Abstract
Soft-tissue bacterial infection can progress to severe sepsis and septic shock as a result of a disproportionate inflammatory response, characterized by an excessive release of cytokines and influx of immune cells. Reltecimod (previously known as AB103 or p2TA), a peptide derived from the T-cell receptor CD28, modulates the host immune response by targeting the co-stimulatory pathway, which is essential for the induction of multiple pro-inflammatory cytokines. Consequently, reltecimod has demonstrated beneficial effects against different bacterial infections, their exotoxins and endotoxins, and ionizing radiation. The dosing regimen of reltecimod was evaluated in three mouse models of infection. The effect of the number of reltecimod doses with respect to survival, cytokine/chemokine levels, and blood leukocyte profiles was assessed. Overall, mice treated with a single intravenous dose of reltecimod (5 mg/kg) at 1–2 h after infection showed significantly greater survival as compared with saline-treated controls. Mice treated with a second doses demonstrated improved survival compared with saline-treated controls. However, in all models of infection, administration of a single therapeutic dose of reltecimod was superior to two or multiple doses. Further examination showed that the single therapeutic dose of reltecimod was associated with an early (within 24 h) decrease in cytokine/chemokine levels and most circulating leukocyte subpopulations. A second dose of reltecimod did not improve these early positive effects and appeared to attenuate further changes. These results provided insight into the mechanism of action of reltecimod and established a basis for the dosing regimen utilized in clinical trials, where reltecimod is administered as a single dose.
Similar content being viewed by others
Introduction
The invasion of microbial pathogens into the bloodstream is characterized by a systemic pro-inflammatory response that can lead to severe sepsis and septic shock. It develops when the initial appropriate host response to an infection becomes amplified and subsequently dysregulated (Cohen 2002). The activation of this “first line of cellular defense” results in an excessive release of cytokines, chemokines, and other inflammatory regulators, as well as affecting the influx of immune cells, predominantly polymorphonuclear neutrophils (PMNs), into remote or affected organs and tissues. Some localized infections caused by gram-positive bacterial pathogens, including group A Streptococcus pyogenes (S. pyogenes) and Staphylococcus aureus, are complicated by manifestations of systemic toxicity and may progress to sepsis and lethal septic or toxic shock (Johansson et al. 2010; Brosnahan and Schlievert 2011). Necrotizing soft- tissue infections (NSTI) by some gram-positive pathogens can be complicated by toxic shock syndromes which can rapidly become fatal. Sepsis due to severe gram-negative bacterial infections is also a major cause of morbidity and mortality worldwide (Dellinger et al. 2008). Despite the availability of potent antimicrobial agents and advances in supportive care, mortality from sepsis has persisted at > 20% (Annane et al. 2009; Napolitano 2018) and mortality from NSTI is currently estimated as 15–25% (Barupal et al. 2019). This situation is further exacerbated by the dramatic rise in resistance to commonly used antimicrobial agents and the dearth of new antibiotics in the drug development pipeline. Consequently, there have been concerted efforts to develop agents that can either neutralize bacterial virulence factors or enhance host defenses (or both) and that, in conjunction with antibiotic therapy, may improve the outcome from severe infections.
Reltecimod (previously known as AB103 or p2TA) is a novel, 10-amino-acid immunomodulating peptide. Targeting the host immune response rather than the pathogen, reltecimod provides treatment for bacterial infections by delivering broad-spectrum coverage, independent of pathogen type, and may eliminate the risk of development of drug resistance. Furthermore, this mode of action permits the initiation of therapy at early disease stages, before the bacterial pathogen has been identified. Reltecimod modulates the inflammatory response by targeting and attenuating the critical CD28/B7-2 co-stimulatory pathway, without inhibiting it. The extracellular β-barrel homodimer interface of CD28 is remote, at the opposite pole, from the binding site for the two B7 co-ligands (Evans et al. 2005). Nevertheless, it has been shown that engagement of B7-2 and CD28 receptors can be regulated via their homodimer interfaces (Kaempfer et al. 2017; Levy et al. 2016). Binding of reltecimod to CD28 (Shirvan et al. 2018) is hypothesized to induce changes in CD28 beyond the specific binding site that act to reduce its binding to B7-2 without blocking it, thus down-regulating synapse formation and downstream events. Additionally, CD28/B7-2 and SEB/CD28 affinity are both in the micromolar range [20 μM (Collins et al. 2002) and 2.3 µM (Arad et al. 2011), respectively] resulting in reduction rather than complete blocking of CD28 B7-2 interaction.
Reltecimod has been shown to provide broad protection against polymicrobial, gram-positive (Ramachandran et al. 2013) and gram-negative bacteria (Ramachandran et al. 2015), their exotoxins and endotoxins [e.g., staphylococcal enterotoxin B (SEB) (Arad et al. 2011) and lipopolysaccharide (LPS) (Ramachandran et al. 2015)], and ionizing radiation (Mirzoeva et al. 2014). Reltecimod peptide is derived from the homodimer interface of the co-stimulatory T-cell receptor CD28, which is essential for the induction of multiple pro-inflammatory cytokines when co-stimulation is activated (Arad et al. 2011). Reltecimod does not have antimicrobial activity, and by targeting CD28, it prevents the excessive harmful inflammatory cytokine response underlying infection pathology; it significantly improves the host’s ability to respond to infection efficiently and, consequently, reduces the tissue damage caused to key organs during acute inflammation (Ramachandran et al. 2013, 2015; Mirzoeva et al. 2014). By modulating an upstream target, reltecimod attenuates a broad range of cytokines. This is in contrast to other therapeutic efforts designed to inhibit a specific cytokine (e.g., tumor necrosis factor α [TNF-α] or interleukin 1β [IL-1β]), that have been shown to be unsuccessful.
Exposure to bacterial infections, especially in sepsis, persists for long periods of time. While pharmacokinetic studies of reltecimod have indicated a short half-life in plasma (1–2 min, based on studies conducted in mice, pigs, and humans), reltecimod has pharmacodynamic effects that last for hours or even days, as demonstrated in experimental animal systems and early clinical trials in patients with necrotizing soft-tissue infections (NSTI) (clinicaltrials.gov Identifier: NCT01417780) (Ramachandran et al. 2013, 2015; Mirzoeva et al. 2014; Bulger et al. 2014). Therefore, debate arose as to the optimal therapeutic regimen for reltecimod that would be sufficient to provide sustained benefit following bacterial infection.
We therefore conducted experiments in which we compared the efficacy of single and multiple doses of reltecimod using three mouse models of infection, in which reltecimod efficacy was previously demonstrated (Ramachandran et al. 2013, 2015). The parameters compared included survival, cytokine/chemokine levels, and leukocyte profiles. We examined whether reltecimod protects mice from lethality following gram-negative, gram-positive, and polymicrobial infections and whether, in the mouse models, a single dose of reltecimod was superior to multiple doses. We present the results of these studies and correlate these findings with the effect observed on cytokine/chemokine levels and leukocyte profile.
Materials and Methods
Reagents
Chemical reagents were obtained from Sigma (St. Louis, MO), unless otherwise stated. The antibiotic cefepime was obtained from Elan Pharmaceuticals, Inc. (Dublin, Ireland).
Peptide
Reltecimod (also known as AB103 and p2TA) is a peptide with the amino acid sequence of SPMLVAYD; it has D-alanine residues abutted to its N- and C-termini to enhance protease resistance (Arad et al. 2011). Once dissolved in phosphate-buffered saline (PBS) at 1 mg/mL, reltecimod was used immediately at desired dilutions.
