofocal (Tecnis ZCB00, Abbott, United States) (68 patients with 100 eyes).
The study was conducted in accordance with the ethical principles originating from the Declaration of Helsinki and its amendments, consistent with Good Clinical Practices and local regulatory requirements. Written informed consent was obtained from all patients and the protocols were reviewed and approved by the institutional review board of the six centers. The research was registered on Chinese Clinical Trial Registry with the number ChiCTR1800016964.
Patients were excluded from the study if they had corneal astigmatism >1.0D, other refractive media opacity, corneal disease, glaucoma, high myopia, macular degeneration, optic neuropathy, uveitis, retinal detachment, diabetic retinopathy, hypertensive retinopathy, complicated systemic disease or were incapable of completing study-related visits.
Clinical evaluation
Preoperative evaluation included uncorrected distance visual acuity (UDVA) (4 m, Early Treatment of Diabetic Retinopathy Study [ETDRS]), Goldmann applanation tonometry, slit lamp, ophthalmoscopy and biometry (IOL Master 500, Carl Zeiss Meditec, Jena, Germany).
Postoperative examinations were performed at 3 months following cataract surgery. Assessment procedures included all preoperative examinations in addition to monocular best corrected distance visual acuity (BCDVA) (4 m, ETDRS), monocular UIVA (66 cm, modified ETDRS for European-wide use for near and intermediate distance recordings, Precision Vision), monocular uncorrected near visual acuity (UNVA) (33 cm, modified ETDRS for European-wide use for near and intermediate distance recordings, Precision Vision), contrast sensitivity, and dynamic vision. Contrast sensitivity was examined under photopic, photopic with glare, mesopic, and mesopic with glare condition at 1.5, 3, 6, 12, and 18 cd/m2 (OPTEC 6500P, Chicago, USA). The subject was adapted in the darkness for 10 min before testing the mesopic condition.
Dynamic visual acuity
Assessment of DVA has been described in detail in our previous research [8]. The DVA examination system includes a self-developed program which runs on a laptop that projects optotypes (the letters H, O, T, and V) of horizontal movement onto a screen. The testing environment and user interface are demonstrated in Fig. 1. The dynamic optotypes were developed to be the same size as standard ETDRS charts with an adjustable speed, including 15, 30, 60, and 90 degrees per second (dps). The transformation between optotype size and DVA is summarized in Supplement Table 1.
The patient was required to sit 4 m away from the screen. The position of the projector was adjusted to create a 1-meter-wide image on the screen. The patient was initially trained to understand the motor pattern of the optotypes and be aware of the testing procedure. Once training was complete, the dynamic optotypes were projected on the screen and VA was recorded at varying speeds as logMAR.
Surgical technique
Standard technique of small incision phacoemulsification with IOL implantation was performed on each patient by experienced ophthalmologists. Topical anesthesia was applied for all cases after routine disinfection. The surgical area was exposed using a speculum. The main incision was performed into the limbus at the 11 O’clock position followed by an injection of a viscoelastic agent. Assisted incision was performed at the 3 O’clock position and a capsulorhexis was performed. Balanced salt solution was applied to hydrodissect the lens nucleus and cortex. Following phacoemulsification, a coaxial irrigation/aspiration needle was used to remove the residual cortex. The selected trifocal or monofocal IOL was implanted through the main incision into the capsule.
Statistical analysis
Statistical analysis was conducted applying SPSS (Version 23.0, International Business Machines Corp.). The Kolmogorov–Smirnov test was used to check the normality of the data distribution. Data were represented as mean ± standard deviation (SD) for continuous variables. For parametric statistical analysis, independent t-test was applied for comparison between two groups. Otherwise, nonparametric statistical tests were applied. The value of VA and contrast sensitivity were transformed to log value prior to analysis. In addition, a multiple linear regression model was established to evaluate the effect of static visual acuity at different distances on DVA at different adjusting velocities. p < 0.05 was considered statistically significant.
Results
The present study enrolled 81 patients with 110 eyes (39 males) that received implantation of a trifocal IOL and 68 patients with 100 eyes (33 males) that received a monofocal IOL. The mean age was 63.2 ± 6.8 years in the trifocal IOL group (45–79 years), and 65.1 ± 6.6 years in the monofocal IOL group (52–80 years). No significant difference in age (p = 0.236) and gender (p = 0.314) were observed between the two groups.
