Abstract
The International Collaboration on Cancer Reporting (ICCR) is a not for profit organisation whose goal is to produce standardised internationally agreed and evidence-based datasets for pathology reporting. With input from pathologists worldwide, the datasets are intended to be uniform and structured. They include all items necessary for an objective and accurate pathology report which enables clinicians to apply the best treatment for the patient. This dataset has had input from a multidisciplinary ICCR expert panel. The rationale for some items being required and others recommended is explained, based on the latest literature. The dataset incorporates data from the World Health Organization (WHO) 2016, and also from the latest (8th edition) TNM staging system of the American Joint Committee on Cancer (AJCC). Fifteen required elements and eight recommended items are described. This dataset provides all the details for a precise and valuable pathology report required for patient management and prognostication. This dataset is intended for worldwide use, and should facilitate the collection of standardised comparable data on bladder carcinoma at an international level.
Similar content being viewed by others
Introduction
Cancer treatment has become, over the years, more and more standardised. In order to treat patients the same way according to international standards and internationally adopted protocols, it is of critical importance that pathologists report the same items in a uniform way in their daily practice. The development of a single structured pathology report which can easily be applied worldwide is one of the major aims of this project. The approach of the ICCR has been accepted by genitourinary pathologists all over the world. With the input of an international group of expert pathologists, the approaches adopted in different organisations can be merged into one agreed upon dataset. In 2011, the College of American Pathologists (USA), The Royal College of Pathologists (UK), The Royal College of Pathologists of Australasia and the Canadian Association of Pathology (CAP-ACP) in association with the Canadian Partnership Against Cancer (CPAC) agreed to collaborate on the development of internationally agreed standards for pathology cancer reporting. The goal was to produce standards which could be integrated into national programs where they exist and to provide standards where none are available.
Following a successful pilot, the ICCR was incorporated as a not-for-profit organisation in 2014. Additional organisations including the American Society for Clinical Pathology, the European Society of Pathology and the Faculty of Pathology of the Royal College of Physicians of Ireland joined the group. To date, the ICCR has produced over 30 cancer reporting datasets which are made freely available from its website: www.iccr-cancer.org
All cancer reporting standards must align to the latest WHO Classification of Tumours and therefore the ICCR has aligned its development schedule with the update to the “bluebook” volumes. In 2015, the WHO commenced an update of the genitourinary chapters for the 4th edition of the bluebooks [1]. The ICCR initiated the development of a series of twelve datasets in synchrony with the production of the WHO Classification of Tumours of the Urinary System and Male Genital Organs which included four urinary tract datasets. This paper outlines the recommendations of the ICCR in regard to carcinoma of the urinary bladder in cystectomy, cystoprostatectomy and diverticulectomy specimens.
Methods
The purpose of the dataset was to make sure that a histopathology report includes all relevant information, and it was aimed to extend these recommendations internationally. The ICCR has developed standard operating procedures for the process of dataset development overseen by a Dataset Steering Committee (DSC), and these have been described in earlier publications (www.iccr-cancer.org/datasets). This dataset was developed through collaboration between the ICCR and the International Society of Urological Pathology (ISUP). The scope of this publication covers the pathology reporting of primary carcinoma of the urinary bladder in cystectomy, cystoprostatectomy and diverticulectomy specimens. This dataset does not include biopsies or transuretheral resection of the urinary bladder which are the subject of a separate dataset.
An expert panel (Data Authoring Committee [DAC]) was established with a designated Chair (Grignon D [USA]) and including several international expert uropathologists (Compérat E [Europe], Brimo F [Canada], Delahunt B [Australasia], Lopez-Beltran A [Europe], Reuter V [USA], Samaratunga H [Australasia], Shanks J [UK], Tsuzuki T [Japan], van der Kwast T [Canada], and Varma M [UK]) and a urologist (Koch M [USA]). Each DSC includes an ICCR representative (Srigley JR) and an ICCR Project Manager (Webster F) who are tasked with guiding and supporting the Chair in the development of the ICCR standards and to ensure quality assurance.
In keeping with all ICCR datasets, based on a comprehensive literature review and collected evidence, a set of elements were developed and categorised by the expert panel as either “required” or “recommended”. Required elements are considered to be mandatory and must be included as the minimum information in the pathology report. Required elements are those that the panel agreed were essential for diagnosis, prognostication and patient management. In general, these have evidentiary support at Level III-2 or above (based on prognostic factors in the National Health and Medical Research Council levels of evidence document, and defined as “Analysis of prognostic factors amongst persons in a single arm of a randomised controlled trial”). Elements lacking that level of evidence but considered critical in clinical practice could also be considered to be required. The “recommended” elements were defined as non-mandatory, which should ideally be included in the dataset, but were not yet validated or regularly used in patient management. Since the publication of the dataset, ICCR terminology has been modified to use the terms core and non-core rather than required and recommended; see http://www.iccr-cancer.org.
A commentary for each data item was provided on the basis of a review of the current literature, made by the project manager, who reviewed all cancer datasets and recommendations pertaining to primary urothelial carcinoma requiring bladder cystectomy, cystoprostatectomy or bladder diverticulectomy. This information was the basis of discussion among the experts. The experts were given time to go through the literature, and then a series of teleconferences to review and discuss each of the elements in the collated dataset were held.
A first draft was developed with the assistance of the Project Manager, presenting the proposed elements in order to follow the harmonisation of terminology guidelines and the included proposed responses. This draft was circulated to the expert panel for its comments. Points of agreement and disagreement were identified, and telephone conferences were held amongst the members of the expert panel to discuss each element. According to these discussions, modifications were made and, if necessary, an updated comment was added. The purpose of the commentary was to clarify the thought process and literature that supported the panel’s inclusion of individual elements as required or recommended. After reaching a general agreement by the DAC and after approval by the ICCR DSC, the dataset was posted to the ICCR website for a period of 2 months for public comment. After collecting all feedback, the dataset was once again reviewed and approved and final changes were made by the DAC. After the final approval by the DAC, the dataset was submitted to the ICCR DSC for ratification.
Results
The dataset has been developed for the reporting of cystectomy, cystoprostatectomy or diverticulectomy specimens from patients with carcinoma of the urinary bladder. The protocol applies to primary carcinomas (non-invasive and invasive), with or without associated epithelial lesions. Urothelial tumours diagnosed as papilloma or papillary urothelial neoplasm of low malignant potential are not carcinomas and this dataset does not apply to those diagnoses. Biopsy and transurethral resection specimens of the urinary bladder are dealt with in a separate dataset. The required elements in the dataset are listed in Table 1 and the recommended elements in Table 2.
Required dataset elements
Operative procedure
Documentation of the specific procedure performed should be a standard part of any pathology report. Knowledge of the procedure is crucial to the proper handling and reporting of a case. In some instances where there has been prior therapy (e.g. external beam radiation therapy for prostate cancer) or with large invasive tumours, the presence of certain tissues may not be readily apparent from the gross examination.
Additional specimens submitted
If any additional tissues are resected, documentation of these is a necessary part of the pathology report.
Maximum tumour dimension
The maximum tumour dimension is required (Table 1) with additional dimensions being recommended (Table 2). Some studies have demonstrated the maximum diameter of the residual tumour at the time of cystectomy as an independent predictor of recurrence and cancer-specific survival. In one report, residual tumour diameter ≥ 3 cm was an independent predictor of cancer-specific survival [2].
Macroscopic extent of invasion
For the staging of bladder cancer, documenting the gross extent of tumour invasion into the bladder wall is required (specifically for separation of pT3a from pT3b, which for these stages is a macroscopic classification). However, the distinction between tumour or fibrosis involving the perivesical fat can be challenging and requires microscopic confirmation to determine the tumour stage. Sites of prior transurethral resections of bladder tumours (TURBT) can appear as scars with a more or less prominent degree of fibrosis, depression and induration of the mucosa, especially when receiving the sample without fixation. After fixation, these gross aspects are less visible.
