Abstract
Purpose of Review
The present review aims to highlight the noise effects on the patients’ well-being and by inference on their recovery, during their hospitalization, and also the effectiveness of applied interventions to reduce noise in the health care environment.
Recent Findings
Key findings reported in relevant studies and conducted during the last 4 years are as follows: (a) noise continues to be above guideline values in health care facilities; (b) noise can disturb the sleep of the patients, can affect their rest and the communication between patients/staff/visitors, and finally can affect the staff effectiveness; (c) interventions to reduce the noise are promising but not well proven; and (d) the derived conclusions about the relationship between noise and the healing process are made indirectly and not by measurable patients’ physical parameters.
Summary
The pathways that theoretically connect noise and the healing of the patients are numerous and still unclear. An extensively examined pathway infers that noise can disturb sleep and thus may prevent the patient’s recovery. Other pathways that relate noise to the recovery of the inpatients remain unknown, such as the aggravation/degradation of measureable physical parameters or the re-hospitalization due to noise, or the effect of the low-frequency noise. A protocol to conduct noise monitoring is required, as well as validated questionnaires, to examine the inpatient’s subjective perceptions for their acoustic environment. This may lead to comparable results among the relevant studies and hence to robust interventions for the improvement of the noise environment for hospitalized patients.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Adam K. Sleep as a Restorative Process and a Theory to Explain Why. In: McConnell PS, Boer GJ, Romijn HJ, Van De Poll NE, Corner MA, editors. Progress in Brain Research. Elsevier. 1980;289–305.
Afshar PF, Bahramnezhad F, Asgari P, Shiri M. Effect of white noise on sleep in patients admitted to a coronary care. J Caring Sci. 2016;5(2):103.
Andrade KP, LLAd O, Souza RP, Matos IM. Noise level measurement and its effects on hospital employees based on complaint reports. Rev CEFAC. 2016;18(6):1379–88.
Allaouchiche B, Duflo F, Debon R, Bergeret A, Chassard D. Noise in the postanaesthesia care unit. Br J Anaesth. 2002;88(3):369–73. https://doi.org/10.1093/bja/88.3.369.
Applebaum D, Calo O, Neville K. Implementation of quiet time for noise reduction on a medical-surgical unit. JONA. 2016;46(12):669–74.
A.o.A.A. Consultants (2017). Association of australasian acoustical consultants guideline for healthcare facilities, version 2.0. https://aaac.org.au/resources/Documents/Public/Healthcare%20Facilities%20V2.0.pdf (assessed 17 Sept 2019).
Babisch W. The noise/stress concept, risk assessment and research needs. Noise Health. 2002;4(16):1.
Bani Younis M, Hayajneh F, Batiha A-M. Measurement and nonpharmacologic management of sleep disturbance in the intensive care units: a literature review. Crit Care Nurs Q. 2019a;42(1):75–80. https://doi.org/10.1097/cnq.0000000000000240.
Bani Younis MK, Hayajneh FA, Alduraidi H. Effectiveness of using eye mask and earplugs on sleep length and quality among intensive care patients: a quasi-experimental study. Int J Nurs Pract. 2019b;25(3):e12740. https://doi.org/10.1111/ijn.12740.
Basner M, Babisch W, Davis A, Brink M, Clark C, Janssen S, et al. Auditory and non-auditory effects of noise on health. Lancet. 2014;383(9925):1325–32.
Basner M, McGuire S. WHO environmental noise guidelines for the European region: a systematic review on environmental noise and effects on sleep. Int J Environ Res Public Health. 2018;15(3):519.
Berglund B, Lindvall T, Schwela DH, World Health Organization O, Environmental Health T. Guidelines for community noise. Geneva: World Health Organization; 1999.
Bion V, Lowe ASW, Puthucheary Z, Montgomery H. Reducing sound and light exposure to improve sleep on the adult intensive care unit: an inclusive narrative review. J Intensive Care Soc. 2018;19(2):138–46. https://doi.org/10.1177/1751143717740803.
