Abstract
Cerebral venous thrombosis (CVT) is characterized by its variety of neurological manifestations and difficulty in diagnosis. In subacute cases, the main symptoms are secondary to increased intracranial pressure. This condition is associated with an extensive range of medical disorders, but only 2% are caused by a CNS infection in recent series. We report a 45-year-old patient, with no previous medical history, who developed a syndrome of increased intracranial pressure as the presentation of a cryptococcal meningoencephalitis (CM) complicated with a CVT. The patient was first diagnosed of a CVT, and later on, the VIH infection and the CM diagnosis were made. Despite being treated with anticoagulation, liposomal amphotericin B, and a therapeutic lumbar puncture, the patient continued to deteriorate and suffered a respiratory arrest secondary to the increased intracranial pressure, with subsequent brain death. Cryptococcus is an infrequent cause of CNS infection in developed countries, despite being the most frequent cause of meningits in adults in several countries with high rates of HIV infection. CVT is a very rare complication of CM which can contribute to worsen the increased intracranial pressure and in consequence, its prognosis and outcome. A high level of suspicion is needed for diagnosing CM as the underlying cause of CVT and the subsequent increased intracranial pressure should be managed exhaustively.
Similar content being viewed by others
Case report
A 45-year-old Moroccan woman, who had lived in Spain for the past years, and with no previous medical history, was initially assessed in the emergency room referring an intense headache and dizziness with nausea for 10 days. Physical examination only showed hyperpigmented papules on both legs (Fig. 1), and the neurological exam was unremarkable. Blood tests, chest radiography, and a non-enhanced brain-CT were normal, and the patient was discharged.
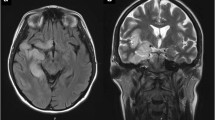
She returned to the emergency room 5 days later, due to increasing headache, diplopia, and confusion. Vital signs, including temperature, were normal. Examination showed a bilateral VI cranial nerve palsy and a decreased level of consciousness, raising the suspicion of a syndrome of increased intracranial pressure. Blood tests again were normal. A CT venography showed a partial thrombosis of the right transverse/sigmoid sinus (Fig. 2). A lumbar puncture was performed and a clear cerebrospinal fluid (CSF) was obtained, with 13 leukocytes/mm3 (84% of lymphocytes), 1700 red blood cells/mm3, 28.7 mg/dL of proteins, 46 mg/dL of glucose, and negative adenosine deaminase.
The patient was started on enoxaparin (1 mg/kg every 12 h), and in the next day, a positive blood serology for HIV was received. The thrombophilia and autoimmunity studies were normal. On the second day after admission, Cryptococcus neoformans was isolated on aerobic culture from CSF sample. With these results, treatment was switched to liposomal amphotericin B (4 mg/kg per day), and a therapeutic lumbar puncture was performed to decrease CSF pressure. However, despite an initial improvement, the patient continued to deteriorate during the next 2 days. Finally, she suffered a respiratory arrest secondary to the increased intracranial pressure, and she needed to be intubated, with subsequent brain death hours later.
Discussion
CM is an infrequent cause of meningoencephalitis in resource-rich settings and, if the patient is not suspected to be immunocompromised, it is not usually included as part of the initial differential diagnosis. However, CM is the most frequent cause of meningitis in adults in several countries with high rates of HIV infection (Williamson et al. 2017). The typical presentation includes fever and intense headache, but signs of increased intracranial pressure may also be present. Characteristic CSF parameters include elevated white cell count (with lymphocyte predominance), slightly elevated protein, and low glucose concentrations. In HIV-associated CM, white cell count is lower and can often be normal (Williamson et al. 2017). Recommended CSF diagnostic techniques include detection of cryptococcal antigen and aerobic culture (Williamson et al. 2017).
Treatment strategies for HIV-infected patients with CM include liposomal amphotericin-B (3–4 mg/kg per day intravenously) plus flucytosine (100 mg/kg per day orally) for at least 2 weeks (Perfect et al. 2010; Benson et al. 2018). Mortality is high even in resource-rich settings (15–26% at 10 weeks), and some of the factors that worsen the prognosis are the diagnostic delay, abnormal mental status, raised CSF pressure, and high CSF fungal burden (Williamson et al. 2017).
CVT is far less common than most other types of stroke, presenting with a remarkably wide spectrum of signs and symptoms that can make diagnosis difficult. The most frequent symptom is headache, which can be isolated or associated with other signs of increased intracranial pressure (Bousser and Ferro 2007). The main underlying causes nowadays are non-infectious, especially genetic and acquired thrombophilic disorders, pregnancy, puerperium, and oral contraceptives (Ferro et al. 2004). On the contrary, CNS infections only cause 2.1% of all cases in recent series and are associated with an unfavorable outcome (Ferro et al. 2004).