Prostatic involvement by tumour can occur by in situ involvement (essentially invisible on a gross examination) of the urethra and the prostatic ducts with or without associated invasion or by direct invasion by a bladder tumour that is invading through the bladder wall. For invasive carcinomas located towards the bladder neck region of the urinary bladder, submissions of sections to include the invasive tumour and the adjacent prostate gland are important; invasive tumours located on the posterior bladder wall can directly invade the seminal vesicles, and the gross evaluation should include evaluation of this area for accurate staging (pT4) [3].
If the tumour is located in the dome, the gross evaluation can be important to distinguish between urachal and bladder origin. The current WHO classification system includes urachal carcinoma as a separate category [1].
Histological tumour type
The 2016 WHO classification describes the different histological tumour types that should be reported [1]. As in the previous 2004 WHO Classification, a tumour is classified as a urothelial carcinoma if there is any identifiable urothelial component no matter how small, including the presence of urothelial carcinoma in situ (CIS) [1, 4]. For mixed tumours. the histological tumour type should be urothelial with the sub-type designated and the percentage provided. For example, a urothelial carcinoma with 80% squamous differentiation would be reported as urothelial carcinoma under histological tumour type and squamous under histological sub-type.
The only exception are cases with a neuroendocrine component (no matter whether small cell or large cell). The neuroendocrine tumour category includes 4 entities: small cell and large cell neuroendocrine carcinoma, which are distinct in respect of prognosis compared to the well-differentiated neuroendocrine tumours and paragangliomas, which will not be further discussed in this paper [1]. This remains a controversial area with conflicting approaches in the WHO publication and between the first and second print runs of the book. In the “invasive urothelial carcinoma” section, the recommendation is to report all cases with a neuroendocrine carcinoma component in the neuroendocrine tumour category. The neuroendocrine tumour section however recommended that mixed tumours be included in the neuroendocrine category only if the neuroendocrine carcinoma component constituted the majority of the tumour. In the second edition, the latter was changed to reflect the controversy in this area. The ICCR panel recommends following the recommendation in the invasive urothelial carcinoma section but also requires the percentage of the neuroendocrine carcinoma to be reported in all cases. From a practical standpoint, cases with a small cell neuroendocrine carcinoma component, irrespective of the amount are managed as small cell neuroendocrine carcinoma, even if there exists only a focal component of small cell carcinoma [5, 6].
Small cell neuroendocrine carcinoma is by far the most common among neuroendocrine tumours. About one-half of cases are pure, the others are mixed, mostly in association with classical urothelial carcinoma [1]. The National Comprehensive Cancer Network (NCCN) includes tumours with “any small-cell component” in the category of non-urothelial cell carcinoma [4, 7]. The diagnosis is defined by morphology and is supported by demonstration of neuroendocrine differentiation by immunohistochemistry with chromogranin A, synaptophysin and/or CD56. It should be noted that TTF-1 expression is present in approximately 50% of cases. If pure, direct spread from an adjacent organ or metastasis must be excluded clinically. Few data exist about large cell neuroendocrine carcinomas, but they should probably be treated the same [8].
Biopsies and TURBTs with pure adenocarcinoma or pure squamous cell carcinoma should be diagnosed as such, recognizing that definitive typing will only be possible after an evaluation of the entire tumour in the resection specimen. Urothelial carcinomas are heterogeneous lesions; therefore, the findings in the cystectomy specimen might differ from the initial TURBT report. In cases with pure squamous or glandular differentiation on biopsy/TURBT, the cystectomy may reveal a urothelial carcinoma with squamous or glandular differentiation. For this reason, a definitive diagnosis should be made with caution in biopsy or TURBT material.
For the first time, the 2016 WHO classification includes urachal carcinomas, arising from urachal remnants as a separate category [1]. It is generally not possible to diagnose urachal carcinoma in biopsy and TURBT material based on the morphologic findings alone. Criteria for the diagnosis of urachal carcinoma include location in the bladder dome or anterior wall with an epicentre in the bladder wall or perivesical tissue. The absence of diffuse cystitis glandularis/intestinal metaplasia outside of the dome/anterior wall region and the absence of a known primary elsewhere are also in favour of this diagnosis. Over 80% of urachal carcinomas are adenocarcinomas (mucinous, solid or cystic, rarely enteric or signet ring-cell), followed by urothelial carcinoma, squamous cell carcinoma and small cell neuroendocrine carcinoma. If a diagnosis of urachal carcinoma is rendered, the histologic type, like in other bladder carcinomas, should be specified. No reliable immunohistochemical markers exist in order to distinguish adenocarcinomas of the urachus from primary adenocarcinomas of the bladder proper or from secondary adenocarcinomas [9,10,11]. Gross examination and imaging are probably the most important parameters for this distinction.
Another new category in the 2016 WHO classification is the very rare Müllerian tumours [1]. These consist primarily of clear cell carcinoma and rarely of endometrioid carcinoma, which are morphologically the same as their counterparts in the female genital tract. If clear cell carcinoma presents as a bladder tumour in a female, it more likely represents secondary involvement of a primary arising in a urethral diverticulum [12]. Clear cell carcinoma and endometrioid carcinoma may arise from endometriosis or rarely from Müllerianosis [13]. Clear cell carcinoma must also be distinguished from urothelial carcinoma with divergent differentiation along Müllerian lines [14]. An important diagnostic criterion is the negativity of urothelial markers such as p63, GATA3 and high molecular weight cytokeratin [15, 16]. Müllerian type clear cell carcinoma has a similar immunohistochemical profile to primary tumours of the female genital tract, and so immunohistochemistry cannot be used to distinguish a primary from a secondary origin [17, 18].
Lastly, there are carcinomas arising in the urinary bladder without any specific differentiation, and if metastasis can be excluded, the carcinoma is considered to be primary in the urinary tract. Given that there is no evidence of urothelial differentiation, these should be reported using the “carcinoma, type cannot be determined” category [1].
Histologic subtype/variant
Numerous morphologic variations of urothelial carcinoma have been described with many of these included in the WHO 2016 classification as specific subtypes. Three main morphologic categories can be distinguished: variants that have a deceptively bland morphology, such as the nested variant, which can be misdiagnosed as von Brunn’s hyperplasia, if not invading the muscularis propria/detrusor muscle. Even if the nuclear cytomorphology appears relatively bland, these carcinomas behave like high-grade carcinomas. The second category contains tumours that have a morphology mimicking other tumours, for example the micropapillary carcinoma, especially in a metastatic setting (e.g. metastases from another micropapillary carcinoma from the ovary/peritoneum or more rarely gastrointestinal tract). Lastly are those tumour variants that have important prognostic or therapeutic implications such as the plasmacytoid/diffuse or sarcomatoid variants. The level of evidence for specific variants having independent prognostic information varies [19,20,21]. Rather than requiring reporting of variant histology, including the percentage of the variant component for selected variants only, it is recommended that this be done for all variants.
Variant histology has been receiving increasing attention in clinical management decisions since it has been clear that some variants have different prognosis and treatment implications [22, 23]. Some variants are highlighted because of the high frequency of understaging when present in biopsy or TURBT specimens, as discussed in the ICCR Urinary tract carcinoma—biopsy and transurethral resection specimen dataset [24]. There are an increasing number of therapeutic algorithms that incorporate variant histology as a significant factor [25]. Some authors even raise the question of an upfront cystectomy in some cases with variant histology, such as the micropapillary carcinoma cT1N0M0 [7, 26, 27]. The responsibility of the pathologist to recognize and document variant histology in this setting is obvious.