Bliefnick JM, Ryherd EE, Jackson R. Evaluating hospital soundscapes to improve patient experience. J Acoust Soc Am. 2019;145(2):1117–28. https://doi.org/10.1121/1.5090493.
Blomkvist V, Eriksen CA, Theorell T, Ulrich R, Rasmanis G. Acoustics and psychosocial environment in intensive coronary care. Occup Environ Med. 2005;62(3):e1.
Burdick K, Courtney M, Wallace MT, Baum Miller SH, Schlesinger JJ. Living and working in a multisensory world: from basic neuroscience to the hospital. Multimodal Technol Interact. 2019;3(1):2.
Camuccio CA, Sanavia M, Cutrone F, Marella I, Gregio M, Cabbia C, et al. Noise levels in an acute psychiatric unit: an exploratory observational study. Issues Mental Health Nurs. 2019;40(6):493–502. https://doi.org/10.1080/01612840.2018.1557301.
Carvalhais C, Santos J, Xavier A, Silva MV. Noise reduction and control in hospital environment: design of the NeoNoise project. In: Ahmed N, ed. Advances in Noise Analysis, Mitigation and Control. Rijeka: InTech; 2016;229–244. https://www.intechopen.com/books/advances-in-noise-analysis-mitigation-and-control/noise-reduction-and-control-in-hospital-environment-design-of-the-neonoise-project. Accessed 25 Dec 2019.
Choiniere DB. The effects of hospital noise. Nurs Adm Q. 2010;34(4):327–33. https://doi.org/10.1097/NAQ.0b013e3181f563db.
Cowan JP. Psychological Effects of Sound Exposure. In: Cowan JP, editor. The Effects of Sound on People. John Wiley & Sons; 2016;81–101.
Cunha M, Silva N. Hospital noise and patients’ wellbeing. Procedia Soc Behav Sci. 2015;171:246–51. https://doi.org/10.1016/j.sbspro.2015.01.117.
Delaney L, Litton E, Van Haren F. The effectiveness of noise interventions in the ICU. Currt Opin Anesthesiol. 2019;32(2):144–9. https://doi.org/10.1097/aco.0000000000000708.
Delaney LJ. The role of sleep in patient recovery. Aust Nurs Midwifery J. 2016;23(7):26–9.
Delaney LJ, Currie MJ, Huang H-CC, Lopez V, Van Haren F. “They can rest at home”: an observational study of patients’ quality of sleep in an Australian hospital. BMC Health Serv Res. 2018;18(1):524. https://doi.org/10.1186/s12913-018-3201-z.
Gabor JY, Cooper AB, Crombach SA, Lee B, Kadikar N, Bettger HE, et al. Contribution of the intensive care unit environment to sleep disruption in mechanically ventilated patients and healthy subjects. Am J Respir Crit Care Med. 2003;167(5):708–15. https://doi.org/10.1164/rccm.2201090.
Garside J, Stephenson J, Curtis H, Morrell M, Dearnley C, Astin F. Are noise reduction interventions effective in adult ward settings? A systematic review and meta analysis. Appl Nurs Res. 2018;44:6–17. https://doi.org/10.1016/j.apnr.2018.08.004.
Hagerman I, Rasmanis G, Blomkvist V, Ulrich R, Anne Eriksen C, Theorell T. Influence of intensive coronary care acoustics on the quality of care and physiological state of patients. Int J Cardiol. 2005;98(2):267–70. https://doi.org/10.1016/j.ijcard.2003.11.006.
Hahad O, Beutel M, Gori T, Schulz A, Blettner M, Pfeiffer N, et al. Annoyance to different noise sources is associated with atrial fibrillation in the Gutenberg Health Study. Int J Cardiol. 2018;264:79–84. https://doi.org/10.1016/j.ijcard.2018.03.126.
