Abstract
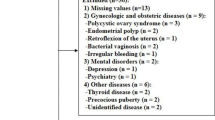
Daytime sleepiness is common in college students. In women, daytime sleepiness increases in the late-luteal phase compared with the follicular phase. In addition, women with premenstrual dysphoric disorder (PMDD), the severest form of premenstrual syndrome (PMS), experience severer daytime sleepiness than healthy women do. To date, daytime sleepiness has not been compared between women with PMDD and those with moderate PMS, or between men and women. Hence, this study aims to explore daytime sleepiness in college students in correlation with gender and the severity of premenstrual symptoms. We enrolled 658 Japanese college students (383 females, 275 males; age: 18–27 years) and assessed PMS and PMDD using the PMDD scale. Using the Japanese version of the Epworth Sleepiness Scale (JESS), we evaluated daytime sleepiness. Furthermore, women were asked about the severity of premenstrual daytime sleepiness. In this study, 47 (12.3%), 79 (20.6%), and 257 women (67.1%) were with PMDD, moderate-to-severe PMS (PMS), and no or mild PMS (no/mild PMS), respectively. The JESS score was markedly higher in women than that in men. The JESS score was highest in those with PMDD, followed by those with PMS, and lowest in those with no/mild PMS. Furthermore, women with no/mild PMS exhibited higher JESS score than men. This study suggests that daytime sleepiness is severer in women before menstruation than in men. Furthermore, the severity of daytime sleepiness in women correlates with the severity of premenstrual symptoms. Hence, daytime sleepiness should be cautioned in women with PMS/PMDD.

Similar content being viewed by others
References
American Academy of Sleep Medicine. International classification of sleep disorders. 3rd ed. Darien: American Academy of Sleep Medicine; 2014.
Steptoe A, Peacey V, Wardle J. Sleep duration and health in young adults. Arch Intern Med. 2006;166(16):1689–92.
Fukuda K, Ishihara K. Age-related changes of sleeping pattern during adolescence. Psychiatry Clin Neurosci. 2001;55(3):231–2.
Asaoka S, Fukuda K, Tsutsui Y, Yamazaki K. Does television viewing cause delayed and/or irregular sleep-wake patterns? Sleep Biol Rhythms. 2007;5(1):23–7.
Van den Bulck J. Television viewing, computer game playing, and Internet use and self-reported time to bed and time out of bed in secondary-school children. Sleep. 2004;27(1):101–4.
Asaoka S, Fukuda K, Yamazaki K. Effects of sleep–wake pattern and residential status on psychological distress in university students. Sleep Biol Rhythms. 2004;2(3):192–8.
Takamoto M, Komura K. Part-time jobs, mental health, and earning university credit. Jpn J Educ Psychol. 2018;66:14–27.
Wolfson AR, Carskadon MA. Understanding adolescents’ sleep patterns and school performance: a critical appraisal. Sleep Med Rev. 2003;7(6):491–506.
Rhie S, Lee S, Chae KY. Sleep patterns and school performance of Korean adolescents assessed using a Korean version of the pediatric daytime sleepiness scale. Korean J Pediatr. 2011;54(1):29–35.
Shibui K, Uchiyama M, Okawa M, Kudo Y, Kim K, Liu X, Kamei Y, Hayakawa T, Akamatsu T, Ohta K, et al. Diurnal fluctuation of sleep propensity and hormonal secretion across the menstrual cycle. Biol Psychiatry. 2000;48(11):1062–8.
Manber R, Bootzin RR. Sleep and the menstrual cycle. Health Psychol. 1997;16(3):209–14.
Merryman W, Boiman R, Barnes L, Rothchild I. Progesterone anesthesia in human subjects. J Clin Endocrinol Metab. 1954;14(12):1567–9.
Eisenhofer G, Peitzsch M, Kaden D, Langton K, Pamporaki C, Masjkur J, Tsatsaronis G, Mangelis A, Williams TA, Reincke M, et al. Reference intervals for plasma concentrations of adrenal steroids measured by LC–MS/MS: impact of gender, age, oral contraceptives, body mass index and blood pressure status. Clin Chim Acta. 2017;470:115–24.
Deutsch SI, Mastropaolo J, Hitri A. GABA-active steroids: endogenous modulators of GABA-gated chloride ion conductance. Clin Neuropharmacol. 1992;15(5):352–64.
Israel S, Schneller O. The thermogenic property of progesterone. Fertil Steril. 1950;1:53–65.
World Health Organization. Mental, behavioral and developmental disorders Tenth Revision of the International Classification of Diseases (ICD-10). Geneva: World Health Organization; 1996.
American Psychiatric Association: Diagnostic and statistical manual of mental disorders fifth edition (DSM-5) Arlington; 2013.