Reporting the percentage of variant histology is recommended, providing clinicians the ability to treat patients according to the latest results of the literature. If more than one variant is present, it is recommended that the percentage of each be documented. Supporting data regarding the significance of the percentage of a given variant is limited and available for only a few such as the micropapillary, sarcomatoid, lymphoepithelioma-like and carcinomas with divergent differentiation (glandular, squamous). Even for these, the data is limited and not robust with well-defined cut points not yet available. Nonetheless, utilizing this information in clinical decision making is recommended in some clinical guidelines. The 2016 WHO classification of tumours of the urothelial tract is provided in Table 3 [1].
Non-invasive carcinoma
The majority of cystectomies are performed for invasive pT1–4 carcinomas. However, according to published clinical guidelines, other indications exist: e.g. patients with urothelial CIS that fail intra-vesical therapy, or for high-grade non-invasive papillary carcinomas that are refractory to BCG or recur after completion of BCG maintenance [28]. Furthermore, BCG intolerance may also be an indication for cystectomy. In cases of large and extensive non-resectable (by TURBT) non-invasive papillary tumours, cystectomy can also become necessary.
For patients undergoing cystectomy for invasive carcinoma, it may be important to document the presence of non-invasive carcinoma. Large cystectomy series have reported concomitant carcinoma in situ in 19 to 54% of cases with most series at the higher end of this range. The data are contradictory as to whether the presence of concomitant CIS has an impact on an increased risk of recurrence elsewhere in the urinary tract or on cancer-specific survival [29]. Prostatic involvement by in situ carcinoma has been shown to be a major risk factor of urethral recurrence in men [30].
Histological tumour grade
Histologic grading of urothelial tumours is best considered in two categories: non-invasive papillary tumours and invasive carcinoma. For non-invasive papillary tumours, the 2016 WHO remains the same as in the 2004 WHO and continues to recommend the grading system first put forward by the ISUP in 1997 [31]. In this grading system, carcinomas are either low or high grade [31, 32]. The system is now recommended by almost all major pathology and urology organisations as the preferred grading system [7, 30, 31]. With this system, more high-grade tumours are reported; however, it must be remembered that a substantial proportion of what were formerly considered low-grade carcinomas are now placed in the papillary urothelial neoplasm of low malignant potential category.
The WHO 2016 considers the category of “papillary urothelial neoplasm of low malignant potential” to represent a tumour without the capacity to invade or metastasise. These can however “recur” but patients with this as their initial diagnosis will rarely develop a high-grade or invasive carcinoma [1, 33]. Papillary urothelial neoplasm of low malignant potential is not reported using this dataset.
Grade heterogeneity, is quite common in papillary urothelial carcinoma, and has been reported in up to 32% of cases [34]. It is currently recommended that the tumour grade be assigned based on the highest grade present. Some authors have recommended considering a tumour low grade if the high-grade component accounts for less than 5% of the tumour volume [33]. In one study, tumours with less than 10% of high-grade histology (5% of the cases) were compared with low- and high-grade tumours. The progression-free and cancer-specific survival of the mixed cases was similar to low-grade tumours and significantly better than that of high-grade cases [35]. The limited data does not however allow for a definitive statement regarding reporting of cases with a small volume of high-grade tumour or to determine what percentage of high-grade tumour is necessary to indicate a significantly worse prognosis. Another recent paper with a small number of cases showed that grade heterogeneity in urothelial carcinoma is characterized by increased MIB-1 labelling, in the low-grade areas as well as the high-grade component. Further, the investigators found that in FGFR3 mutant carcinoma, homozygous deletions of CDKN2A in both low- and high-grade areas, suggesting that CDKN2A deletion occurs prior to grade progression. This study supports the current convention to assign the highest grade to urothelial carcinomas with grade heterogeneity [36].
The International Consultation on Urologic Disease considered that a reasonable approach for tumours with grade heterogeneity would be to assign grade based on the highest grade present, and in those cases where the high-grade component is less than 10%, this observation should be communicated to the clinician in the pathology report [34]. The 2016 WHO recommends grading based on the highest grade component acknowledging the uncertainty of how to approach cases with a small proportion of high-grade tumour. It does indicate that “it may be prudent to state the proportion of high-grade disease”. [1] The ICCR recommends reporting cases where the high-grade component is less than 10% as high grade but including this information in the pathology report.
The 1973 WHO grading system for non-muscle invasive tumours remains in use in some regions, and some published guidelines recommend the reporting of both the current WHO grade with the 1973 grade [37], while others provide for the 1973 grade to be included by institutional choice [30]. It is beyond the scope of this commentary to provide a detailed argument for or against the 1973 WHO. Interested readers can review those discussions elsewhere [37]. The ICCR dataset follows WHO 2016 [1] with reporting of the WHO 2016 grade as a required element and the inclusion of other grading systems as optional.
The grading of invasive urothelial carcinoma is another area of controversy. In North America, the vast majority of invasive urothelial carcinomas have been diagnosed as high grade in contrast to European studies where a substantial percentage of invasive tumours has been graded as WHO 1973 grade 2 or even grade 1. Currently, there is general agreement that grade 1 tumours do not invade and this grade should not be assigned [38,39,40]. Some cases reported as grade 2 invasive tumours correspond to histological variants, such as the nested carcinoma that, as already described, has bland features but is nevertheless an aggressive carcinoma. It is questionable if variants should be graded, as studies show that patients with variant histologies have poorer outcome [41, 42]. In studies using the 1998 ISUP/WHO 2004 grading system, the vast majority of invasive tumours are high grade [41]. The conclusion of the International Consultation on Urologic Disease pathology group was that all invasive carcinomas should be considered high grade. We recommend the 2016 WHO approach of continuing to grade invasive carcinoma using the WHO 2004 system recognising that the vast majority of tumours will be high grade [1, 43]. If invasive tumours are graded using an alternative grading system, this should be indicated.
Microscopic extent of invasion
Determining the extent of invasion is the key feature for assigning the pathologic stage (pT) [44]. In most cases, this is relatively straightforward, but a few situations can be present challenges. There are several publications providing guidelines for the optimal gross examination and sampling of radical cystectomy specimens, and those will not be repeated here [44, 45].
In contemporary cystectomy series, 5 to 20% of specimens do not display any residual tumour [44, 46]. The increasing use of neoadjuvant chemotherapy and the performance of radical cystectomy for cT1 disease will contribute to the number of pT0 cases increasing in the future. When evaluating for residual disease, it is crucial to find the site of the prior TURBT. If grossly evident, this area can be completely submitted for microscopic examination (or if large extensively sampled). If no grossly apparent lesion exists, the clinical information, including location and pathologic findings from a previous resection, may be helpful. Sampling of areas with mucosal lesions such as erythema may identify foci of carcinoma in situ, and the same is true for random samples of apparently normal mucosa, although less frequently. If the prior TURBT site is identified microscopically and no cancer is found, the case can be reported as “no residual tumour” (pT0) without resorting to extensive sampling of grossly normal bladder tissue.
Determination of peri-vesical fat invasion would seem to be relatively straight forward, but the junction between the outer layer of the muscularis propria and the perivesical fat is poorly defined. The deep aspect of the muscularis propria typically results in haphazardly separated muscle bundles forming a poorly defined demarcation, and there is inconsistency, even among experts in defining peri-vesical fat extension [47]. This variability may explain the contradictory prognostic differences between pT2b and pT3a tumours in different reports [48, 49]. Distinction of pT3a from pT3b tumours has consistently been found to be prognostically significant. Desmoplastic reaction and fibrosis around an invasive carcinoma invading the perivesical fat is frequently observed and can be also problematic for staging. Tumour within desmoplastic tissue but not touching fat should still be assigned to the pT3 category if beyond the muscularis propria. Further, tumours described as grossly involving the perivesical fat require histologic confirmation before assigning a pT3b category.