Hsu S-M, Ko W-J, Liao W-C, Huang S-J, Chen RJ, Li C-Y, et al. Associations of exposure to noise with physiological and psychological outcomes among post-cardiac surgery patients in ICUs. Clinics (Sao Paulo). 2010;65(10):985–9. https://doi.org/10.1590/s1807-59322010001000011.
Jones K. Environmental Noise and Health: A Review. ERCD REPORT 0907, City: UK Civil Aviation Authority, 2010. https://publicapps.caa.co.uk/docs/33/ERCD0907.pdf. Accessed 25 Dec 2019.
Kane HS, Dacanay D, Renzi J, Wilson L. The Shhh Campaign: Noise Reduction to Improve Patient Outcomes. 2018. https://sigma.nursingrepository.org/handle/10755/624280. Accessed 25 Dec 2019.
Korompeli A, Muurlink O, Kavrochorianou N, Katsoulas T, Fildissis G, Baltopoulos G. Circadian disruption of ICU patients: a review of pathways, expression, and interventions. J Crit Care. 2017;38:269–77. https://doi.org/10.1016/j.jcrc.2016.12.006.
Lawson N, Thompson K, Saunders G, Saiz J, Richardson J, Brown D, et al. Sound intensity and noise evaluation in a critical care unit. Am J Crit Care. 2010;19(6):e88–98. https://doi.org/10.4037/ajcc2010180.
Loupa G, Fotopoulou S, Tsagarakis KP. A tool for analysing the interdependence of indoor environmental quality and reported symptoms of the hospitals’ personnel. J Risk Res. 2015:1–14. https://doi.org/10.1080/13669877.2015.1119182.
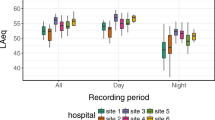
Loupa G, Katikaridis A, Karali D, Rapsomanikis S. Mapping the noise in a Greek general hospital. Sci Total Environ. 2019;646:923–9.
Mariconte R, Giliberti C, Cavuto C, Strigari L, editors. Noise in healthcare facilities. 22nd International Congress on Sound and Vibration, ICSV 2015; 2015: International Institute of Acoustics and Vibrations. https://www.researchgate.net/profile/Raffaele_Mariconte/publication/280096374_NOISE_IN_HEALTHCARE_FACILITIES/links/55a8d69008aea3d0867ca7ea/NOISE-IN-HEALTHCARE-FACILITIES.pdf. Accessed 25 Dec 2019.
McGough NNH, Keane T, Uppal A, Dumlao M, Rutherford W, Kellogg K, et al. Noise reduction in progressive care units. J Nurs Care Qual. 2018;33(2):166–72. https://doi.org/10.1097/ncq.0000000000000275.
Messingher G, Ryherd E, Ackerman J. Hospital noise and staff performance. J Acoust Soc Am. 2012;132(3):2031.
Milani RV, Bober RM, Lavie CJ, Wilt JK, Milani AR, White CJ. Reducing hospital toxicity: impact on patient outcomes. Am J Med. 2018;131(8):961–6. https://doi.org/10.1016/j.amjmed.2018.04.013.
Montes-González D, Barrigón-Morillas JM, Gómez Escobar V, Vílchez-Gómez R, Rey-Gozalo G, Atanasio-Moraga P, et al. Environmental noise around hospital areas: a case study. Environments. 2019;6(4):41.
Plummer NR, Herbert A, Blundell JE, Howarth R, Baldwin J, Laha S. SoundEar noise warning devices cause a sustained reduction in ambient noise in adult critical care. J Intensive Care Soc. 2018;20(2):106–10. https://doi.org/10.1177/1751143718767773.
Salonen H, Lahtinen M, Lappalainen S, Nevala N, Knibbs LD, Morawska L, et al. Physical characteristics of the indoor environment that affect health and wellbeing in healthcare facilities: a review. Intell Build Int. 2013;5(1):3–25.