Bacteria
Streptococcus pyogenes strain 8198 (scarlet fever serotype M1T1, kindly provided by Dr. Jonathan Cohen (Hammersmith Hospital, London, United Kingdom), produces SPEA and SPEB, and carries genes for SPEG, SPEJ, and SMEZ (Sriskandan et al. 1996); it was cultured in Todd-Hewitt broth (Becton Dickinson) at 37 °C under aerobic conditions. Escherichia coli O18:K1:H7 (also known as “Bort” strain), a highly virulent, serum-resistant, gram-negative bacteria isolated from the spinal fluid of a neonate, was used for the peritonitis studies (Cross et al. 1993).
Animals and Ethics
Pathogen-free, female BALB/c mice (aged 8–12 weeks for the polymicrobial sepsis and peritonitis models, and aged 6–8 weeks for the thigh infection model) were obtained from Charles River Laboratories (Wilmington, Mass.). All animal studies were approved by the Brown University/Rhode Island Hospital and University of Maryland Institutional Animal Care and Use Committees (IACUCs) before experiments were initiated. Animals were housed in an IACUC-approved facility under biosafety level 2 safety conditions and were monitored by Brown University/Rhode Island Hospital and University of Maryland veterinary staffs.
Escherichia coli Peritonitis Mouse Model
Acute bacterial peritonitis was induced by intraperitoneal (IP) challenge of BALB/c mice with E. coli 018:K1 (1 × 105 colony-forming units [CFUs]), followed by IV therapy with either reltecimod or saline 4 h after challenge. The protective ability of reltecimod was tested following the induction of E. coli peritonitis in the presence of a suboptimal dose of the antibiotic cefepime (Elan Pharmaceuticals, Inc.).
Streptococcus pyogenes Thigh Infection Mouse Model
Thigh infection with Group A streptococcus (GAS) is a model for NSTI. BALB/c mice were infected intramuscularly (IM) (100 µL) in the left upper thigh with 1 × 107 CFUs of GAS. Reltecimod (2.5 or 5 mg/kg) was administered intravenously at 1 h, or at 1 h and 12 or 72 h post infection, and survival was monitored. Mice injected with phosphate-buffered saline (uninfected) served as controls.
Cecal Ligation and Puncture (CLP) Polymicrobial Sepsis Model
The murine CLP model of polymicrobial sepsis has been detailed elsewhere (Opal et al. 2005). Moxifloxacin (Schering) was given at a suboptimal dose of 5 mg/kg. Animals that underwent sham surgery were handled in the identical fashion except that, after laparotomy, the exposed cecum was not ligated or punctured. We tested the efficacy of reltecimod administered at different time points and regimens as indicated, after CLP. Moribund animals (defined as animals that were hypothermic, with temperature < 30 °C, and unable to maintain normal body posture) were euthanized and scored as lethally infected animals. For assessing the cytokine/chemokine level and leukocyte profile, another set of mice, randomized to three groups, was used. Mice were euthanized at prespecified periods after CLP (24 h or 48 h), and quantitative analysis of blood cytokines, chemokines, and leucocyte profiles was determined.
Suboptimal dose of antibiotics were used in E. coli peritonitis and CLP sepsis experimental models to allow the host to reduce the burden of bacteria, and permit the host response to re-establish homeostasis so it can control the infection. Since reltecimod is not an antibacterial agent, it will not by itself kill the bacteria. The suboptimal (subtherapeutic) amount of antibiotic allows the host, in conjunction with antibiotics, to assist in clearing the infection whereas higher doses of antibiotics alone may be sufficient to treat the infection efficaciously, without the need for reltecimod. Further, reltecimod is indicated to be used as adjunctive treatment to the standard of care, and it is envisioned that it will always be used clinically, in conjugation with antibiotics or some other therapy. In a real-life situation, patients may receive a sub-optimal amount of antibiotics, and reltecimod would be expected to improve the outcome.
Sample Preparation
At 24 h or at 24 h and 48 h after the CLP procedure, prior to euthanasia, blood specimens were collected in heparinized syringes by cardiac puncture from mice under deep terminal anesthesia, and plasma specimens were obtained by centrifugation. The sham-operated group was handled in an identical fashion except that, after laparotomy, the exposed cecum was not ligated or punctured. The sham-operated group served as baseline control.
Cytokine and Chemokine Level Determination
Mouse cytokine levels of IL-6, IL-3, IFN-γ, IL-1α, MCP-1, and RANTES were assayed in serum, using a multiplex immunoassay, with standard curves (Quansys Biosciences, Logan, UT).
Leukocyte Profile Determination
For total T cells and subsets of T-cell populations—CD4+ cells, CD8+ cells, B cells, neutrophils, and macrophages/monocytes—heparinized mouse blood samples were fixed in PBS 2% FBS 2% PFA and were washed and run on a FACSCalibur™ (BD). Data were analyzed using FlowJo (TreeStar). The fluorescent automated cell sorter (FACS) was used to identify each cell marker by labelled antibodies: CD16/32 (Clone YT1.24) to FC receptor; TCRβ-PE (Clone H57-597), CD8α-Alexa488 (Clone 53-6.7), CD4-PercP-eFluor710 (Clone GK1.5), CD49b-APC (Clone DX5), F4/80-Alexa488 (Clone BM8), Ly6C-PE (Clone HK1.4), Ly6G-PercP-eFluor710 (Clone 1A8), CD11b-APC (Clone M1/70), B220-FITC (Clone RA3-6B2), CD20-PE (Clone AISB12), and CD19-APC (Clone 1D3). Cell populations were identified using the following markers: Total cells—hemocytometer; CD4+ T cells—[CD4+, TCRβ+, CD49b+]; CD8+ T cells—[CD8+, TCR β+, CD49b+]; B cells—[B220+, CD19+ CD20+]; monocytes—[CD11b+, Ly6Chigh, F4/80+]; neutrophils—[CD11b+, Ly6Cint L6G+].
Statistical Analysis
Values are expressed as mean ± standard error of the mean. Differences between groups were analyzed using the Student t test, pEXACT (P-value from nonparametric exact Wilcoxon test), and pANOVA (P-value from parametric ANOVA on natural log-transformed values). Differences are considered statistically significant at a P-value of < 0.05.
Spearman correlations between pairs of cytokine measures at 24 h, collapsing across control and single dose groups, and at 48 h, collapsing over all three treatments, were used to measure the relationship among the cytokines measured. In addition, correlation analyses were performed to examine any associations between cytokine levels and lymphocyte profiles, and among cytokines at a given time point, both overall and within treatment groups. For this correlation analysis, results were based on Spearman rank correlations in the full sample, with similar analyses presented within treatment groups where data were available.
Results
Survival Studies
Cecal Ligation and Puncture (CLP) Polymicrobial Mouse Model
The murine CLP intra-abdominal infection model is considered a clinically relevant model for investigating polymicrobial infections and for following the effects of therapeutic agents as a well-accepted model for intra-abdominal infections or sepsis. Previous results have demonstrated that single dose intravenous (IV) administration of reltecimod, at 2, 12, or 24 h post infection (at doses of 1.25, 2.5, or 5 mg/kg), in addition to suboptimal dose of moxifloxacin administered intramuscularly (IM), increased day 7 survival by up to 100%, as compared with only 8–25% survival in control groups treated only with a suboptimal dose of moxifloxacin (P < 0.05) (Ramachandran et al. 2015).