Invasion into adjacent structures represents pT4 disease and is important to document. Involvement of the prostate gland represents a unique group in that the invasion can occur by different routes: direct invasion by the invasive tumour from the bladder or invasion by from situ disease involving the prostatic urethra and/or prostatic ducts (see “Pathological staging” section for detailed discussion) [3].
Less than 2% of bladder carcinomas arise in diverticula. For unknown reasons, the urothelium in diverticula has a significantly higher risk for developing a carcinoma than in the urinary bladder. This may relate to chronic inflammation or irritation of the mucosa though that is speculative. Most carcinomas in diverticula are urothelial, but other histologic types such as squamous cell carcinoma can occur [50, 51]. The majority of bladder diverticula are acquired (no muscularis propria); therefore, pT2 category cannot be assigned resulting in invasive tumours being placed in pT1 or pT3 only [1, 25, 52]. Acquired diverticula usually have fibres of the muscularis mucosae present, and these can be hypertrophic and should not be confused with muscularis propria. Diverticular carcinomas are treated by diverticulectomy, partial cystectomy or radical cystectomy.
Lymphovascular invasion
The data on lymphovascular invasion (LVI) in urothelial carcinoma of the urinary bladder is abundant, and it has repeatedly been shown to be a poor prognosticator in pT1–4 carcinomas [1]. Large multi-institutional series, cases from phase 3 clinical trials and prognostic scores, have found LVI to be a highly significant independent predictor of outcome [30, 53, 54]. This is therefore a required element. Immunohistochemistry can be useful in confirming its presence, but is not considered to be necessary.
Margin status
Evaluation of surgical margin status is a major component of the evaluation of resection specimens in most areas of surgical oncology [55]. Gross evaluation of the surgical margins is important to ensure that tissue sections are taken at the locations that are most likely to have involvement confirmed histologically. For cases where the gross examination suggests a positive surgical margin, margins should be inked. If histology does not confirm the gross impression, additional sections in this region may be appropriate. Confirmation by microscopic examination is necessary as the stromal response to invasive tumour or a prior TURBT may mimic a positive margin.
Studies have reported positive surgical margins to be present in 4 to 15% of radical cystectomy specimens [55, 56]. They generally fall into three categories: urethral, ureteral and soft tissue. Urethral and ureteral margins can be involved by in situ carcinoma and/or invasive carcinoma. Evaluation can be done intra-operatively by frozen section. Margins that are most frequently positive are the soft tissues followed by the urethra and then the ureters (recognizing that the latter are often controlled with intra-operative frozen sections).
Positive soft tissue surgical margins are an independent predictors of an increased risk of recurrence and decreased cancer-specific survival [57]. A French multi-institutional case control study showed a significantly higher recurrence rate and decreased cancer-specific survival for patients with positive urethral and soft tissue surgical margins but not for ureteral margins [55]. In the multivariable analysis, both urethral and soft tissue margins remained significant for recurrence with only soft tissue margins being significant for cancer-specific survival.
Frozen sections are commonly performed for margin control of the ureters at the time of cystectomy. Frozen section interpretation is reliable with low false positive or false negative rates. Involvement of the margin by carcinoma in situ is observed in up to 9% of cases [58]. The utility of routine frozen sections is however controversial [55, 59]. “Skip lesions” can be present in up to 4.8% of patients, as urothelial carcinoma has to be considered as a multifocal disease [59]. The European Association of Urology (EAU) guidelines do not currently recommend the routine use of frozen sections [25]. Overall recurrence in the ureter occurs in up to 13% of patients following cystectomy and with recurrence of invasive carcinoma at the uretero-ileal anastomosis in less than 1% [60]. Recurrence is significantly higher in patients with documented ureteric involvement, especially in men [61]. This increased risk is reduced if a negative margin is subsequently obtained with frozen section control or a prior negative biopsy [62, 63].
Frozen sections for control of the urethral margin are performed less frequently. In general, they are most often performed when an orthotopic diversion is planned and/or when there has been documentation of prostatic urethral involvement prior to the resection procedure. A positive urethral margin is associated with an increased risk of recurrence in the urethra.
Pathological staging
Pathologic stage remains the single most important prognostic parameter in patients treated by radical cystectomy. Many issues related to staging have already been addressed in the section on extent of invasion and will not be repeated here.
An important issue that has been controversial but has been clarified in the 8th edition of the AJCC Cancer Staging Manual [64] is the assignment of pathologic stage in cases with involvement of the prostatic urethra and the prostate gland in cystoprostatectomy specimens. In contemporary cystoprostatectomy series, involvement of the prostatic urethra with or without prostate gland involvement is a frequent finding being reported in 16 to 48% of cases [65, 66].
Some authors have reported that prostatic gland involvement in such cases could be classified as contiguous or non-contiguous with the latter having a significantly better prognosis [67]. The prostatic stroma can be invaded by different mechanisms. The first is direct (transmural) extension of the invasive bladder cancer into the prostatic stroma. A second is a tumour which invades via the bladder wall and the perivesical fat into the outer part of the prostate gland [3]. A third mechanism would be extension of urothelial carcinoma in situ into the prostatic urethra and/or prostatic ducts with subsequent prostatic stromal invasion. There are data that indicate significant prognostic differences between these groups, with the extension via the perivesical fat having a substantially worse prognosis [68]. It is therefore important to determine the mechanism of involvement.
The current TNM (AJCC) has clarified the handling of prostatic involvement [64] .For cases with direct extension of the invasive tumour into the prostate gland, the pT4a category is assigned. In cases of invasion of the prostatic stroma from tumour in the urethra or prostatic ducts, the pT category is assigned using the urethral carcinoma staging system. If the tumour invades from the urethral mucosa into the subepithelial connective tissue but not into the prostatic stroma, it is placed in the pT1 category. For cases with prostatic stromal involvement (from the urethra or prostatic ducts), it is assigned pT2, and if there is invasion of the periprostatic soft tissue pT3.
Regional lymph node status
A regional lymph node dissection is a standard part of radical cystectomy or cystoprostatectomy procedures. Most features relating to regional lymph node status are required items (Table 1), but some are recommended (Table 2).
The optimal surgical extent of the lymph node dissection has not been determined and remains a topic under discussion in the urologic oncology community. Contrary to the situation with other organs, no minimal lymph node number is universally accepted to define an “acceptable” lymph node sampling. Several studies have demonstrated that the number of lymph nodes resected and the number of positive lymph nodes are independent prognostic indicators. The distinction of pN1 from pN2 is based on the number of positive lymph nodes (1 or greater than 1). There is also strong data indicating that the proportion of positive lymph nodes (lymph node density) is also prognostically significant. For these reasons, accurate assessment of the number of lymph nodes sampled and the number with metastases is important and has required elements.
Extranodal extension of a lymph node metastasis appears to be associated with worse cancer-specific survival but there is limited data in the literature and for that reason, this element is in the recommended group. In a multi-institutional study of 748 cases with positive lymph nodes, extranodal extension was present in 50% and was the most significant independent predictor of disease recurrence and cancer-specific mortality [69, 70].
Histologically confirmed distant metastases
In some patients, there will be known metastases that have been confirmed histologically. This should be included in the pathology report with the relevant pathology identifier if available.
In the 8th edition of the AJCC TNM staging manual, the M category has been revised [64]. pM1 is now subdivided into pM1a for distant metastases limited to lymph nodes beyond the common iliac nodes and pM1b for non-lymph node metastases [64, 71].
Recommended dataset elements
Those elements which are not a required component of a pathology report, but provide important information that relates to diagnosis, treatment and/or prognostic assessment, are classified as recommended elements and are listed in Table 2.