CVT can be an atypical complication of CM, with very few cases reported so far (Alejandra et al. 2014; Thiansukhon et al. 2014; Senadim et al. 2016). This is the first case report in a resource-rich setting like western Europe or USA. Two of the patients previously described were HIV seropositve, who developed CVT during the course of the CM (Alejandra et al. 2014; Thiansukhon et al. 2014). The first patient died and the second one improved gradually with anticoagulant and antifungal therapy. The last case was an immunocompetent patient, who was first diagnosed of CVT, with a CM diagnosis coming 1 week later after rapid deterioration of his mental status (Senadim et al. 2016).
Therefore, CVT is a rare complication of CM and, at the same time, CM is a very unusual cause of CVT. This fact can make a diagnostic really challenging, especially in subacute cases in which symptomatology is very unspecific. Our patient’s clinical presentation, consisting on a syndrome of increased intracranial pressure, could be easily attributed to the cerebral venous thrombosis, especially considering that she showed no infectious signs and that she was a young woman with no previous medical history. The main clues in the diagnostic approach of this patient, apart from being aware of the atypical and not well-known relationship between CM and CVT, are the HIV seropositivity, and the cutaneous lesions that she presented at the first examination. These molluscum contagiosum-like lesions are uncommon (10–20%) in CM, but they are considered as a marker of underlying disseminated disease and can sometimes precede the diagnosis of systemic infection (Hayashida et al. 2017; Baker and Reboli 1997). Nevertheless, the previous CM-CVT reported cases did not present these types of lesions.
As previously mentioned, diagnostic delay worsens the prognosis, as well as a high CSF pressure, which is usually attributed to blockage of the CSF reabsorption by cryptococcus at the level of the arachnoid granulations and other sites of CSF reabsorption (Williamson et al. 2017). Therefore, periodical therapeutic lumbar punctures are recommended to control high CSF pressure (Williamson et al. 2017; Perfect et al. 2010). In our patient, however, both the CM and the CVT might have contributed to the increased intracranial pressure and to the poor prognosis.
Our report contributes to recognize the relationship between CM and CVT, which is important to prevent a diagnosis delay of these life-threatening diseases. Additionally, this case report highlights the relevance of CVT in CM’s outcome, which should be taken into account when managing patients with this complication of the disease.
References
Alejandra GD, Carla TS, Laura MO (2014) Cerebral venous sinus thrombosis associated with cryptococcal meningitis in an HIV-positive patient. J Clin Case 4:421
Baker DJ, Reboli AC (1997) Cutaneous cryptococcosis. N Engl J Med 336:998
Benson C, Brooks J, Holmes K, Masur H, Pau A (2018) Panel on Opportunistic Infections in HIV-Infected Adults and Adolescents. Guidelines for the prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: recommendations from the Centers for Disease Control and Prevention, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. Available at http://aidsinfo.nih.gov/contentfiles/lvguidelines/adult_oi.pdf. Accessed 12/1/2018
Bousser MG, Ferro JM (2007) Cerebral venous thrombosis: an update. Lancet Neurol 6(2):162–170
Ferro JM, Canhão P, Stam J, Bousser MG, Barinagarrementeria F, ISCVT Investigators (2004) Prognosis of cerebral vein and dural sinus thrombosis: results of the International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVT). Stroke 35(3):664–670
Hayashida MZ, Seque CA, Pasin VP, Simões MM, Enokihara S, Porro AM (2017) Disseminated cryptococcosis with skin lesions: report of a case series. An Bras Dermatol 92(5 Suppl 1):69–72
Perfect JR, Dismukes WE, Dromer F, Goldman DL, Graybill JR, Hamill RJ, Harrison TS, Larsen RA, Lortholary O, Nguyen MH, Pappas PG, Powderly WG, Singh N, Sobel JD, Sorrell TC (2010) Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the Infectious Diseases Society of America. Clin Infect Dis 50(3):291–322
Senadim S, Alpaydin Baslo S, Tekin Güveli B, Dedei Daryan M, Kantaroglu E, Ozturk O, Atakli D (2016) A rare cause of cerebral venous thrombosis: cryptococcal meningoencephalitis. Neurol Sci 37(7):1145–1148
Thiansukhon E, Potigumjon A, Smitasin N (2014) Cerebral venous sinus thrombosis: a rare complication in cryptococcal meningitis. Int J Infect Dis 21:291
Williamson PR, Jarvis JN, Panackal AA et al (2017) Cryptococcal meningitis: epidemiology, immunology, diagnosis and therapy. Nat Rev Neurol 13(1):13–24
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Equiza, J., Fernandez-Eulate, G., Rodriguez-Antigüedad, J. et al. Cryptococcal meningoencephalitis presenting as cerebral venous thrombosis. J. Neurovirol. 26, 289–291 (2020). https://doi.org/10.1007/s13365-019-00813-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13365-019-00813-3