Baker FC, Colrain IM. Daytime sleepiness, psychomotor performance, waking EEG spectra and evoked potentials in women with severe premenstrual syndrome. J Sleep Res. 2010;19(1 Pt 2):214–27.
Lamarche LJ, Driver HS, Wiebe S, Crawford L. JM DEK: nocturnal sleep, daytime sleepiness, and napping among women with significant emotional/behavioral premenstrual symptoms. J Sleep Res. 2007;16(3):262–8.
Mauri M, Reid RL, MacLean AW. Sleep in the premenstrual phase: a self-report study of PMS patients and normal controls. Acta Psychiatr Scand. 1988;78(1):82–6.
Joo S, Shin C, Kim J, Yi H, Ahn Y, Park M, Kim J, Lee S. Prevalence and correlates of excessive daytime sleepiness in high school students in Korea. Psychiatry Clin Neurosci. 2005;59(4):433–40.
Liu Y, Zhang J, Li SX, Chan NY, Yu MWM, Lam SP, Chan JWY, Li AM, Wing YK. Excessive daytime sleepiness among children and adolescents: prevalence, correlates, and pubertal effects. Sleep Med. 2019;53:1–8.
Hara C, Lopes Rocha F, Lima-Costa MF. Prevalence of excessive daytime sleepiness and associated factors in a Brazilian community: the Bambui study. Sleep Med. 2004;5(1):31–6.
Gaina A, Sekine M, Hamanishi S, Chen X, Wang H, Yamagami T, Kagamimori S. Daytime sleepiness and associated factors in Japanese school children. J Pediatr. 2007;151(5):518–22 (522 e511–514).
Akerstedt T, Hallvig D, Kecklund G. Normative data on the diurnal pattern of the Karolinska Sleepiness Scale ratings and its relation to age, sex, work, stress, sleep quality and sickness absence/illness in a large sample of daytime workers. J Sleep Res. 2017;26(5):559–66.
Gau SF, Soong WT. Sleep problems of junior high school students in Taipei. Sleep. 1995;18(8):667–73.
Takegami M, Suzukamo Y, Wakita T, Noguchi H, Chin K, Kadotani H, Inoue Y, Oka Y, Nakamura T, Green J, et al. Development of a Japanese version of the Epworth Sleepiness Scale (JESS) based on item response theory. Sleep Med. 2009;10(5):556–65.
Miyaoka Y, Akimoto Y, Ueda K, Ujiie Y, Kametani M, Uchiide Y, Kamo T. Fulfillment of the premenstrual dysphoric disorder criteria confirmed using a self-rating questionnaire among Japanese women with depressive disorders. Biopsychosoc Med. 2011;5(1):5.
Steiner M, Macdougall M, Brown E. The premenstrual symptoms screening tool (PSST) for clinicians. Arch Womens Ment Health. 2003;6(3):203–9.
Yama K, Minami E, Machida M, Hayase N, Miura J. Relation between premenstrual syndrome, oxidative stress and depression. Pharmacometrics (Oyo Yakuri). 2018;95(1/2):19–24.
Johns M, Hocking B. Daytime sleepiness and sleep habits of Australian workers. Sleep. 1997;20(10):844–9.
Owens J. Adolescent Sleep Working G, Committee on A: insufficient sleep in adolescents and young adults: an update on causes and consequences. Pediatrics. 2014;134(3):e921–32.
Takeda T, Tasaka K, Sakata M, Murata Y. Prevalence of premenstrual syndrome and premenstrual dysphoric disorder in Japanese women. Arch Womens Ment Health. 2006;9(4):209–12.
Owashi T, Otsubo T, Tanaka K, Yoshida Y, Ishii Y, Koda R, Kobayashi R, Okajima Y, Kamijima K. Premenstrual dysphoric disorder in Japanese students of a nurse’s training schlool. Seishin Igaku (Clinical Psychiatry). 2001;43:1311–5.
Akimoto Y, Miyaoka Y, Kamo T. Clinical characteristics and stress coping behaviors in women with premenstrual syndrome or premenstrual dysphoric disorder. J Atomi Univ Fac Lit. 2009;43:45–60.
Acknowledgements
The authors thank all participants of this study for their time.
Author information
Authors and Affiliations
Contributions
JM conceptualized and designed the study, drafted the manuscript and the figure, and was responsible for the whole study. RH assisted with data acquisition and statistical analyses.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
This study protocol was approved by the Ethics Committee of Hokkaido Pharmaceutical University (No. 15-03-022) and was conducted per the ethical principles of the Declaration of Helsinki (Fortaleza, Brazil, 2013).
Research involving human participants
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Miura, J., Honma, R. Daytime sleepiness in relation to gender and premenstrual symptoms in a sample of Japanese college students. Sleep Biol. Rhythms 18, 3–8 (2020). https://doi.org/10.1007/s41105-019-00236-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41105-019-00236-x