Abstract
Purpose
This study aimed to validate whether the recently-proposed prognostic grading system, initial brain metastasis velocity (iBMV), is applicable to breast cancer patients receiving stereotactic radiosurgery (SRS). We focused particularly on whether this grading system is useful for patients with all molecular types, i.e., positive versus negative for EsR, PgR and HER2.
Methods and materials
This was an institutional review board-approved, retrospective cohort study using our database, prospectively accumulated at three gamma knife institutes, during the 20-year-period since 1998. We excluded patients for whom the day of primary cancer diagnosis was not available, had synchronous presentation, lacked information regarding molecular types, and/or had received pre-SRS radiotherapy and/or surgery. We ultimately studied 511 patients categorized into two classes by iBMV scores, i.e., < 2.00 and ≥ 2.00.
Results
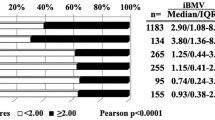
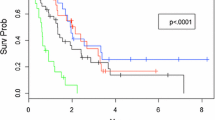
The median iBMV score for the entire cohort was 0.97 (IQR 0.39–2.84). Median survival time (MST) in patients with iBMV < 2.00, 15.9 (95% CI 13.0–18.6, IQR 7.5–35.5) months, was significantly longer than that in patients with iBMV ≥ 2.00, 8.2 (95% CI 6.8–9.9, IQR 3.9–19.4) months (HR 1.582, 95% CI: 1.308–1.915, p < 0.0001). The same results were obtained in patients with EsR (−), PgR (−), HER2 (+) and HER2 (−) cancers, while MSTs did not differ significantly between iBMV < 2.00 vs ≥ 2.00 in patients with EsR (+) and PgR (+) cancers.
Conclusions
This system was clearly shown to be applicable to breast cancer patients with SRS-treated BMs. However, this system is not applicable to patients with hormone receptor (+) breast cancer.





Similar content being viewed by others
References
Soike MH, McTyre ER, Hughes RT et al (2018) Initial brain metastasis velocity: does the rate at which cancers first seed the brain affect outcomes? J Neurooncol 139:461–467. https://doi.org/10.1007/s11060-018-2888-3
Yamamoto M, Aiyama H, Koiso T et al (2019) Applicability and limitation of a recently-proposed prognostic grading metric, initial brain metastasis velocity, for brain metastasis patients undergoing stereotactic radiosurgery. J Neuro-Oncol 143:613–621. https://doi.org/10.1007/s11060-019-03199-8
Schouten LJ, Rutten J, Huveneers HA, Twijnstra A (2002) Incidence of brain metastases in a cohort of patients with carcinoma of the breast, colon, kidney, and lung and melanoma. Cancer 94:2698–2705. https://doi.org/10.1002/cncr.10541
Yamamoto M, Kawabe T, Sato Y et al (2013) A case-matched study of stereotactic radiosurgery for patients with multiple brain metastases: comparing treatment results for 1–4 vs ≥ 5 tumors. J Neurosurg 118:1258–1268. https://doi.org/10.3171/2013.3.JNS121900
Yamamoto M, Sato Y, Serizawa T et al (2012) Subclassification of recursive partitioning analysis class II patients with brain metastases treated radiosurgically. Int J Radiat Oncol Biol Phys 83:1399–1405. https://doi.org/10.1016/j.ijrobp.2011.10.018
Yamamoto M, Serizawa T, Sato Y et al (2013) Validity of two recently-proposed prognostic grading indices for lung, gastro-intestinal, breast and renal cell cancer patients with radiosurgically-treated brain metastases. J Neurooncol 111:327–335. https://doi.org/10.1007/s11060-012-1019-9
Yamamoto M, Serizawa T, Shuto T et al (2014) Stereotactic radiosurgery for patients with multiple brain metastases (JLGK0901): a multi-institutional prospective observational study. Lancet Oncol 15:387–395. https://doi.org/10.1016/S1470-2045(14)70061-0
Zafir-Lavie I, Sherbo S, Goltsman H et al (2018) Successful intracranial delivery of trastuzumab by gene-therapy for treatment of HER2-positive breast cancer brain metastases. J Control Release 291:80–89. https://doi.org/10.1016/j.jconrel.2018.10.017
Rostami R, Mittal S, Rostami P, Tavassoli F, Jabbari B (2016) Brain metastasis in breast cancer: a comprehensive literature review. J Neurooncol 127:407–414. https://doi.org/10.1007/s11060-016-2075-3
Miller JA, Kotecha R, Ahluwalia MS et al (2017) Overall survival and the response to radiotherapy among molecular subtypes of breast cancer brain metastases treated with targeted therapies. Cancer 123:2283–2293. https://doi.org/10.1002/cncr.30616
Grubb CS, Jani A, Cheng-Chia Wu CC et al (2016) Breast cancer subtype as a predictor for outcomes and control in the setting of brain metastases treated with stereotactic radiosurgery. J Neurooncol 127:103–110. https://doi.org/10.1007/s11060-015-2014-8
Leyland-Jones B (2009) (2009) Human epidermal growth factor receptor 2-positive breast cancer and central nervous system metastases. J Clin Oncol 27:5278–5286. https://doi.org/10.1200/JCO.2008.19.8481
Tonyali O, Coskun U, Yuksel S et al (2016) Risk factors for brain metastasis as a first site of disease recurrence in patients with HER2 positive early stage breast cancer treated with adjuvant trastuzumab. Breast 25:22–26. https://doi.org/10.1016/j.breast.2015.11.006
Palmieri D, Bronder JL, Herring JM et al (2007) (2007) Her-2 overexpression increases the metastatic outgrowth of breast cancer cells in the brain. Cancer Res 67:4190–4198. https://doi.org/10.1158/0008-5472.CAN-06-3316
Sperduto PW, Chao ST, Sneed PK et al (2010) Diagnosis-specific prognostic factors, indexes, and treatment outcomes for patients with newly diagnosed brain metastases: a multi-institutional analysis of 4,259 patients. Int J Radiat Oncol Biol Phys 77:655–661. https://doi.org/10.1016/j.ijrobp.2009.08.025
Sperduto PW, Kased N, Roberge D et al (2012) The effect of tumor subtype on survival and the graded prognostic assessment (GPA) for patients with breast cancer and brain metastases. Int J Radiat Oncol Biol Phys 82:2111–2117. https://doi.org/10.1016/j.ijrobp.2011.02.027
Yamamoto M, Kawabe T, Higuchi Y et al (2012) Validity of three recently proposed prognostic grading indexes for breast cancer patients with radiosurgically treated brain metastases. Int J Radiat Oncol Biol Phys 8:1110–1115. https://doi.org/10.1016/j.ijrobp.2012.02.040
Funding
The authors have no sources of financial and/or material support to declare.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No actual or potential conflicts of interest exist.
Informed consent
Written informed consent was obtained from all patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yamamoto, M., Serizawa, T., Nagano, O. et al. Three-institution study on applicability of initial brain metastasis velocity for breast cancer brain metastasis patients undergoing stereotactic radiosurgery. J Neurooncol 147, 177–184 (2020). https://doi.org/10.1007/s11060-020-03412-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-020-03412-z