Clinical information
Relevant history is critical in the accurate diagnosis of tumours in any location, including the urinary tract [27]. This may be relevant to the specific diagnosis of the case. Given that the provision of clinical information is largely the responsibility of the clinician, it is listed as a recommended rather than required element. This information can have an impact on the diagnostic process or affect its interpretation. Urothelial carcinoma is a multifocal disease, and therefore the entire urinary tract can be affected. Morphologic changes occur with the potential for misdiagnosis if the pathologist is unaware of a prior treatment such as Bacillus Calmette-Guerine (BCG), radiation therapy or neoadjuvant chemotherapy [34]. A prior transurethral resection can result in a pronounced myofibroblastic proliferation that can be misinterpreted as being sarcomatoid carcinoma. Radiation therapy (to the bladder or to an adjacent organ) can be associated with a pseudocarcinomatous hyperplasia that can be misinterpreted as invasive carcinoma.
Tumour focality
Urothelial carcinoma of the urinary bladder is often present as a multifocal disease. Recent studies have shown that multifocal tumours might have different clonal origins [67]. Multifocality of invasive urothelial carcinoma is part of the SPARC (Survival Prediction After Radical Cystectomy) score, a prediction model for bladder cancer-specific survival after radical cystectomy. This model includes also other items like tumour stage, nodal status and lymphovascular invasion [72]. There are inconsistent data to suggest that the multifocality in the urinary bladder increases the risk of the later development of urothelial carcinoma in the upper tracts and urethra [73,74,75].
Macroscopic tumour site
Tumour location is important for several reasons. Location in the dome or anterior wall requires consideration of a possible urachal origin. In cases with secondary involvement of the urinary bladder, common sites of direct extension from adjacent organs include the prostate gland, cervix and lower uterine segment. Colorectal adenocarcinoma is also a consideration for adenocarcinoma. Depending on the histological features, these possibilities should be considered when the tumour involves the posterior wall and bladder neck region. This is also relevant for staging as tumours in this region may directly invade adjacent structures such as the prostate gland in men and the vagina/cervix/uterus in women.
Block identification key
The origin/designation of all tissue blocks must be recorded and documented in the final pathology report in all cases. This is particularly important in cases undergoing internal or external review. If this information is not included in the final pathology report, it must be available on the laboratory computer system and relayed to the reviewing pathologist. The designation of tissue blocks is also crucial for further immunohistochemical or molecular analysis, research studies or clinical trials. Although block identification is not a required element in the dataset, we do consider it a required element in the surgical pathology report (most often located within the gross description).
Associated epithelial lesions
Many neoplastic lesions other than urothelial carcinoma are recognised in the urinary tract. These include papillary lesions such as urothelial papilloma, papillary urothelial neoplasm of low malignant potential and inverted urothelial papilloma. There can also be flat lesions such as urothelial dysplasia, keratinizing squamous metaplasia with or without dysplasia and intestinal metaplasia with or without dysplasia. Their identification may have diagnostic and prognostic implications (e.g. the presence of keratinizing squamous metaplasia with dysplasia supporting the diagnosis of primary squamous cell carcinoma). Reporting these items is a question of completeness of the pathology report but is not considered to be required.
Response to preoperative therapy
Neoadjuvant chemotherapy is recommended as a part of the management of patients with high-risk bladder cancer prior to cystectomy [25]. In the EAU guidelines, neoadjuvant chemotherapy is a grade “A” recommendation for cT2-T4a cN0 M0 bladder cancer and should always be a cisplatinum-based combination therapy [25]. After cystectomy, patients receiving neoadjuvant chemotherapy are often down staged and may be pT0, which is associated with improved survival; the same has been shown for ypT0 at cystectomy after TURBT. Variant histology does not seem to impact these results [76, 77].
There is little data on what, if any, morphologic alterations in the tumour can be related to the chemotherapy agents nor if any possible changes are related to outcome. The term “tumour regression grade” has appeared in the literature, but this refers to the volume of residual disease relative to the size of the TURBT scar rather than a morphologic alteration in the tumour itself [78].
Coexistent pathology
Several non-neoplastic changes can be found in radical cystectomy specimens. For the urinary bladder, findings such as keratinizing squamous metaplasia and intestinal metaplasia may be relevant in cases of squamous cell carcinoma and adenocarcinoma but reporting is neither critical nor required. Other findings such as nephrogenic adenoma, inflammation (including BCG-related granulomas) and changes related to prior biopsy or TURBT procedures are often present. Once again, reporting these when present is essentially a question of completeness of the surgical pathology report.
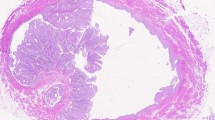
Significant pathology in other organs removed at the time of radical cystectomy can also be recognised. Perhaps most common is the incidental finding of prostate adenocarcinoma in cystoprostatectomy specimens. This has been reported in 25 to 38% of cystoprostatectomies [79, 80]. When this occurs, the prostatectomy dataset should be inserted in the pathology report and completed as appropriate (Fig. 10).
Ancillary studies
Currently, there are no ancillary studies recommended for routine use in urothelial carcinoma; immunohistochemistry, if used diagnostically, should be reported in this section.
Conclusion
The current recommended reporting dataset for cystectomy/cystoprostatectomy/diverticulectomy specimens looks exhaustive at first sight, but contains only the minimum requirements for a complete standardised pathology report. This report also asks for some collaboration from the clinician. Without clinical information, the pathologist will not be able to produce a complete and accurate report to support optimal patent management. Required elements reflect those elements that have strong supporting published data and/or are vital to patient management. Inclusion of recommended elements as well will result in a comprehensive and complete assessment of the resection specimen.
This dataset has been developed in conjunction with recent ISUP-based articles on the detailed macroscopic and microscopic assessments, the WHO classification of tumours and the 8th edition of the AJCC cancer staging manual. Published clinical guidelines, in particular those developed by the EAU, are referenced throughout. The development of these datasets by the ICCR in collaboration with multiple pathology organizations is intended to improve uniformity in the reporting of carcinomas arising in the urinary bladder. This will help in patient management and allow further studies to investigate the prognostic and clinical importance of the elements described at an international level.
Data availability
All ICCR datasets are freely available for worldwide use at the following website: http://www.iccr-cancer.org/datasets.