In the initial set of experiments, we used the CLP model to compare survival among controls (n = 16) and among mice receiving either a single dose of reltecimod (IV, 2 h post CLP; n = 10) or two doses of reltecimod (IV, 2 h and 24 h post CLP; n = 10). After 7 days, both the single dose and the two doses of reltecimod significantly improved survival as compared with control (P = 0.001 and P = 0.0007, respectively). The single 5 mg/kg dose of reltecimod provided 90% survival, while two doses of reltecimod, 5 mg/kg each, yielded 40% survival. The results demonstrate that both single and two doses of reltecimod provides survival benefit as compared to control (5% survival). Surprisingly however, despite the short half-life of reltecimod and the persistence of the infectious pathogen, one dose of reltecimod provides significantly greater protection than two doses (P = 0.0002) (Fig. 1a). Further support for the superiority of a single dose of reltecimod was evident from calculation of the mean survival time (Fig. 1b). Treatment with reltecimod prolonged the mean survival time relative to control by 2.1 days (from 2.9 to 5 days) for two doses, and by 3.8 days (from 2.9 to 6.7 days) for a single dose (P < 0.005 each). The single dose of reltecimod significantly extended survival by 1.7 days as compared with two doses of reltecimod (from 5.0 to 6.7 days; P = 0.0182).
Efficacy of a single dose versus two doses of reltecimod, at 24 h interval, in a mouse model of lethal CLP infection. BALB/c mice underwent CLP surgical procedure. Reltecimod (5 mg/kg), with suboptimal moxifloxacin (5 mg/kg), was administered by IV at 2 h or at 2 h and 24 h post CLP (n = 10/group). Mice injected with suboptimal moxifloxacin (IM, 5 mg/kg) and phosphate-buffered saline (saline-treated) served as controls (n = 16). Survival was monitored for 7 days, and results are shown as Kaplan–Meier survival curves (a) and average survival time (b). *P < 0.05 versus control, **P = 0.0182 versus two doses (a); *P = 0.001, **P = 0.0007, ***P = 0.0002 (b). Kaplan–Meier survival curve was created using GraphPad Prism and average survival time histogram was created using Microsoft Excel
Lethal S. pyogenes NSTI Mouse Model
Group A streptococcus S. pyogenes (GAS) is one of the most common pathogens leading to necrotizing soft-tissue infections. Using a mouse model for GAS lethal bacterial infection, a recognized model for NSTI, we have previously shown that in the absence of antibiotic, IV administration of reltecimod as a single dose (0.5–5 mg/kg at 30 min pre-infection, or at 1 h or 5 h post infection) increased overall survival (by up to 80% as compared with infected, saline-treated controls) in the presence of a clinically isolated invasive strain of S. pyogenes (Ramachandran et al. 2013).
In order to define the optimal dosing regimen of reltecimod in this model, we performed experiments to determine the optimal number and interval between reltecimod doses. These regimens were investigated in BALB/c mice that were infected with S. pyogenes and in which the first dose was administered at a delayed time point (1 h) post infection.
Single Dose Versus Two Doses of Reltecimod at Different Concentrations
The effect of a single dose of reltecimod as compared with two doses was examined under a regimen in which the first dose was initiated at 1 h post infection and the interval to the second dose was 12 h (Fig. 2). Reltecimod doses of 2.5 mg/kg and 5 mg/kg were evaluated, and survival was monitored for 8 days. Infected, saline-treated control mice (n = 20) exhibited 20% survival. Treatment with a single dose of reltecimod 2.5 mg/kg (n = 20) resulted in 65% survival (P < 0.005 vs. control). Two doses of reltecimod at 2.5 mg/kg each (n = 20) yielded 30% survival. Survival in the two-dose group was significantly better than that for the saline-treated control group (P < 0.005 vs. control), however it was inferior to treatment by a single dose reltecimod at 2.5 mg/kg (P = 0.0043 for one vs. two reltecimod doses; log rank test). Similarly, reltecimod at 5 mg/kg (n = 20) as a single dose yielded 45% survival (P < 0.05 vs. control), whereas two doses provided only 30% survival (P < 0.05 vs. control; log rank test). Addition of more than two doses (i.e.; three or four doses) did not improve the outcome over that obtained with two doses (data not shown). These results suggest that the superiority of a single dose is independent of either the dose or the number of additional doses (two to four doses).
Efficacy of a single dose of reltecimod versus two doses, at 12 h intervals, in a lethal S. pyogenes thigh infection mouse model. BALB/c mice were infected IM in the left upper thigh with 1 × 107 CFU S. pyogenes (100 µL). Reltecimod (2.5 or 5 mg/kg) was administered by IV, at 1 h or at 1 h and 12 h post infection. Survival was monitored for 8 days. Mice injected with phosphate-buffered saline (saline-treated) served as controls (n = 20 for all groups). *P < 0.005 versus control, **P < 0.05 versus control, ***P = 0.0043 one versus two reltecimod doses; log rank test. Kaplan–Meier survival curve was created using GraphPad Prism
One Dose Versus Two Doses of Reltecimod: Effect of Extending the Dosing Interval
The effect of extending the time interval between the first and second reltecimod dose was tested. A single dose of reltecimod, 5 mg/kg at 1 h post infection (n = 20), was compared with the saline-treated controls or with two doses of reltecimod, 5 mg/kg each (n = 20), administered at 1 h and at 72 h post infection. Reltecimod administered at 1 h post infection resulted in 90% survival, as compared with 20% survival for saline-treated control animals (P < 0.0009) (Fig. 3). By comparison, administration of two doses of reltecimod at 1 h and at 72 h post infection resulted in 20% survival, which was similar to the survival rate in saline-treated control animals, and significantly lower than the survival rate following single dose treatment (P < 0.0011 vs. one dose). Even when the first dose of reltecimod was given at 5 h post infection, a single dose was superior (with 60% survival rate) to two doses, administered at 5 h and at 72 h post infection (with 40% survival rate; data not shown). These results suggest that the superiority of a single dose is independent of the interval between doses in this mouse model for lethal S. pyogenes infection.
Efficacy of a single dose of reltecimod versus two doses, at 72 h interval, in a lethal S. pyogenes thigh infection mouse model. BALB/c mice were infected IM in the left upper thigh with 1 × 107 CFU of GAS (100 µL). Reltecimod (5 mg/kg) was administered IV at 1 h, or at 1 h and 72 h post infection. Survival was monitored for 6 days. Mice injected with phosphate-buffered saline (saline-treated) served as controls (n = 20 for all groups). *P < 0.0009 (vs. control), **P < 0.0011 versus two dose. Kaplan–Meier survival curve was created using GraphPad Prism
Lethal E. coli Peritonitis Mouse Model
The ability of reltecimod to increase overall survival in the presence of a virulent, invasive gram-negative bacterial infection (E. coli serotype O18:K1, IP) was evaluated previously (Ramachandran et al. 2015). When reltecimod was administered by IV (5 mg/kg) at 4 h post infection, together with a suboptimal dose of the antibiotic cefepime (5 mg/kg IM at 4 h post infection, which reflects 25% of the effective dose), the overall survival reached 100%, as compared with 20% in either the group treated with saline alone or in a group treated with suboptimal cefepime alone (P < 0.001 vs. saline-treated or suboptimal antibiotic-treated infection controls).
Using the same model, the treatment benefit of a single administration of reltecimod, at 1.25 mg/kg (n = 20) or at the full effective dose of 5 mg/kg (n = 5), was compared against fractionating the full effective dose (5 mg/kg) into four equal portions of 1.25 mg/kg each, given at 12 h intervals between doses (n = 10). Control groups showed only 20% survival on day 7, with or without a suboptimal dose of cefepime (Fig. 4). Treatment with a low dose of reltecimod (1.25 mg/kg), in addition to suboptimal cefepime, showed some improvement in survival (40% survival), while treatment of mice with 5 mg/kg reltecimod, in addition to suboptimal cefepime, showed a dramatic and statistically significant improvement (100% survival; P < 0.05 vs. control). Fractionated, full effective dose (5 mg/kg), of four equal portions of 1.25 mg/kg each, was less protective, culminating in 70% survival (P < 0.05 between treatment groups receiving one and two doses).