Visual acuity
Visual acuity outcomes preoperatively and 3 months postoperatively are summarized in Table 1. No significant difference was observed in preoperative UDVA between the two groups. Significant improvements of UDVA was shown 3 months postoperatively for both groups (p < 0.001). At 3 months postoperatively, monocular BCVDA was the same between the two groups (p = 0.77), while the UD (p < 0.001), intermediate (p < 0.001) and near (p < 0.001) VA were significant better in the trifocal IOL group when compared with the monofocal IOL group.
Contrast sensitivity
The contrast sensitivity in different spatial frequencies under photopic, mesopic, photopic with glare and mesopic with glare conditions for each group are summarized in Table 2. The group that received the trifocal IOL demonstrated better contrast sensitivity under photopic, mesopic, photopic with glare conditions in all spatial frequencies (p < 0.05) except at 18 cpd (p = 0.384; p = 0.415; p = 0.523). For mesopic with glare conditions, the trifocal IOL group demonstrated significantly better contrast sensitivity except at 1.5 cpd spatial frequency (p = 0.465).
Dynamic visual acuity
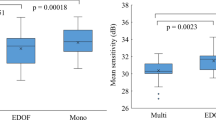
The results of DVA 3 months postoperatively is summarized in Table 3. The DVA of the trifocal IOL group was logMAR 0.183 ± 0.125 at 15 dps, 0.254 ± 0.127 at 30 dps, 0.306 ± 0.135 at 60 dps, and 0.351 ± 0.135 at 90 dps, which was significantly better when compared with the monofocal IOL group, which were LogMAR 0.249 ± 0.24 at 15 dps (p < 0.001), 0.335 ± 0.111 at 30 dps (p < 0.001), 0.356 ± 0.108 at 60 dps (p < 0.001), and 0.406 at 90 dps (p < 0.001).
Association between static and dynamic visual acuity
The results of multiple linear regression analysis for static VA of different distance and DVA of different velocities, considering age, gender, and lens type are summarized in Table 4. DVA of 15 and 30 dps was only significantly positively associated UDVA. And the UIVA was positively correlated with DVA at the speed of 60 and 90 dps. The standardized coefficient for static VA at different distances demonstrated that the strength of the positive association between DVA and UDVA decreased as the velocity increased. However, the strength of positive association between UIVA and DVA increased as the velocity increased.
Discussion
The present study applied a novel standardized testing system to evaluate postoperative DVA following IOL implantation and demonstrated that patients implanting of trifocal IOL experience significantly better postoperative DVA as compared with monofocal IOLs at speeds of 15, 30, 60, and 90 dps.
Multifocal IOLs have been developed and are used with the intention of increasing the depth of field at varying distances [10]. The AT LISA tri 839MP is a diffractive trifocal IOL that allocates 50% of the light to distance vision, 20% to intermediate, and 30% for near vision. To improve the quality of retinal processing, a slow transition area was designed to reduce disturbing light phenomena including glare and halo between the main zone and phase zones.
The present study demonstrated that implantation of the AT LISA tri 839MP provided better postoperative uncorrected near, intermediate, and distant VA compared with monofocal IOLs. The postoperative VA for trifocal IOL was similar to previous studies of the AT LISA tri 839MP [14, 15]. In addition, eyes in the trifocal IOL group showed better contrast sensitivity under photopic, mesopic, and photopic with glare conditions, at almost all spatial frequencies except for the spatial frequency of 18 cpd. Related to the mesopic with glare condition, the advantage of the trifocal IOL was observed in all assessed spatial frequencies, except 1.5 cpd. These contrast sensitivity results in the present study are consistent with some of the previous studies revealing that the photopic and mesopic contrast sensitivity were within the normal range following AT LISA tri 839MP implantation [16, 17]. And prospective cases demonstrated that no significant difference was found in low mesopic contrast sensitivity function between AT LISA tri 839MP group and monofocal group [18]. However, recently meta-analysis based on randomized clinical trials demonstrated that the contrast sensitivity following multifocal IOL implantation was significantly slightly lower than that of monofocal implantation, as multifocal IOL distributes light into different foci [19]. The disparity in the results might be due to IOL features and the patient enrollment including age [20]. Research showed that though the difference in contrast sensitivity between multifocal and monofocal was significant, multifocal IOLs of diffractive optics and aspheric profiles performed better and was similar to monofocal IOL in mesopic condition [21]. Thus, the superiority in contrast sensitivity in trifocal group might attribute to the design of AT LISA tri 839MP and better postoperative UDVA.
Dynamic vision plays an important role in performance of daily tasks. To our knowledge, presently, no standard DVA evaluation method has been widely accepted, although various DVA assessment systems have been developed [22,23,24,25]. There are two main methods of assessment to evaluate DVA. In one method, a static observer with their head secured fixes on the dynamic object (dynamic-object DVA). Alternatively, the static object is observed by the individual with their head permitted to move (static-object DVA). Dynamic-object DVA is more commonly applied except for when vestibular function is being assessed [26].