References
World Health Organization (2016) In: Moch H, Humphrey P, Ulbright T, Reuter R (eds) WHO classification of umours of the urinary system and male genital organs. IARC Press, Lyon, France
Soave A, John LM, Dahlem R, Minner S, Engel O, Schmidt S, Kluth LA, Fisch M, Rink M (2015) The impact of tumor diameter and tumor necrosis on oncologic outcomes in patients with urothelial carcinoma of the bladder treated with radical cystectomy. Urology 86(1):92–98
Donat SM, Genega EM, Herr HW, Reuter VE (2001) Mechanisms of prostatic stromal invasion in patients with bladder cancer: clinical significance. J Urol 165(4):1117–1120
Clark PE, Agarwal N, Biagioli MC, Eisenberger MA, Greenberg RE, Herr HW, Inman BA, Kuban DA, Kuzel TM, Lele SM, Michalski J, Pagliaro LC, Pal SK, Patterson A, Plimack ER, Pohar KS, Porter MP, Richie JP, Sexton WJ, Shipley WU, Small EJ, Spiess PE, Trump DL, Wile G, Wilson TG, Dwyer M, Ho M, National Comprehensive Cancer Network (NCCN) (2013) Bladder cancer. J Natl Compr Cancer Netw 11(4):446–475
Alanee S, Alvarado-Cabrero I, Murugan P, Kumar R, Nepple KG, Paner GP, Patel MI, Raspollini MR, Lopez-Beltran A, Konety BR (2019) Update of the international consultation on urological diseases on bladder cancer 2018: non-urothelial cancers of the urinary bladder. World J Urol 37(1):107–114
Warrick JI, Sjodahl G, Kaag M, Raman JD, Merrill S, Shuman L et al (2019) Intratumoral heterogeneity of bladder cancer by molecular subtypes and histologic variants. Eur Urol 75(1):18–22
Amin MB, Smith SC, Reuter VE, Epstein JI, Grignon DJ, Hansel DE, Lin O, McKenney J, Montironi R, Paner GP, al-Ahmadie HA, Algaba F, Ali S, Alvarado-Cabrero I, Bubendorf L, Cheng L, Cheville JC, Kristiansen G, Cote RJ, Delahunt B, Eble JN, Genega EM, Gulmann C, Hartmann A, Langner C, Lopez-Beltran A, Magi-Galluzzi C, Merce J, Netto GJ, Oliva E, Rao P, Ro JY, Srigley JR, Tickoo SK, Tsuzuki T, Umar SA, van der Kwast T, Young RH, Soloway MS (2015) Update for the practicing pathologist: the international consultation on urologic disease-European association of urology consultation on bladder cancer. Mod Pathol 28(5):612–630
Zhou HH, Liu LY, Yu GH, Qu GM, Gong PY, Yu X, Yang P (2017) Analysis of clinicopathological features and prognostic factors in 39 cases of bladder neuroendocrine carcinoma. Anticancer Res 37(8):4529–4537
Gopalan A, Sharp DS, Fine SW, Tickoo SK, Herr HW, Reuter VE, Olgac S (2009) Urachal carcinoma: a clinicopathologic analysis of 24 cases with outcome correlation. Am J Surg Pathol 33(5):659–668
Amin MB, Smith SC, Eble JN, Rao P, Choi WW, Tamboli P et al (2014) Glandular neoplasms of the urachus: a report of 55 cases emphasizing mucinous cystic tumors with proposed classification. Am J Surg Pathol 38(8):1033–1045
Paner GP, Annaiah C, Gulmann C, Rao P, Ro JY, Hansel DE et al (2014) Immunohistochemical evaluation of novel and traditional markers associated with urothelial differentiation in a spectrum of variants of urothelial carcinoma of the urinary bladder. Hum Pathol 45(7):1473–1482
Kosem M, Sengul E (2005) Clear cell adenocarcinoma of the urinary bladder. Scand J Urol Nephrol 39(1):89–92
Lah K, Desai D, Hadway P, Perry-Keene J, Coughlin G (2013) Primary vesical clear cell adenocarcinoma arising in endometriosis: a rare case of mullerian origin. Anticancer Res 33(2):615–617
Sung MT, Zhang S, MacLennan GT, Lopez-Beltran A, Montironi R, Wang M, Tan PH, Cheng L (2008) Histogenesis of clear cell adenocarcinoma in the urinary tract: evidence of urothelial origin. Clin Cancer Res 14(7):1947–1955
Alexiev BA, Tavora F (2013) Histology and immunohistochemistry of clear cell adenocarcinoma of the urethra: histogenesis and diagnostic problems. Virchows Arch 462(2):193–201
Gilcrease MZ, Delgado R, Vuitch F, Albores-Saavedra J (1998) Clear cell adenocarcinoma and nephrogenic adenoma of the urethra and urinary bladder: a histopathologic and immunohistochemical comparison. Hum Pathol 29(12):1451–1456
Brimo F, Herawi M, Sharma R, Netto GJ, Epstein JI, Illei PB (2011) Hepatocyte nuclear factor-1beta expression in clear cell adenocarcinomas of the bladder and urethra: diagnostic utility and implications for histogenesis. Hum Pathol 42(11):1613–1619
Reis LO, Billis A, Ferreira FT, Ikari LY, Stellini RF, Ferreira U (2011) Female urethral carcinoma: evidences to origin from Skene's glands. Urol Oncol 29(2):218–223
Royce TJ, Lin CC, Gray PJ, Shipley WU, Jemal A, Efstathiou JA (2018) Clinical characteristics and outcomes of nonurothelial cell carcinoma of the bladder: results from the National Cancer Data Base. Urol Oncol 36(2):78.e1–78.e12
Moschini M, D’Andrea D, Korn S, Irmak Y, Soria F, Comperat E et al (2017) Characteristics and clinical significance of histological variants of bladder cancer. Nat Rev Urol 14(11):651–668
Davaro F, Schaefer J, May A, Raza J, Siddiqui S, Hamilton Z (2019) Invasive non-urachal adenocarcinoma of the bladder: analysis of the National Cancer Database. World J Urol 37(3):497–505
Shah JB, McConkey DJ, Dinney CP (2011) New strategies in muscle-invasive bladder cancer: on the road to personalized medicine. Clin Cancer Res 17(9):2608–2612
Seiler R, Ashab HAD, Erho N, van Rhijn BWG, Winters B, Douglas J, van Kessel K, Fransen van de Putte E, Sommerlad M, Wang NQ, Choeurng V, Gibb EA, Palmer-Aronsten B, Lam LL, Buerki C, Davicioni E, Sjödahl G, Kardos J, Hoadley KA, Lerner SP, McConkey D, Choi W, Kim WY, Kiss B, Thalmann GN, Todenhöfer T, Crabb SJ, North S, Zwarthoff EC, Boormans JL, Wright J, Dall'Era M, van der Heijden M, Black PC (2017) Impact of molecular subtypes in muscle-invasive bladder cancer on predicting response and survival after neoadjuvant chemotherapy. Eur Urol 72(4):544–554
Grignon D, Brimo F, Comperat E, Delahunt B, Koch M, Lopez-Beltran A, et al. (2018) Urinary tract carcinoma, histopathology reporting guide, biopsy and transurethral resection specimen, 1st Edition. In: Reporting ICoC, editor. Sydney, Australia
Alfred Witjes J, Lebret T, Comperat EM, Cowan NC, De Santis M, Bruins HM et al (2017) Updated 2016 EAU guidelines on muscle-invasive and metastatic bladder cancer. Eur Urol 71(3):462–475
Willis DL, Flaig TW, Hansel DE, Milowsky MI, Grubb RL, Al-Ahmadie HA et al (2014) Micropapillary bladder cancer: current treatment patterns and review of the literature. Urol Oncol 32(6):826–832
Hansel DE, Amin MB, Comperat E, Cote RJ, Knuchel R, Montironi R et al (2013) A contemporary update on pathology standards for bladder cancer: transurethral resection and radical cystectomy specimens. Eur Urol 63(2):321–332
Roupret M, Babjuk M, Comperat E, Zigeuner R, Sylvester RJ, Burger M et al (2018) European Association of urology guidelines on upper urinary tract urothelial carcinoma: 2017 update. Eur Urol 73(1):111–122
Moschini M, Sharma V, Dell'oglio P, Cucchiara V, Gandaglia G, Cantiello F, Zattoni F, Pellucchi F, Briganti A, Damiano R, Montorsi F, Salonia A, Colombo R (2016) Comparing long-term outcomes of primary and progressive carcinoma invading bladder muscle after radical cystectomy. BJU Int 117(4):604–610
Fritsche HM, Burger M, Svatek RS, Jeldres C, Karakiewicz PI, Novara G, Skinner E, Denzinger S, Fradet Y, Isbarn H, Bastian PJ, Volkmer BG, Montorsi F, Kassouf W, Tilki D, Otto W, Capitanio U, Izawa JI, Ficarra V, Lerner S, Sagalowsky AI, Schoenberg M, Kamat A, Dinney CP, Lotan Y, Shariat SF (2015) Corrigendum to “characteristics and outcomes of patients with clinical T1 grade 3 urothelial carcinoma treated with radical cystectomy: results from an international cohort” [Eur Urol 2010;57:300-9]. Eur Urol 68(1):171
Epstein JI, Amin MB, Reuter VR, Mostofi FK (1998) The World Health Organization/International Society of Urological Pathology consensus classification of urothelial (transitional cell) neoplasms of the urinary bladder. Bladder Consensus Conference Committee. Am J Surg Pathol 22(12):1435–1448
Stein JP, Clark P, Miranda G, Cai J, Groshen S, Skinner DG (2005) Urethral tumor recurrence following cystectomy and urinary diversion: clinical and pathological characteristics in 768 male patients. J Urol 173(4):1163–1168
Cheng L, Neumann RM, Nehra A, Spotts BE, Weaver AL, Bostwick DG (2000) Cancer heterogeneity and its biologic implications in the grading of urothelial carcinoma. Cancer 88(7):1663–1670
Comperat E, Babjuk M, Algaba F, Amin M, Brimo F, Grignon D et al (2019) SIU-ICUD on bladder cancer: pathology. World J Urol 37(1):41–50
Gofrit ON, Pizov G, Shapiro A, Duvdevani M, Yutkin V, Landau EH, Zorn KC, Hidas G, Pode D (2014) Mixed high and low grade bladder tumors--are they clinically high or low grade? J Urol 191(6):1693–1696
Downes MR, Weening B, van Rhijn BW, Have CL, Treurniet KM, van der Kwast TH (2017) Analysis of papillary urothelial carcinomas of the bladder with grade heterogeneity: supportive evidence for an early role of CDKN2A deletions in the FGFR3 pathway. Histopathology 70(2):281–289
Comperat EM, Burger M, Gontero P, Mostafid AH, Palou J, Roupret M et al (2019) Grading of urothelial carcinoma and the new “World Health Organisation classification of tumours of the urinary system and male genital organs 2016”. Eur Urol Focus (3):457–466.
