Abstract
Purpose
Posterior fossa tumors (PFTs) are the most common type of brain tumor in children. Dysphagia is a known complication of PFT resection in children, but data regarding risk factors and clinical course are sparse.
Methods
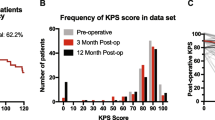
The records of all children who underwent resection of posterior fossa tumor between April 2007 and May 2017 at our institution were analyzed. Clinical, radiographic, histologic data were gathered. Swallowing function was assessed immediately postoperatively and at 1-year follow-up.
Results
A total of 197 patients were included. Forty-three (21.8%) patients developed dysphagia after surgery. Patients who developed dysphagia were younger (4.5 vs. 7.2 years, p < 0.01), were more likely to have brainstem compression (74.4% vs. 57.8%, p < 0.03) or invasion (14.0 vs. 9.7%, p < 0.03), and were more likely to have ependymoma (27.9% vs. 13.6%, p < 0.01) or ATRT (atypical teratoid/rhabdoid tumor) (9.3% vs. 3.9%, p < 0.01). Patients with postoperative dysphagia also had a longer length of stay (33.7 vs. 12.7 days, p < 0.01) and were more likely to be discharged to inpatient rehabilitation (25.6% vs. 9.1%, p < 0.01). Ten patients (5.1%) were PEG-dependent by 1-year follow-up. These patients were younger (2.7 vs. 5.6 years, p < 0.01), had a longer length of stay (55.5 vs. 27.4 days, p < 0.01), and were more likely to have ATRT (30.0% vs. 0.0%, p < 0.01). Recovery was not associated with tumor grade or extent of resection.
Conclusions
Dysphagia after PFT resection is associated with younger age, aggressive tumor histology, and increased healthcare utilization. While most patients recover, a small percentage are still dependent on enteral feeding at 1-year follow-up. Further research is needed to identify factors associated with persistent deficits.
Similar content being viewed by others
Abbreviations
- PFT:
-
posterior fossa tumor
- ATRT:
-
atypical teratoid/rhabdoid tumor
- PEG:
-
percutaneous endoscopic gastrostomy
- VFSS:
-
videofluoroscopic swallow study
- JPA:
-
juvenile pilocytic astrocytoma
- GTR:
-
gross total resection
- STR:
-
subtotal resection
References
Cornwell PL, Murdoch BE, Ward EC, Morgan A (2003) Dysarthria and dysphagia as long-term sequelae in a child treated for posterior fossa tumour. Pediatr Rehabil 6:67–75. https://doi.org/10.1080/1363849031000139289
Gustafsson B, Tibbling L (1991) Dysphagia, an unrecognized handicap. Dysphagia. 6:193–199
Hudgins RJ, Edwards MS (1987) Management of infratentorial brain tumors. Pediatr Neurosci 13:214–222
Kurien M, Andrews RE, Tattersall R, McAlindon ME, Wong EF, Johnston AJ, Hoeroldt B et al (2017) Gastrostomies preserve but do not increase quality of life for patients and caregivers. Clin Gastroenterol Hepatol 15:1047–1054. https://doi.org/10.1016/j.cgh.2016.10.032
Lee WH, Oh B-M, Seo HG, Kim SK, Phi JH, Chong S, Han TR (2016) One-year outcome of postoperative swallowing impairment in pediatric patients with posterior fossa brain tumor. J Neuro-Oncol 127:73–81. https://doi.org/10.1007/s11060-015-2010-z
Mei C, Morgan AT (2011) Incidence of mutism, dysarthria and dysphagia associated with childhood posterior fossa tumour. Childs Nerv Syst 27:1129–1136. https://doi.org/10.1007/s00381-011-1433-x
Morgan AT, Sell D, Ryan M, Raynsford E, Hayward R (2008) Pre and post-surgical dysphagia outcome associated with posterior fossa tumour in children. J Neuro-Oncol 87:347–354. https://doi.org/10.1007/s11060-008-9524-6
Morgan AT, Dodrill P, Ward EC (2012) Interventions for oropharyngeal dysphagia in children with neurological impairment. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD009456.pub2
Newman LA, Boop FA, Sanford RA, Thompson JW, Temple CK, Duntsch CD (2006) Postoperative swallowing function after posterior fossa tumor resection in pediatric patients. Childs Nerv Syst 22:1296–1300. https://doi.org/10.1007/s00381-006-0065-z
Rahnemai-Azar AA, Rahnemaiazar AA, Naghshizadian R, Kurtz A, Farkas DT (2014) Percutaneous endoscopic gastrostomy: indications, technique, complications and management. World J Gastroenterol 20:7739–7751. https://doi.org/10.3748/wjg.v20.i24.7739
Ram Z, Grossman R (2014) Dysphagia as a complication of posterior Fossa surgery in adults. World Neurosurg 82:625–626. https://doi.org/10.1016/j.wneu.2013.02.045
Rommel N, Hamdy S (2016) Oropharyngeal dysphagia: manifestations and diagnosis. Nat Rev Gastroenterol Hepatol 13:49–59. https://doi.org/10.1038/nrgastro.2015.199
Shem KL, Castillo K, Wong SL, Chang J, Kao M-C, Kolakowsky-Hayner SA (2012) Diagnostic accuracy of bedside swallow evaluation versus videofluoroscopy to assess dysphagia in individuals with tetraplegia. PM R 4:283–289. https://doi.org/10.1016/j.pmrj.2012.01.002
Snider CA, Yang K, Mack SC, Suh JH, Chao ST, Merchant TE, Murphy ES (2018) Impact of radiation therapy and extent of resection for ependymoma in young children: a population-based study. Pediatr Blood Cancer 65:e26880. https://doi.org/10.1002/pbc.26880
Spennato P, Nicosia G, Quaglietta L, Donofrio V, Mirone G, Di Martino G et al (2015) Posterior fossa tumors in infants and neonates. Childs Nerv Syst 31:1751–1772. https://doi.org/10.1007/s00381-015-2783-6
Steinbok P, Mangat JS, Kerr JM, Sargent M, Surianingtyas W, Singhal A, Cochrane D (2013) Neurological morbidity of surgical resection of pediatric cerebellar astrocytomas. Childs Nerv Syst 29:1269–1275. https://doi.org/10.1007/s00381-013-2171-z
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
IRB approval was obtained for this project.
Portions of this work were presented in poster form at the 2019 AANS Annual Scientific Meeting in San Diego, CA.
Conflict of interest
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Goethe, E.A., Gadgil, N., Stormes, K. et al. Predicting dysphagia in children undergoing surgery for posterior fossa tumors. Childs Nerv Syst 36, 925–931 (2020). https://doi.org/10.1007/s00381-019-04468-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-019-04468-7