The present study utilized a self-developed dynamic-object DVA test system. DVA is influenced by the velocity, contrast, brightness, and motor pattern of the optotypes [27]. The test system applied in the present study projects optotypes of certain velocity and proper contrast in a bright environment. The optotypes were designed to be the same size, aligning with the optotypes on the ETDRS chart.
In the present study, trifocal IOL implantation demonstrated better DVA compared with monofocal IOLs. Optical factors may contribute to different DVA between groups. The correlation analysis in the present study demonstrated that DVA was positively associated with static VA, because retinal smear, defined as marginal artefacts of the retinal image, attribute to decreases in DVA [4]. Patients that received the trifocal IOL implant obtained better static VA compared with those that received the monofocal IOL in the present study. Thus, the retinal smear of patients receiving the monofocal IOLs may be more impactful than in the patients with the trifocal IOL, leading to worse DVA. However, conclusions related to the relationship between static VA and DVA have previously been controversial [23, 28, 29]. Primarily, static VA has been associated with DVA at mainly low speed, but not high speed [28], and in the present study, the DVA in eyes with a trifocal IOL was superior at both low and high speeds. This result may have been a consequence of variable mechanisms that contribute to the identification of objects at different speeds.
The completion of dynamic vision involves a complicated process including visual tracking, vestibular-ocular reflex, saccade and others, in order to maintain the position of the image on the retina, adjacent to the fovea to create clear vision [30,31,32]. In addition, DVA at different speeds is associated with different types of eye movements. The dynamic vision of low speed is mainly related to smoothing pursuit eye movement [33]. The tracking movement alone can maintain the target close to the fovea keeping consistently clear vision for low speed dynamic objects [34]. Thus, the better static VA obtained by a trifocal IOL may be predictive of better DVA.
For objects at high speed, an effective catch-up saccade strategy, compensating for the position error, is crucial in achieving better DVA [35, 36]. Better DVA is related to a minimum position error and low frequency of reverse saccades. Clear vision of objects is achieved when the position error is minimized during the negative acceleration phase of a catch-up saccade [33]. The primary advantage of the trifocal IOL is to provide improved near, intermediate, and distance VA, rather than only VA at a distance [11]. Previous research demonstrates that stable defocus curves are achieved following trifocal IOL implantation, meaning patients maintain continuous range of vision at different distances [37, 38]. The multiple linear regression in the present study demonstrated that intermediate visual acuity increasingly contributed to the dynamic vision as the speed increased, which revealed that better continuous range of vision at different distances is associated with better high speed dynamic vision. Thus, trifocal IOLs provide superior DVA over monofocal IOLs at both low and high speeds. Continuous range of vision likely provides patients with better predictive abilities of the position of dynamic objects and thus increases the accuracy of the catch-up saccade to avoid reverse saccade and detecting a step-ramp position error, effectively prompting the catch-up saccade.
In addition to static VA, DVA is crucial for patients to complete everyday tasks and is associated with quality of life in real-world circumstances [7]. Previous research, via questionnaires, have demonstrated that patients experience improved quality of life following trifocal IOL implant [16]. Development and application of DVA assessment contributes to a more comprehensive postoperative evaluation of patients, following cataract surgery. The main advantages of the present testing system are that it is easy to operate and master with testing procedures very similar to static VA with standardized optotypes. The test system developed and applied to the present study can also be used to evaluate DVA for patients receiving other ocular interventions such as keratoplasty, vitrectomy, and trabeculectomy to assess their ability to return to normal functioning and performance of daily tasks.
Limitations exist in the present study, which include the short duration of follow-up, of 3 months. Also, the analysis focused solely on the comparison of DVA between the groups, however, kinetic visual acuity also plays an important role in performance of tasks in daily life [39]. Improvements are planned for future iterations of the testing system to include different motor patterns for assessment. In addition, the present study was not randomized to IOL allocation and did not evaluate DVA preoperatively, thus lacking a comparative preoperative and postoperative assessment. Future studies are being planned that will include preoperative assessment and follow patient outcomes for a longer duration.
The present study demonstrated that implantation of diffractive trifocal IOLs provides better full range VA, contrast sensitivity and DVA at 15, 30, 60, 90 dps compared with monofocal IOLs. And intermediate visual acuity is increasingly associated with better DVA as the velocity increasing.
Summary
What was known before
-
Traditional cataract management has primarily focused on improving static visual acuity, however, rising patient expectations in the postoperative period have also increased the demand for enhanced vision, as an extension of quality of life relevant to improved DVA.