Mikulowski P, Hellsten S (2005) T1 G1 urinary bladder carcinoma: fact or fiction? Scand J Urol Nephrol 39(2):135–137
van Rhijn BW, Musquera M, Liu L, Vis AN, Zuiverloon TC, van Leenders GJ et al (2015) Molecular and clinical support for a four-tiered grading system for bladder cancer based on the WHO 1973 and 2004 classifications. Mod Pathol 28(5):695–705
Kruger S, Thorns C, Bohle A, Feller AC (2003) Prognostic significance of a grading system considering tumor heterogeneity in muscle-invasive urothelial carcinoma of the urinary bladder. Int Urol Nephrol 35(2):169–173
Cao D, Vollmer RT, Luly J, Jain S, Roytman TM, Ferris CW, Hudson MA (2010) Comparison of 2004 and 1973 World Health Organization grading systems and their relationship to pathologic staging for predicting long-term prognosis in patients with urothelial carcinoma. Urology 76(3):593–599
Soave A, Schmidt S, Dahlem R, Minner S, Engel O, Kluth LA et al (2015) Does the extent of variant histology affect oncological outcomes in patients with urothelial carcinoma of the bladder treated with radical cystectomy. Urol Oncol 33(1):21.e1–21.e9
WHO (World Health Organization) (2004) In: Eble J, Sauter G, Epstein J, Sesterhenn I (eds) World Health Organization classification of tumours. Pathology and genetics of tumours of the urinary system and male genital organ. IARC Press, Lyon, France
Tilki D, Svatek RS, Novara G, Seitz M, Godoy G, Karakiewicz PI, Kassouf W, Fradet Y, Fritsche HM, Sonpavde G, Izawa JI, Ficarra V, Lerner SP, Schoenberg M, Stief CG, Dinney CP, Skinner E, Lotan Y, Sagalowsky AI, Reich O, Shariat SF (2010) Stage pT0 at radical cystectomy confers improved survival: an international study of 4,430 patients. J Urol 184(3):888–894
Amin MB, Trpkov K, Lopez-Beltran A, Grignon D (2014) Best practices recommendations in the application of immunohistochemistry in the bladder lesions: report from the International Society of Urologic Pathology consensus conference. Am J Surg Pathol 38(8):e20–e34
Kassouf W, Spiess PE, Brown GA, Munsell MF, Grossman HB, Siefker-Radtke A, Dinney CP, Kamat AM (2007) P0 stage at radical cystectomy for bladder cancer is associated with improved outcome independent of traditional clinical risk factors. Eur Urol 52(3):769–774
Ananthanarayanan V, Pan Y, Tretiakova M, Amin MB, Cheng L, Epstein JI, Grignon DJ, Hansel DE, Jimenez RE, McKenney J, Montironi R, Oliva E, Osunkoya AO, Rao P, Reuter VE, Ro JY, Shen SS, Srigley JR, Tsuzuki T, Yao JL, Antic T, Haber M, Taxy JB, Paner GP (2014) Influence of histologic criteria and confounding factors in staging equivocal cases for microscopic perivesical tissue invasion (pT3a): an interobserver study among genitourinary pathologists. Am J Surg Pathol 38(2):167–175
Bastian PJ, Hutterer GC, Shariat SF, Rogers CG, Palapattu GS, Lotan Y, Vazina A, Amiel GE, Gupta A, Sagalowsky AI, Lerner SP, Schoenberg MP, Karakiewicz PI, Bladder Cancer Research Consortium (2008) Macroscopic, but not microscopic, perivesical fat invasion at radical cystectomy is an adverse predictor of recurrence and survival. BJU Int 101(4):450–454
Neuzillet Y, Lebret T, Molinie V, Yonneau L, Herve JM, Theodore C, Botto H (2012) Perivesical fat invasion in bladder cancer: implications for prognosis comparing pT2b, pT3a and pT3b stages and consequences for adjuvant chemotherapy indications. BJU Int 110(11):1736–1741
Tamas EF, Stephenson AJ, Campbell SC, Montague DK, Trusty DC, Hansel DE (2009) Histopathologic features and clinical outcomes in 71 cases of bladder diverticula. Arch Pathol Lab Med 133(5):791–796
Idrees MT, Alexander RE, Kum JB, Cheng L (2013) The spectrum of histopathologic findings in vesical diverticulum: implications for pathogenesis and staging. Hum Pathol 44(7):1223–1232
Walker NF, Gan C, Olsburgh J, Khan MS (2014) Diagnosis and management of intradiverticular bladder tumours. Nat Rev Urol 11(7):383–390
Kluth LA, Rieken M, Xylinas E, Kent M, Rink M, Roupret M et al (2014) Gender-specific differences in clinicopathologic outcomes following radical cystectomy: an international multi-institutional study of more than 8000 patients. Eur Urol 66(5):913–919
von Rundstedt FC, Mata DA, Groshen S, Stein JP, Skinner DG, Stadler WM et al (2015) Significance of lymphovascular invasion in organ-confined, node-negative urothelial cancer of the bladder: data from the prospective p53-MVAC trial. BJU Int 116(1):44–49
Neuzillet Y, Soulie M, Larre S, Roupret M, Defortescu G, Murez T, Pignot G, Descazeaud A, Patard JJ, Bigot P, Salomon L, Colin P, Rigaud J, Bastide C, Durand X, Valeri A, Kleinclauss F, Bruyere F, Pfister C, Comité de Cancérologie de l’Association Française d'Urologie (CCAFU) (2013) Positive surgical margins and their locations in specimens are adverse prognosis features after radical cystectomy in non-metastatic carcinoma invading bladder muscle: results from a nationwide case-control study. BJU Int 111(8):1253–1260
Dotan ZA, Kavanagh K, Yossepowitch O, Kaag M, Olgac S, Donat M et al (2007) Positive surgical margins in soft tissue following radical cystectomy for bladder cancer and cancer specific survival. J Urol 178(6):2308–2312 discussion 13
Hadjizacharia P, Stein JP, Cai J, Miranda G (2009) The impact of positive soft tissue surgical margins following radical cystectomy for high-grade, invasive bladder cancer. World J Urol 27(1):33–38
Raj GV, Tal R, Vickers A, Bochner BH, Serio A, Donat SM, Herr H, Olgac S, Dalbagni G (2006) Significance of intraoperative ureteral evaluation at radical cystectomy for urothelial cancer. Cancer 107(9):2167–2172
Hoang AN, Agarwal PK, Walton-Diaz A, Wood CG, Metwalli AR, Kassouf W, Brown GA, Black PC, Urbauer DL, Grossman HB, Dinney CP, Kamat AM (2014) Clinical significance of ureteric ‘skip lesions’ at the time of radical cystectomy: the M.D. Anderson experience and literature review. BJU Int 113(5b):E28–E33
Schumacher MC, Scholz M, Weise ES, Fleischmann A, Thalmann GN, Studer UE (2006) Is there an indication for frozen section examination of the ureteral margins during cystectomy for transitional cell carcinoma of the bladder? J Urol 176(6 Pt 1):2409–2413 discussion 13