Efficacy of a single dose of reltecimod versus fractionated doses, at 12 h intervals, in the lethal E. coli mouse infection model. A virulent, invasive strain of E. coli serotype O18:K1 was grown at 37 °C and, while at log-phase growth, was injected intraperitoneally to BALB/c mice, at 107 CFU. Saline (control infection), Cef alone (IM, at LD25), or reltecimod (5 mg/kg, 1.25 mg/kg, or 4 × 1.25 mg/kg) with Cef (at LD25) (IV and IM, respectively) was given at 1 h post infection or at 1, 12, 24, and 36 h post infection (4 × 1.25 mg/kg). Animal survival was monitored for 7 days. Cef = cefepime; LD = lethal dose. *P < 0.05 versus control, **P < 0.05 versus two fractionated doses. Kaplan–meier survival curve was created using GraphPad
Summary for Survival in All Lethal Models
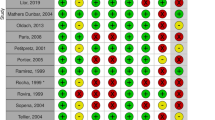
The dosing regimen (number of doses and interval between them) was investigated in the three infection models. In all cases, a single dose of reltecimod (administered at different time points post infection) was compared against several doses (two or four doses) that were given at varying intervals between them, ranging from 12 to 72 h. In addition, in all models, administration of a single, optimally effective dose of reltecimod was superior to two doses or fractionated doses. Importantly, in most cases, administration of two or multiple doses of reltecimod demonstrated beneficial effects as compared with saline-treated infection control animals. A summary of these comparisons is shown in Table 1. These results suggest that a single, fully effective dose of reltecimod, administered within a time window that still supports efficacy, is sufficient to provide survival benefit to animals following different bacterial infections regardless of the dose of reltecimod that was used, and that additional doses may be less favorable.
Cytokine/Chemokine and Leukocyte Profiles
To elucidate the possible processes underlying the reduced survival upon administration of two or multiple doses of reltecimod as compared with a single dose, we employed the CLP intra-abdominal polymicrobial infection model. The effect on the cytokine/chemokine response and on leukocyte profiles was examined and compared with each other (between one and two doses) and with the saline-treated control group at 24 and 48 h as illustrated in Fig. 5.
Experimental design. Mice received vehicle, a single IV dose of reltecimod (5 mg/kg), or two IV doses of reltecimod (5 mg/kg each, at 2 h and 24 h post CLP). Animals were euthanized at 24 h or 48 h after the CLP procedure. Plasma levels of various cytokines/chemokines and lymphocyte subsets were determined, as schematically illustrated. Sham animal values, at time 0, were used as baseline. Diagram was created using Microsoft PowerPoint
Cytokines and Chemokines
In order to characterize the effect of reltecimod on the systemic pro-inflammatory response elicited by the invasion of microbial pathogens into the bloodstream, the levels of several pro-inflammatory cytokines (interleukin 6 [IL-6], interleukin 3 [IL-3], interferon γ [IFN-γ], interleukin IL-1α [IL-1α]) and chemokines (monocyte chemoattractant protein 1 [MCP-1] and regulated on activation, normal T cell expressed and secreted [RANTES]) were determined in the plasma. The effect of one and two doses of reltecimod on the cytokine response following the CLP surgical procedure, after 24 and 48 h, was examined and compared with each other and with the saline-treated control group. Representative results are presented (Fig. 6).
Change over time in cytokine/chemokine levels for one or two doses of reltecimod versus control in the CLP lethal infection mouse model. Mice received a single IV dose of reltecimod (5 mg/kg, at 2 h post CLP), vehicle, or two IV doses of reltecimod (5 mg/kg each, at 2 h and 24 h post CLP). At 24 h or 48 h after CLP, animals were euthanized under anesthesia. Various cytokines/chemokines were determined using a multiplex immunoassay. The sham group served as baseline control. Representative cytokine/chemokine levels for the different treatment groups over time are presented as mean levels (pg/mL). *P = 0.053 (pANOVA). The graphs were constructed using group specific summary statistics. Kaplan–Meier survival curve was created using GraphPad Prism. Histograms were created using Microsoft Excel
Overall, a single dose of reltecimod (5 mg/kg) given 2 h post-surgery reduced the level of most cytokines/chemokines tested as compared with levels in the saline-treated control group at 24 h post administration, with further reduction in levels at 48 h (Fig. 6). Importantly, the cytokine levels were not ablated by reltecimod but, rather, were restored to a more homeostatic state.
Near statistical significance reduction (P = 0.053 vs. control) (Online Resource Table S1) was observed for median cytokine values of IL-6 achieved with a single dose of reltecimod versus control, using primary nonparametric analyses (or parametric comparison of natural log-transformed cytokine levels); Other cytokines demonstrated a similar trend, yet without statistical significance.
We next examined differences in cytokine median values between the group treated with two doses of reltecimod 5 mg/kg (at 2 h and 24 h post-surgery) and the saline-treated control group. Samples were evaluated at 48 h after the CLP procedure, which represented a lag time of 24 h between the second dose of reltecimod and the time of evaluation (Fig. 6). In general, median values for most of the cytokines/chemokines were higher in the group treated with two doses of reltecimod, as compared with the control group at 48 h, but no significant differences between the two groups were observed in nonparametric comparisons (or in parametric comparison of natural log-transformed cytokine levels, Online Resource Table S2).
Cytokine values at 48 h were compared between treatment with one and two doses of reltecimod (Online Resource Table S3a). The results showed that median values of IL-3, IL-6, MCP-1, IFN-γ, and RANTES (but not IL-1α) were lower in the single dose group than in the two-dose group, but the difference did not reach statistical significance. IL-6 and MCP-1, which are often measured in the blood following CLP and are nonspecific indicators of inflammation, showed the largest differences between the treatments (two- and threefold higher in the group treated with two doses of reltecimod versus the group treated with one dose of reltecimod, respectively).
Comparison of the median cytokine/chemokine levels for the two-dose reltecimod group evaluated at 48 h versus the levels for the single dose reltecimod group at 24 h (Online Resource Table S3b) revealed that the values were similar. The second dose of reltecimod (given at 2 and 24 h) appeared to attenuate or interrupt the process of reduction/normalization in cytokine/chemokine levels observed after 24 h with one dose. This resulted in elongation of the exposure to the cytokine/chemokine levels observed at 24 h for at least an additional 24 h. Consequently, two doses of reltecimod were inferior in terms of survival as compared with the one-dose treated group, yet the group treated with two doses showed better survival than the saline-treated, control group. Nevertheless, as with previous comparisons of cytokines/chemokines, we observed no statistically significant differences between the two conditions.
In summary, compared with the group treated with two doses of reltecimod, the single dose treatment group showed a lower level of pro-inflammatory cytokines (e.g., IL-6, IFN-γ) and a lower level of chemokines (e.g., MCP-1, which is known to be negatively correlated with the survival outcome) (Gao et al. 2012). These median levels correlated with survival results, where one dose consistently yielded greater survival than two doses. These observations suggest that the chain of events initiated after administration of one dose of reltecimod, which is essential for best efficacy, is interrupted when a second dose of reltecimod is administered at 24 h after the first dose.