-
Our previous research has demonstrated greater loss in DVA for cataract patients and significant improvement of DVA following cataract surgery.
-
Trifocal intraocular lens provides with continuous range of vision compared with monofocal intraocular lens.
What this study adds
-
Diffractive trifocal intraocular lens provides better postoperative dynamic vision at low and high speeds compared with monofocal intraocular lens.
-
Intermediate visual acuity is increasingly associated with DVA as the velocity increasing.
Data availability
The raw data required to reproduce these findings are available upon requirements.
References
Lee CM, Afshari NA. The global state of cataract blindness. Curr Opin Ophthalmol. 2017;28:98–103.
Wang SY, Stem MS, Oren G, Shtein R, Lichter PR. Patient-centered and visual quality outcomes of premium cataract surgery: a systematic review. Eur J Ophthalmol. 2017;27:387–401.
Perez-Vives C. Biomaterial influence on intraocular lens performance: an overview. J Ophthalmol. 2018;2018:2687385.
Geer I, Robertson KM. Measurement of central and peripheral dynamic visual acuity thresholds during ocular pursuit of a moving target. Optom Vis Sci. 1993;70:552–60.
Hendry SH, Calkins DJ. Neuronal chemistry and functional organization in the primate visual system. Trends Neurosci. 1998;21:344–9.
Ishigaki H, Miyao M. Implications for dynamic visual acuity with changes in aged and sex. Percept Mot skills. 1994;78:363–9.
Patel I, Turano KA, Broman AT, Bandeen-Roche K, Munoz B, West SK. Measures of visual function and percentage of preferred walking speed in older adults: the salisbury eye evaluation project. Investig Ophthalmol Vis Sci. 2006;47:65–71.
Ao M, Li X, Huang C, Hou Z, Qiu W, Wang W. Significant improvement in dynamic visual acuity after cataract surgery: a promising potential parameter for functional vision. PloS ONE. 2014;9:e115812.
de Silva SR, Evans JR, Kirthi V, Ziaei M, Leyland M. Multifocal versus monofocal intraocular lenses after cataract extraction. Cochrane database Syst Rev. 2016;12:Cd003169.
Leyland M, Zinicola E. Multifocal versus monofocal intraocular lenses in cataract surgery: a systematic review. Ophthalmology. 2003;110:1789–98.
Mojzis P, Majerova K, Hrckova L, Pinero DP. Implantation of a diffractive trifocal intraocular lens: one-year follow-up. J cataract refractive Surg. 2015;41:1623–30.
Gatinel D, Pagnoulle C, Houbrechts Y, Gobin L. Design and qualification of a diffractive trifocal optical profile for intraocular lenses. J cataract refract Surg. 2011;37:2060–7.
Alfonso JF, Fernandez-Vega Cueto L, Belda-Salmeron L, Montes-Mico R, Fernandez-Vega L. Visual function after implantation of a diffractive aspheric trifocal intraocular lens. Eur J Ophthalmol. 2016;26:405–11.
Kretz FTA, Breyer D, Diakonis VF, Klabe K, Henke F, Auffarth GU et al. Clinical outcomes after binocular implantation of a new trifocal diffractive intraocular lens. J Ophthalmol. 2015;2015:962891.
Mendicute J, Kapp A, Lévy P, Krommes G, Arias-Puente A, Tomalla M et al. Evaluation of visual outcomes and patient satisfaction after implantation of a diffractive trifocal intraocular lens. J cataract refract Surg. 2016;42:203–10.
Alio JL, Kaymak H, Breyer D, Cochener B, Plaza-Puche AB. Quality of life related variables measured for three multifocal diffractive intraocular lenses: a prospective randomised clinical trial. Clin Exp Ophthalmol. 2018; 46:380–8
Mojzis P, Kukuckova L, Majerova K, Ziak P, Pinero DP. Postoperative visual performance with a bifocal and trifocal diffractive intraocular lens during a 1-year follow-up. Int J Ophthalmol. 2017;10:1528–33.
Plaza-Puche AB, Alio JL, Sala E, Mojzis P. Impact of low mesopic contrast sensitivity outcomes in different types of modern multifocal intraocular lenses. Eur J Ophthalmol. 2016;26:612–7.
Cao K, Friedman DS, Jin S, Yusufu M, Zhang J, Wang J et al. Multifocal versus monofocal intraocular lenses for age-related cataract patients: a system review and meta-analysis based on randomized controlled trials. Surv Ophthalmol. 2019;64:647–58
Schmitz S, Dick HB, Krummenauer F, Schwenn O, Krist R. Contrast sensitivity and glare disability by halogen light after monofocal and multifocal lens implantation. Br J Ophthalmol. 2000;84:1109–12.