Short M, Pearson A. Effects of noise pollution on healthcare staff and patients. A White Paper, Retrieve from: https://www.soundmask.com.au/pdf/2011whitepaper-v2.pdf. Accessed 26 Dec 2019.
Simons KS, Verweij E, Lemmens PM, Jelfs S, Park M, Spronk PE, et al. Noise in the intensive care unit and its influence on sleep quality: a multicenter observational study in Dutch intensive care units. Crit Care. 2018;22(1):250.
Smith A, Whitney H, Thomas M, Perry K, Brockman P. Effects of caffeine and noise on mood, performance and cardiovascular functioning. Hum Psychopharmacol Clin Exp. 1997;12(1):27–33.
Szalma JL, Hancock PA. Noise effects on human performance: a meta-analytic synthesis. Psychol Bull. 2011;137(4):682–707.
Tamura H, Ohgami N, Yajima I, Iida M, Ohgami K, Fujii N, et al. Chronic exposure to low frequency noise at moderate levels causes impaired balance in mice. PLoS One. 2012;7(6):e39807.
Tan X, van Egmond L, Partinen M, Lange T, Benedict C. A narrative review of interventions for improving sleep and reducing circadian disruption in medical inpatients. Sleep Med. 2019;59:42–50. https://doi.org/10.1016/j.sleep.2018.08.007.
Trovato G, Paredes R, Balvin J, Cuellar F, Thomsen NB, Bech S et al., editors. The Sound or Silence: Investigating the Influence of Robot Noise on Proxemics. 2018 27th IEEE International Symposium on Robot and Human Interactive Communication (RO-MAN); 2018;27–31. https://ieeexplore.ieee.org/stamp/stamp.jsp?arnumber=8525795. Accessed 25 Dec 2019.
Tsara V, Nena E, Serasli E, Vasileiadis V, Matamis D, Christaki P. Noise levels in Greek hospitals. Noise & health. 2008;10(41):110–112. https://doi.org/10.4103/1463-1741.44350.
United States Environmental Protection Agency. Information on levels of environmental noise requisite to protect public health and welfare with adequate margin of safety (report no. 550-9-74-004). Washington, DC: Government Printing Office; 1974.
Walker ED, Brammer A, Cherniack MG, Laden F, Cavallari JM. Cardiovascular and stress responses to short-term noise exposures—a panel study in healthy males. Environ Res. 2016;150:391–7.
Walker L, Karl CA. The hospital (not so) quiet zone: creating an environment for patient satisfaction through noise reduction strategies. HERD. 2019;12(4):197–202. https://doi.org/10.1177/1937586719839229.
Xyrichis A, Wynne J, Mackrill J, Rafferty AM, Carlyle A. Noise pollution in hospitals. BMJ. 2018;363:k4808. https://doi.org/10.1136/bmj.k4808.
Zannin P, Ferraz F. Assessment of indoor and outdoor noise pollution at a university hospital based on acoustic measurements and noise mapping. Open J Acoust. 2016;6(4):71–85. https://doi.org/10.4236/oja.2016.64006.
Zannin PHT, Milanês ML, De Oliveira Filho MVM. Evaluation of noise in the vicinity of a hospital and a gated community. Curr Urban Stud. 2019;7(1):59–75. https://doi.org/10.4236/cus.2019.71004.
Zhang Y, Tzortzopoulos P, Kagioglou M. Healing built-environment effects on health outcomes: environment–occupant–health framework. Build Res Inf. 2019;47(6):747–66. https://doi.org/10.1080/09613218.2017.1411130.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
There is no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Noise Pollution
Rights and permissions
About this article
Cite this article
Loupa, G. Influence of Noise on Patient Recovery. Curr Pollution Rep 6, 1–7 (2020). https://doi.org/10.1007/s40726-019-00134-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40726-019-00134-3