Leukocyte Profile
An examination of the phenotypic changes in circulating lymphocyte subsets can be used to monitor the onset and progression of infectious diseases, including sepsis. To further characterize the effect of reltecimod on the processes occurring following polymicrobial abdominal infection, we determined the total number of cells and the levels (number and percentage) of different leukocyte subpopulations (CD4 + cells, CD8 + cells, B cells, T/B lymphocytes, macrophages/monocytes, and neutrophils) in plasma following the CLP surgical procedure. The effect of one and two doses of reltecimod on the leukocyte profiles following CLP after 24 and 48 h was compared for each group and for the saline-treated control group.
The effect on leukocyte profiles after the lethal CLP surgical procedure for the saline-treated control group was first compared with the sham-operated group at 24 and 48 h post infection (Online Resource Table S4).
At 24 h, total leukocyte cell count was reduced in sham-operated animals as compared to saline-treated control animals by approximately 17%. For leukocyte subpopulations, a decrease was observed for all subpopulations: (i) B-cell number and percentage by approximately 82% and 76%, respectively (ii) T/B lymphocyte number by approximately 13% (iii) macrophage/monocyte number by approximately 17% and (iv) neutrophil number and percentage by about 58% and 33%, respectively.
At 48 h, total cell count, B-cell count, and counts for T lymphocytes (number and percentage) showed further reductions, whereas neutrophils showed a substantial increase (4.4-fold). These results agreed with reports in the literature citing transient lymphopenia as often being followed by excess neutrophils in the circulation in sepsis (Hotchkiss et al. 2016; Venet et al. 2010; Zahorec 2001). Contrary to this transient lymphopenia, and in agreement with the literature, an increase in the T-cell subpopulation (CD4+ and CD8+ cells, percentage and number) was observed at 24 h (Hotchkiss et al. 2016; Roger et al. 2012), and returned to normal, or lower than normal median values, after 48 h.
A comparison of leukocyte profiles in the blood between the group receiving a single reltecimod dose and the saline-treated control group at 24 and 48 h following the lethal CLP surgical procedure is presented in Table 2 and Online Resource Table S5. Overall, reltecimod treatment resulted in a reduction in the number and percentage of various lymphocyte cell populations (except for neutrophils).
At 24 h, statistically significant differences for the control group versus the single dose reltecimod group were observed for multiple cell measures. The single dose reltecimod group had lower values for CD4+ count (P = 0.04); CD8+ percentage (P = 0.009) and count (P = 0.021); B-cell percentage (P = 0.012) count (P = 0.039); and for T/B lymphocyte percentage (P = 0.007) and count (P = 0.033). Conversely, the single dose reltecimod group had a higher percentage of neutrophils than did the control group or the sham-operated group (P = 0.006). There were no statistically significant differences in total cell measures or measures of macrophages/monocytes. Similar results were observed between nonparametric and parametric comparisons (with the exception of the percentage of CD4+ cells and the T/B lymphocyte count).
At 48 h, statistically significant differences between the single dose reltecimod group and the control group were observed for the number of total cells (P = 0.039), CD4+ cells (P = 0.025), CD8+ cells (P = 0.016), and T/B lymphocytes (P = 0.023). In each case, the number of cells observed in the single dose reltecimod group was lower than that seen in control animals.
These results agree with the suggested mechanism of action of reltecimod, as an antagonist of the costimulatory pathway, involving reduced levels of pro-inflammatory cytokines. The results also correlate with the improved survival results, where one dose was consistently associated with greater survival than were the two doses, and with better survival than in the saline-treated control groups. These observations suggest that the chain of events initiated after administration of one dose of reltecimod, which is essential for best efficacy, is interrupted when a second dose of reltecimod is administered at 24 h after the first dose.
Comparison of the leukocyte profile values between the control group and the group receiving two doses of reltecimod at the 48 h time point (Online Resource Table S6) showed no significant differences between the two groups (for any measures of percentage or overall cell counts). The percentages and counts of all analyzed cell populations (with the exception of the percentage of neutrophils) were higher in the two-dose reltecimod group as compared with the saline-treated control group. These observations are in contrast to the effect of reltecimod at 24 h, which yielded a reduction in the amount and percentages of analyzed cell populations. Taken together with the survival data and cytokine levels, these results lend additional support to the proposal that a second dose of reltecimod, as compared with only a single dose, further normalization is halted, and thus is not as beneficial as one dose.
Significant differences were observed between one dose of reltecimod and two doses of reltecimod at 48 h. In each instance, the group that was treated with two doses of reltecimod had a statistical significant higher median number of cells as compared with the group receiving only one dose (1.8- to 3.4-fold difference) including the count of total cells (P = 0.020), CD4+ cells (P = 0.012), CD8+ cells (P = 0.003), B cells (P = 0.016), and T/B lymphocytes (P = 0.012) (Online Resource Table S7). These values for two reltecimod doses were closer to the values observed for the sham group (Online Resource Table S6).
Although no significant differences in leukocyte percentages were observed for the effects of one dose versus two doses at 48 h, a consistent trend was apparent (Fig. 7). The percentage of CD4+ and CD8+ T-cell lymphocytes was reduced at 24 h and continued to decline at 48 h in the single dose group. By contrast, in the group treated with two doses of reltecimod, the levels at 48 h were similar to those at the 24 h time point. In a comparison of the leukocyte profiles for the two-dose group at 48 h versus the profile of the one-dose group at 24 h (Online Resource Table S8), it is apparent that the values are similar (with the exception of the neutrophil count, most likely due to the recruitment of neutrophils to the site of infection). The second dose of reltecimod (given at 24 h) attenuated the further reduced levels in the different cell populations observed after 24 h with one dose. This resulted in a prolonged presence of high levels of CD4+ and CD8+ T-cells in the animals for at least an additional 24 h. Consequently, the two-dose group showed better survival than the non-treated control group, although survival was inferior as compared with that for the one-dose treated group.
Leukocyte profiles over time in the CLP lethal infection mouse model for saline-treated control, one dose, and two doses of reltecimod. Mice received a single IV dose of reltecimod (5 mg/kg, at 2 h post CLP), vehicle, or two IV doses of reltecimod (5 mg/kg each, at 2 h and 24 h post CLP). At 24 or 48 h after CLP, animals were euthanized under anesthesia. Various lymphocyte subsets were determined using FACS analysis. The sham group served as baseline control. Results are presented for representative lymphocyte subsets as mean number of cells over time (three repeats). The graphs were constructed using group specific summary statistics. Histograms were created using Microsoft Excel
Cytokines/Chemokines and Leukocyte Profile Correlation
Correlations between cytokines/chemokines were analyzed as described in the Methods. At 24 h, the single dose reltecimod group showed multiple correlations of all cytokines/chemokines with one to six other cytokines/chemokines (data not shown). These results suggest that systemic changes in pro-inflammatory cytokines/chemokines occurred in the group treated with one dose of reltecimod at 24 h which were statistically significant and positively correlated to each other. This is again agrees with the suggested reltecimod role as an anti-inflammatory drug that works by attenuating CD28 signaling. These multiple, statistically significant correlations were observed to a lesser extent at 48 h. Similarly, in the two-dose reltecimod group, we observed significant correlation within six cytokines/chemokines at 48 h.
Correlation analysis was also used to examine the relationships between cytokine/chemokine and leukocyte profile measurements for the control group and the single dose reltecimod group at 24 h, collapsing across the control and the single dose treatment groups (Table 3). Results of this analysis showed significant positive correlations between cytokine/chemokine measures (excluding IL-1α) and the percentage of cell populations, including CD4+ cells, CD8+ cells, B cells, and T/B lymphocytes. Negative correlations were observed for both the number and percentage of neutrophils when significance was achieved. There was some evidence of stronger correlations with macrophage/monocyte measures in the single dose group than were observed overall. The correlations of IL-6, MCP-1, IFN-γ, and RANTES with lymphocyte profiling at 24 h for a single dose of reltecimod were no longer observed at 48 h. In the group that was treated with two doses of reltecimod, IL-1α and MCP-1 showed positive correlation with CD4+, CD8+, and T/B lymphocytes (for both the percentage and the number of cells). These correlations were not observed for the group treated with one dose of reltecimod.