Gil MA, Varon C, Cardona G, Vega F, Buil JA. Comparison of far and near contrast sensitivity in patients symmetrically implanted with multifocal and monofocal IOLs. Eur J Ophthalmol. 2014;24:44–52.
Hirano M, Hutchings N, Simpson T, Dalton K. Validity and repeatability of a novel dynamic visual acuity system. Optom Vis Sci. 2017;94:616–25.
Chang ST, Liu YH, Lee JS, See LC. Comparing sports vision among three groups of soft tennis adolescent athletes: normal vision, refractive errors with and without correction. Indian J Ophthalmol. 2015;63:716–21.
Vital D, Hegemann SC, Straumann D, Bergamin O, Bockisch CJ, Angehrn D et al. A new dynamic visual acuity test to assess peripheral vestibular function. Arch Otolaryngol Head Neck Surg. 2010;136:686–91.
Al-Awar Smither J, Kennedy RS. A portable device for the assessment of dynamic visual acuity. Appl ergonomics. 2010;41:266–73.
Ramat S, Colnaghi S, Boehler A, Astore S, Falco P, Mandala M et al. A device for the functional evaluation of the VOR in clinical settings. Front Neurol. 2012;3:39.
Hoffman LG, Rouse M, Ryan JB. Dynamic visual acuity: a review. J Am Optometric Assoc. 1981;52:883–7.
Weissman S, Freeburne CM. Relationship between static and dynamic visual activity. J Exp Psychol. 1965;70:141–6.
Fergenson PE, Suzansky JW. An investigation of dynamic and static visual acuity. Perception. 1973;2:343–56.
Hirsch J, Curcio CA. The spatial resolution capacity of human foveal retina. Vis Res. 1989;29:1095–101.
Demer JL, Crane BT, Tian JR, Wiest G. New tests of vestibular function. Ann N.Y. Acad Sci. 2001;942:428–45.
Hasegawa T, Yamashita M, Suzuki T, Hisa Y, Wada Y. Active linear head motion improves dynamic visual acuity in pursuing a high-speed moving object. Exp brain Res. 2009;194:505–16.
Palidis DJ, Wyder-Hodge PA, Fooken J, Spering M. Distinct eye movement patterns enhance dynamic visual acuity. PloS ONE. 2017;12:e0172061.
Uchida Y, Kudoh D, Murakami A, Honda M, Kitazawa S. Origins of superior dynamic visual acuity in baseball players: superior eye movements or superior image processing. PloS ONE. 2012;7:e31530.
de Brouwer S, Yuksel D, Blohm G, Missal M, Lefevre P. What triggers catch-up saccades during visual tracking? J Neurophysiol. 2002;87:1646–50.
Watson TL, Krekelberg B. The relationship between saccadic suppression and perceptual stability. Curr Biol: CB. 2009;19:1040–3.
Liu X, Xie L, Huang Y. Comparison of the visual performance after implantation of bifocal and trifocal intraocular lenses having an identical platform. J refract Surg. 2018;34:273–80.
Plaza-Puche AB, Alio JL. Analysis of defocus curves of different modern multifocal intraocular lenses. Eur J Ophthalmol. 2016;26:412–7.
Hoshina K, Tagami Y, Mimura O, Edagawa H, Matsubara M, Nakayama T. A study of static, kinetic, and dynamic visual acuity in 102 Japanese professional baseball players. Clin Ophthalmol. 2013;7:627–32.
Funding
This work was supported by a grant from Chinese Capital’s Funds for Health Improvement and Research (Grant number: CFH2018-2-4093).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Ren, X., Wang, Y., Wang, D. et al. A novel standardized test system to evaluate dynamic visual acuity post trifocal or monofocal intraocular lens implantation: a multicenter study. Eye 34, 2235–2241 (2020). https://doi.org/10.1038/s41433-020-0780-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-0780-9
This article is cited by
-
Comparison of dynamic defocus curve on cataract patients implanting extended depth of focus and monofocal intraocular lens
Eye and Vision (2023)
-
Developing dynamic defocus curve for evaluating dynamic vision accommodative function
BMC Ophthalmology (2022)
-
Comparisons of visual outcomes between bilateral implantation and mix-and-match implantation of three types intraocular lenses
International Ophthalmology (2022)
-
The Evaluation of a New IOL with Extended Depth of Focus to Increase Visual Acuity for Intermediate Distance
SN Comprehensive Clinical Medicine (2021)