Tollefson MK, Blute ML, Farmer SA, Frank I (2010) Significance of distal ureteral margin at radical cystectomy for urothelial carcinoma. J Urol 183(1):81–86
Lee SE, Byun SS, Hong SK, Chang IH, Kim YJ, Gill MC, Song SH, Kim KT (2006) Significance of cancer involvement at the ureteral margin detected on routine frozen section analysis during radical cystectomy. Urol Int 77(1):13–17
Gordetsky J, Bivalacqua T, Schoenberg M, Epstein JI (2014) Ureteral and urethral frozen sections during radical cystectomy or cystoprostatectomy: an analysis of denudation and atypia. Urology 84(3):619–623
Amin M, Edge S, Greene F, Byrd D, Brookland R, Washington M et al (2017) AJCC cancer staging manual, 8th edn. Springer, New York
Revelo MP, Cookson MS, Chang SS, Shook MF, Smith JA Jr, Shappell SB (2008) Incidence and location of prostate and urothelial carcinoma in prostates from cystoprostatectomies: implications for possible apical sparing surgery. J Urol 179(5 Suppl):S27–S32
Shen SS, Lerner SP, Muezzinoglu B, Truong LD, Amiel G, Wheeler TM (2006) Prostatic involvement by transitional cell carcinoma in patients with bladder cancer and its prognostic significance. Hum Pathol 37(6):726–734
Pagano F, Bassi P, Ferrante GL, Piazza N, Abatangelo G, Pappagallo GL, Garbeglio A (1996) Is stage pT4a (D1) reliable in assessing transitional cell carcinoma involvement of the prostate in patients with a concurrent bladder cancer? A necessary distinction for contiguous or noncontiguous involvement. J Urol 155(1):244–247
Patel P, Reikie BA, Maxwell JP, Yilmaz A, Gotto GT, Trpkov K (2013) Long-term clinical outcome of inverted urothelial papilloma including cases with focal papillary pattern: is continuous surveillance necessary? Urology 82(4):857–860
Masson-Lecomte A, Vordos D, Hoznek A, Yiou R, Allory Y, Abbou CC, de la Taille A, Salomon L (2013) External validation of extranodal extension and lymph node density as predictors of survival in node-positive bladder cancer after radical cystectomy. Ann Surg Oncol 20(4):1389–1394
Fajkovic H, Cha EK, Jeldres C, Robinson BD, Rink M, Xylinas E, Chromecki TF, Breinl E, Svatek RS, Donner G, Tagawa ST, Tilki D, Bastian PJ, Karakiewicz PI, Volkmer BG, Novara G, Joual A, Faison T, Sonpavde G, Daneshmand S, Lotan Y, Scherr DS, Shariat SF (2013) Extranodal extension is a powerful prognostic factor in bladder cancer patients with lymph node metastasis. Eur Urol 64(5):837–845
Cancer IUa (2016) In: GM BJD, Wittekind C (eds) TNM classification of malignant tumours, 8th edn. Wiley-Blackwell, New York
Eisenberg MS, Boorjian SA, Cheville JC, Thompson RH, Thapa P, Kaushik D, Frank I The SPARC score: a multifactorial outcome prediction model for patients undergoing radical cystectomy for bladder cancer. J Urol 2013;190(6):2005–10
Picozzi S, Ricci C, Gaeta M, Ratti D, Macchi A, Casellato S, Bozzini G, Carmignani L (2012) Upper urinary tract recurrence following radical cystectomy for bladder cancer: a meta-analysis on 13,185 patients. J Urol 188(6):2046–2054
Huguet J, Monllau V, Sabate S, Rodriguez-Faba O, Algaba F, Palou J et al (2008) Diagnosis, risk factors, and outcome of urethral recurrences following radical cystectomy for bladder cancer in 729 male patients. Eur Urol 53(4):785–792 discussion 92–3
Boorjian SA, Kim SP, Weight CJ, Cheville JC, Thapa P, Frank I (2011) Risk factors and outcomes of urethral recurrence following radical cystectomy. Eur Urol 60(6):1266–1272
Krasnow RE, Drumm M, Roberts HJ, Niemierko A, Wu CL, Wu S, Zhang J, Heney NM, Wszolek MF, Blute ML, Feldman AS, Lee RJ, Zietman AL, Shipley WU, Efstathiou JA (2017) Clinical outcomes of patients with histologic variants of urothelial cancer treated with trimodality bladder-sparing therapy. Eur Urol 72(1):54–60
Rosenblatt R, Sherif A, Rintala E, Wahlqvist R, Ullen A, Nilsson S et al (2012) Pathologic downstaging is a surrogate marker for efficacy and increased survival following neoadjuvant chemotherapy and radical cystectomy for muscle-invasive urothelial bladder cancer. Eur Urol 61(6):1229–1238
Fleischmann A, Thalmann GN, Perren A, Seiler R (2014) Tumor regression grade of urothelial bladder cancer after neoadjuvant chemotherapy: a novel and successful strategy to predict survival. Am J Surg Pathol 38(3):325–332
Pignot G, Salomon L, Lebacle C, Neuzillet Y, Lunardi P, Rischmann P, Zerbib M, Champy C, Roupret M, Peyronnet B, Verhoest G, Murez T, Quintens H, Larré S, Houédé N, Compérat E, Soulié M, Pfister C (2015) Prostate cancer incidence on cystoprostatectomy specimens is directly linked to age: results from a multicentre study. BJU Int 115(1):87–93
Bruins HM, Djaladat H, Ahmadi H, Sherrod A, Cai J, Miranda G, Skinner EC, Daneshmand S (2013) Incidental prostate cancer in patients with bladder urothelial carcinoma: comprehensive analysis of 1,476 radical cystoprostatectomy specimens. J Urol 190(5):1704–1709
Author information
Authors and Affiliations
Contributions
All authors (Compérat E, Srigley JR, Brimo F, Delahunt B, Koch M, Lopez-Beltran A, Reuter V, Samaratunga H, Shanks JH, Tsuzuki T, van der Kwast T, Varma M, Webster F Grignon D) have contributed equally to the paper as well with literature research, but also during telephone conferences and discussions. The dataset published online (ICCR-cancer.org) was written by all authors, while the final paper was written by the corresponding author. The paper has been corrected and approved by all authors. Ms. Webster was mainly involved in logistics and editing.
Corresponding author
Ethics declarations
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Part of the Topical Collection entitled ‘International Collaboration on Cancer Reporting-Collection’
Rights and permissions
About this article
Cite this article
Compérat, E., Srigley, J.R., Brimo, F. et al. Dataset for the reporting of carcinoma of the bladder—cystectomy, cystoprostatectomy and diverticulectomy specimens: recommendations from the International Collaboration on Cancer Reporting (ICCR). Virchows Arch 476, 521–534 (2020). https://doi.org/10.1007/s00428-019-02727-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-019-02727-1