Overall, these results showed that treatment with a single dose of reltecimod leads to multiple changes in both cytokine measures and lymphocyte profile, which are significantly correlated with each other, and can be detected after 24 h. The timing of the different events in the group treated with reltecimod is correlated up to 24 h after insult/treatment, after which it is no longer correlated.
Discussion
Using multiple animal models of infection, we evaluated the effect of the number of reltecimod doses and their timing with respect to survival, cytokines/chemokines measures, and blood leukocyte profiles. Overall, mice treated with a single IV dose of reltecimod (5 mg/kg) at 1–2 h after insult showed substantially greater survival, with an early (within 24 h) decrease in cytokines/chemokines levels and circulating leukocyte subpopulations (with the exception of neutrophils, which increased), as compared with saline-treated controls. An additional dose of reltecimod, at 24 h, did not improve these early positive effects and appeared to attenuate further changes. However, a second dose of reltecimod was beneficial for survival, as compared with survival in saline-treated controls.
Although in this study systemic events following treatment with reltecimod were monitored, we have previously shown (Barupal et al. 2019; Ramachandran et al. 2013) that the effects are paralleled with similar improvements in organs at the site of infection, as well as in remote organs; peritoneal fluid, liver, and kidney for CLP model and liver, kidney and thigh muscle, in case of thigh infection mouse model.
Infectious diseases are a consequence of both inadequate and exaggerated immune responses, where deleterious effects of pathogens can be caused by hyperstimulation and/or chronic activation of the host immune system. In the study presented here, a single dose of reltecimod (at 2 h post insult) attenuated the early release of pro-inflammatory cytokines/chemokines as compared with saline-treated controls (Fig. 6), consistent with its proposed mechanism of action in targeting CD28. With no additional doses of reltecimod, cytokine/chemokine levels in saline-treated controls and single dose treated animals were similar at 48 h. Survival, however, was markedly improved with a single reltecimod dose. Consequently, the total exposure to multiple cytokines for the single dose group was consistently lower than for the saline-treated control group.
These data may suggest that the early resolution or normalization (within 24 h) of multiple cytokine levels is correlated with improved survival 7 days later, and that early intervention after infection is critical for improved outcome. Based on in vitro data, we hypothesis that the long-term efficacy benefit of reltecimod might be based partially on its rapid intervention in signaling pathways, irrespective of its short residence time in plasma.
A second dose of reltecimod (at 24 h) resulted in sustained cytokine/chemokine levels that lasted beyond the 24 h time point until 48 h and was correlated with lower survival rates than seen in the one-dose treatment group. Consequently, the exposure to cytokines for representative cytokines/chemokines of animals that received two doses of reltecimod was higher than after one dose but lower than in control, saline-treated animals.
The observations reported here are consistent with a concept suggested by Xiao et al. (2011) and recently presented by Maier (2019) at the 2019 Annual Congress of the Society of Critical Care Medicine (Maier et al. 2019). They found that the magnitude and duration of dysregulated acute inflammatory response after severe trauma or burn injury in humans has a key role in determining clinical outcomes. Taking a transcriptomic approach, they suggested that the time required for expression of gene clusters to return to control values is a critical factor; specifically, a rapid return to baseline values is associated with uncomplicated outcomes, whereas persistence of high levels of inflammatory mediators is associated with complicated outcomes.
These observations suggest that reltecimod attenuates the massive, early release of cytokines/chemokines in response to lethal bacterial infection, and that survival is related to the total levels of the cytokines/chemokines during this early period. If translated to human exposure, this may imply a need for reduction (but not a total abrogation) in pro-inflammatory response in patients who suffer from severe infections as early as possible.
Subsequently, based on these animal studies, reltecimod is recommended for early administration, and this concept was implemented in Phase 2 (Bulger et al. 2014) and Phase 3 (ACCUTE, clinicaltrials.gov Identifier: NCT02469857) trials conducted in patients with NSTI and in the REACT trial in patients with acute kidney injury (AKI) (clinicaltrials.gov Identifier: NCT03403751).
The leukocyte profile data showed robust differences between treatment regimens. The majority of cell counts and percentages were significantly decreased for animals treated with a single dose of reltecimod, as compared with the values for saline-treated controls at 24 h. Neutrophils showed an expected significant increase possibly as a result of lower influx into affected organs and tissue. Data at 48 h were similar, with the single dose reltecimod group showing significantly lower cell counts (but not percentages) than both the saline-treated controls and the two-dose reltecimod group. Notably, at 48 h, there was no evidence for statistically significant differences between saline-treated controls and the group receiving two doses of reltecimod. The differences in CD4+ and CD8+ T-cell lymphocytes—numbers of which were reduced at 24 h and continued to decline at 48 h in the single dose reltecimod group versus the saline-treated control group—may be an indication of greater trafficking of lymphocytes out of the circulation and into extravascular tissue spaces (occurring during the first 24–48 h) in septic animals after treatment with one dose of reltecimod. This behavior is clearly observed with the analysis of the B cells when comparing sham and CLP control groups (Online Resource Table S4).
In correlation analyses, cytokines levels were generally positively correlated with one another, and with percentage measures of CD4+ cells, CD8+ cells, B cells, and T/B lymphocytes. Neutrophil percentages and counts were negatively correlated with cytokines levels, which is consistent with the elimination of neutrophils while cytokine levels are increased. The group treated with one dose of reltecimod showed more statistically significant correlations than did the group treated with two doses of reltecimod or the saline-treated control group. These correlations were more likely to be significant at 24 h than at 48 h. This observation emphasizes that the early events leading to improved survival are consistent with a more synchronized cytokine response and normalization of lymphocyte profile within 24 h.
Several potential explanations for the reduced efficacy of the second dose exist, and relate to toxicity and pharmacologic properties. Nevertheless, the reduced efficacy upon treatment with multiple doses of reltecimod was not likely due to toxic effects of reltecimod, based on repeat dose toxicology studies conducted in multiple animal models and based on the safety profile in healthy and NSTI human subject (Bulger et al. 2014).
In either healthy or inflammatory models (in pigs, minipigs, rabbits and mice), administration of reltecimod (up to 50 mg/kg) over 14 consecutive days or daily doses up to 8 weeks was not associated with any signs of toxicity. The no-observable-adverse-effect level (NOAEL) appeared to be greater than 50 mg/kg/day for all of these species.
Furthermore, the short half-life of the reltecimod peptide in the circulation (a few minutes) and the dose fractionation data, in the present study, argue against toxicity of reltecimod as an explanation for decreased survival when given as multiple doses: a single 5 mg/kg reltecimod dose was associated with significantly better survival than were two doses of 2.5 mg/kg (24 h apart), or four doses of 1.25 mg/kg (12 h apart).
These results corroborate those of clinical studies performed in human subjects. A Phase 1 clinical study (clinicaltrials.gov identifier: NCT01166984) identified no drug-related toxic effects in healthy subjects. A Phase 2a clinical study (clinicaltrials.gov Identifier: NCT01417780) established the safety of reltecimod in an NSTI patient population, with no drug-related adverse events reported and no significant difference between the treatment arms for adverse events (Bulger et al. 2014).
Another potential explanation for lower survival following subsequent doses, compared with the initial dose of reltecimod, is that the peptide dimerizes or forms a complex with proteins in plasma, such as albumin (Donate et al. 2008). In a study performed to explore potential aggregates and multimers of reltecimod drug product, the drug product was analyzed by both ultra-performance liquid chromatography (UPLC) and reversed-phase high-performance liquid chromatography (RP-HPLC), employing a gradient with a high organic content. No quantifiable peaks (≥0.1%) were observed in reltecimod drug product when examined using either method. These results indicate that no measurable levels of aggregates or multimers are formed under the experimental conditions of these two methods, and therefore dimerization and aggregation are most likely not the explanation.
While reltecimod has a short residence time in the plasma, bacterial infections, especially in sepsis, persist for long periods of time. Therefore, the results obtained, showing a single dose of reltecimod to be sufficient and superior to two doses in providing a survival benefit, sustained for 7 days post infection, were surprising. Other drugs with a single dose regimen are usually drugs with either (i) an extended elimination half-life or (ii) sustained release into the bloodstream, or both. Sustained release allows the drug to be administered in shortened regimens while maintaining therapeutic efficacy over a wide range of infections. For example, Azithromycin, an antibiotic with additional immunomodulatory effects that is useful for the treatment of a number of bacterial infections, has an elimination half-life of more than 60 h and sustained release into the bloodstream (Rothermel 2003; Dunn and Barradell 1996; Guay 2003). Another example is Xofluza (generic name—baloxavir marboxil), the first FDA-approved drug to treat influenza in 20 years (McNeil 2018), is administered in a single dose regimen. The drug, which is a selective inhibitor of influenza cap-dependent endonuclease, shortens flu symptoms, and is expected to work against drug-resistant strains (Omoto et al. 2018). Further studies to address the duration of effect of reltecimod are ongoing.
Conclusions
In conclusion, we have shown that a single dose of reltecimod dramatically improved survival in three different models of infection, and that the early events, including reduced exposure to high levels of cytokines/chemokines and normalization of leukocyte profiles, precede the dramatic improvement in survival. Multiple-dose strategies do not improve survival, and in fact appear to impede beneficial processes that occur following the first dose. These results support the early administration of a single dose of reltecimod in on-going clinical trials involving patients with NSTI and AKI.
Data Availability
The data that support the findings of this study are available from the corresponding author, but restrictions apply to the availability of these data, which are under Atox Bio Ltd license, and so are not publicly available. Data are however available from the corresponding author upon reasonable request and with permission of Atox Bio Ltd.
Abbreviations
- CLP:
-
Cecal ligation and puncture
- FACS:
-
Fluorescent automated cell sorter
- IFN-γ:
-
Interferon γ
- IL:
-
Interleukin
- IM:
-
Intramuscularly
- IP:
-
Intraperitoneal
- LPS:
-
Lipopolysaccharide
- MCP-1:
-
Monocyte chemoattractant protein 1
- NOAEL:
-
No-observable-adverse-effect level
- PBS:
-
Phosphate-buffered saline
- RP-HPLC:
-
Reversed-phase high-performance liquid chromatography
- SEB:
-
Staphylococcal enterotoxin B
- TNF-α:
-
Tumor necrosis factor α
- UPLC:
-
Ultra-performance liquid chromatography
References
Annane D, Bellissant E, Bollaert PE, Briegel J, Confalonieri M, De Gaudio R, Keh D, Kupfer Y, Oppert M, Meduri GU (2009) Corticosteroids in the treatment of severe sepsis and septic shock in adults: a systematic review. JAMA 301(22):2362–2375. https://doi.org/10.1001/jama.2009.815
Arad G, Levy R, Nasie I, Hillman D, Rotfogel Z, Barash U, Supper E, Shpilka T, Minis A, Kaempfer R (2011) Binding of superantigen toxins into the CD28 homodimer interface is essential for induction of cytokine genes that mediate lethal shock. PLoS Biol 9(9):1001149. https://doi.org/10.1371/journal.pbio.1001149
Barupal SR, Soni ML, Barupal R (2019) Factors affecting mortality following necrotizing soft-tissue infections: randomized prospective study. J Emerg Trauma Shock 12(2):108–116. https://doi.org/10.4103/JETS.JETS_17_18
Brosnahan AJ, Schlievert PM (2011) Gram-positive bacterial superantigen outside-in signaling causes toxic shock syndrome. FEBS J 278(23):4649–4667. https://doi.org/10.1111/j.1742-4658.2011.08151.x
Bulger EM, Maier RV, Sperry J, Joshi M, Henry S, Moore FA, Moldawer LL, Demetriades D, Talving P, Schreiber M, Ham B, Cohen M, Opal S, Segalovich I, Maislin G, Kaempfer R, Shirvan A (2014) A Novel drug for treatment of necrotizing soft-tissue infections: a randomized clinical trial. JAMA Surg 149(6):528–536. https://doi.org/10.1001/jamasurg.2013.4841
Cohen J (2002) The immunopathogenesis of sepsis. Nature 420(6917):885–891. https://doi.org/10.1038/nature01326
Collins AV, Brodie DW, Gilbert RJ, Iaboni A, Manso-Sancho R, Walse B, Stuart DI, van der Merwe PA, Davis SJ (2002) The interaction properties of costimulatory molecules revisited. Immunity 17:201–210. https://doi.org/10.1016/S1074-7613(02)00362-X
Cross AS, Opal SM, Sadoff JC, Gemski P (1993) Choice of bacteria in animal models of sepsis. Infect Immun 61(7):2741–2747
Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R et al (2008) Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock. Crit Care Med 36(1):296–327. https://doi.org/10.1097/01.CCM.0000298158.12101.41
Donate F, Parry GC, Shaked Y, Hensley H, Guan X, Beck I, Tel-Tsur Z, Plunkett ML, Manuia M, Shaw DE, Kerbel RS, Mazar AP (2008) Pharmacology of the novel antiangiogenic peptide ATN-161 (Ac-PHSCN-NH2): observation of a U-shaped dose-response curve in several preclinical models of angiogenesis and tumor growth. Clin Cancer Res 14(7):2137–2144. https://doi.org/10.1158/1078-0432.CCR-07-4530
Dunn CJ, Barradell LB (1996) Azithromycin: A review of its pharmacological properties and use as 3-day therapy in respiratory tract infections. Drugs 51(3):483–505. https://doi.org/10.2165/00003495-199651030-00013
Evans EJ, Esnouf RM, Manso-Sancho R, Gilbert RJ, James JR, Yu C, Fennelly JA, Vowles C, Hanke T, Walse B, Hünig T, Sørensen P, Stuart DI, Davis SJ (2005) Crystal structure of a soluble CD28-Fab complex. Nat Immunol 6:271–279. https://doi.org/10.1038/ni1170
Gao M, Zhang L, Liu Y, Yang M, Wang N, Wang K, Ou D, Liu M, Chen G, Liu K, Xiao X (2012) Use of blood urea nitrogen, creatinine, interleukin-6, granulocyte-macrophage colony stimulating factor in combination to predict the severity and outcome of abdominal sepsis in rats. Inflamm Res 61(8):889–897. https://doi.org/10.1007/s00011-012-0481-3
Guay D (2003) Short-course antimicrobial therapy of respiratory tract infections. Drugs 63(20):2169–2184. https://doi.org/10.2165/00003495-200363200-00002
Hotchkiss RS, Moldawer LL, Opal SM, Reinhart K, Turnbull IR, Vincent JL (2016) Sepsis and septic shock. Nat Rev Dis Primers 2:16045. https://doi.org/10.1038/nrdp.2016.45
Johansson L, Thulin P, Low DE, Norrby-Teglund A (2010) Getting under the skin: the immunopathogenesis of Streptococcus pyogenes deep tissue infections. Clin Infect Dis 51(1):58–65. https://doi.org/10.1086/653116
Kaempfer R, Popugailo A, Levy R, Arad G, Hillman D, Rotfogel Z (2017) Bacterial superantigen toxins induce a lethal cytokine storm by enhancing B7–2/CD28 costimulatory receptor engagement, a critical immune checkpoint. Receptor Clin Invest 4(1): 1500. https://doi.org/10.14800/rci.1500
Levy R, Rotfogel Z, Hillman D, Popugailo A, Arad G, Supper E, Osman F, Kaempfer R (2016) Superantigens hyperinduce inflammatory cytokines by enhancing the b7–2/cd28 costimulatory receptor interaction. Proc Natl Acad Sci USA 113:E6437–E6446. https://doi.org/10.1073/pnas.1603321113
Maier RV (2019) Response to injury and stress: a genomic storm [video] https://www.youtube.com/watch?v=SaLUNU-KW10. Accessed 1 March 2019
McNeil D (2018) F.D.A approves new drug for flu. New York Times, 24 Oct 2018
Mirzoeva S, Paunesku T, Wanzer MB, Shirvan A, Kaempfer R, Woloschak GE, Small W Jr (2014) Single administration of p2TA (AB103), a CD28 antagonist peptide, prevents inflammatory and thrombotic reactions and protects against gastrointestinal injury in total-body irradiated mice. PLoS ONE 9(7):e101161. https://doi.org/10.1371/journal.pone.0101161
Napolitano LM (2018) Sepsis 2018: definitions and guideline changes. Surg Infect 19(2):117–125. https://doi.org/10.1089/sur.2017.278
Omoto S, Speranzini V, Hashimoto T, Noshi T, Yamaguchi H, Kawai M, Kawaguchi K, Uehara T, Shishido T, Naito A, Cusack S (2018) Characterization of influenza virus variants induced by treatment with the endonuclease inhibitor baloxavir marboxil. Sci Rep 8(1):9633. https://doi.org/10.1038/s41598-018-27890-4
Opal SM, Palardy JE, Chen WH, Parejo NA, Bhattacharjee AK, Cross AS (2005) Active immunization with a detoxified endotoxin vaccine protects against lethal polymicrobial sepsis: its use with CpG adjuvant and potential mechanisms. J Infect Dis 192(12):2074–2080. https://doi.org/10.1086/498167
Ramachandran G, Kaempfer R, Chung CS, Shirvan A, Chahin AB, Palardy JE, Chen Y, Whitford M, Arad G, Hillman D, hemesh R, Blackwelder W, Ayala A, Cross AS, Opal SM (2015) CD28 homodimer interface mimetic peptide acts as a preventive and therapeutic agent in models of severe bacterial sepsis and gram-negative bacterial peritonitis. J Infect Dis 211(6):995–1003. https://doi.org/10.1093/infdis/jiu556
Ramachandran G, Tulapurkar ME, Harris KM, Arad G, Shirvan A, Shemesh R, Detolla LJ, Benazzi C, Opal SM, Kaempfer R, Cross AS (2013) A peptide antagonist of CD28 signaling attenuates toxic shock and necrotizing soft-tissue infection induced by Streptococcus pyogenes. J Infect Dis 207(12):1869–1877. https://doi.org/10.1093/infdis/jit104
Roger PM, Hyvernat H, Ticchioni M, Kumar G, Dellamonica J, Bernardin G (2012) The early phase of human sepsis is characterized by a combination of apoptosis and proliferation of T cells. J Crit Care 27(4):384–393. https://doi.org/10.1016/j.jcrc.2012.04.010
Rothermel CD (2003) Single dose azithromycin for acute otitis media: a pharmacokinetic/pharmacodynamic rationale. Curr Ther Res Clin Exp 64(Suppl 1):4–15. https://doi.org/10.1016/j.curtheres.2003.09.004
Shirvan A, Bulger E, Danker W (2018) Reltecimod. T-cell-specific surface glycoprotein CD28 (TP44) antagonist, CD28 homodimer interface mimetic peptide, treatment of necrotizing soft-tissue infection. Drugs Future 43(4):243–259. https://doi.org/10.1358/dof.2018.043.04.2772182
Sriskandan S, Moyes D, Buttery LK, Krausz T, Evans TJ, Polak J, Cohen J (1996) Streptococcal pyrogenic exotoxin A release, distribution, and role in a murine model of fasciitis and multiorgan failure due to Streptococcus pyogenes. J Infect Dis 173(6):1399–1407
Venet F, Davin F, Guignant C, Larue A, Cazalis MA, Darbon R, Allombert C, Mougin B, Malcus C, Poitevin-Later F, Lepape A, Monneret G (2010) Early assessment of leukocyte alterations at diagnosis of septic shock. Shock 34(4):358–363. https://doi.org/10.1097/SHK.0b013e3181dc0977
Xiao W, Mindrinos MN, Seok J, Cuschieri J, Cuenca AG, Gao H, Hayden DL, Hennessy L, Moore EE, Minei JP, Bankey PE, Johnson JL, Sperry J, Nathens AB, Billiar TR, West MA, Brownstein BH, Mason PH, Baker HV, Finnerty CC, Jeschke MG, López MC, Klein MB, Gamelli RL, Gibran NS, Arnoldo B, Xu W, Zhang Y, Calvano SE, McDonald-Smith GP, Schoenfeld DA, Storey JD, Cobb JP, Warren HS, Moldawer LL, Herndon DN, Lowry SF, Maier RV, Davis RW, Tompkins RG (2011) Inflammation and host response to injury large-scale collaborative research program, a genomic storm in critically injured humans. J Exp Med 208:2581–2590. https://doi.org/10.1084/jem.20111354
Zahorec R (2001) Ratio of neutrophil to lymphocyte counts–rapid and simple parameter of systemic inflammation and stress in critically ill. Bratisl Lek Listy 102(1):5–14
Acknowledgements
This study was supported by Atox Bio (to RK, SMO, AC and GM). We would like to thank Tsufit Gross for critically reviewing the manuscript.
Funding
This study was supported by Atox Bio (to RK, SMO, AC and GM).
Author information
Authors and Affiliations
Contributions
Concept and design of the study: SMO, AC, MLT, CF, RE, and AS contributed. RE wrote the first draft of the manuscript. Acquisition of data: SMO, AC, MLT, CF. Analysis and interpretation of data: SMO, AC, MLT, CF, GM, RE, and AS. Critical revision of the manuscript for important intellectual content: SMO, AC, MLT, RK, CF, RE, and AS. Study supervision: SMO, AC, RE, and AS.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. AS and RE are employees of Atox Bio. RK, AC, GM and SMO have received funding from Atox Bio. MLT, and CF have no relevant financial relationships to disclose.
Ethics Approval
All animal studies were approved by the Brown University/Rhode Island Hospital and University of Maryland Institutional Animal Care and Use Committees (IACUCs) before experiments were initiated. Animals were housed in an IACUC-approved facility under biosafety level 2 safety conditions and were monitored by Brown University/Rhode Island Hospital and University of Maryland veterinary staffs.
Informed Consent
Not Applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Edgar, R., Tarrio, M.L., Maislin, G. et al. Treatment with One Dose of Reltecimod is Superior to Two Doses in Mouse Models of Lethal Infection. Int J Pept Res Ther 26, 1669–1683 (2020). https://doi.org/10.1007/s10989-019-09974-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10989-019-09974-5