Abstract
Objectives
To assess the prevalence of dental implant-related perforations of relevant anatomical structures and inadequate spacing between the implant and the adjacent tooth or implant, and their association with anatomical location, implant dimension, thread exposure, and presence of graft, using cone beam computed tomography (CBCT).
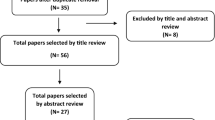
Materials and methods
CBCT scans of patients with implants were retrospectively assessed regarding the presence of implant-related perforation of adjacent anatomical structures, and inadequate mesial and distal spacing between the implant and the adjacent tooth/implant (i.e., < 1 mm or < 3 mm, respectively). Implants were classified according to anatomical location, dimensions, thread exposure, and the presence of graft (i.e., bone graft or bone substitutes). Prevalence of perforations and inadequate spacing was compared among the different implant classifications (Chi-squared test). Significance level was set at 5%.
Results
A total of 1109 implants were assessed, out of which 369 (33.3%) presented perforation of adjacent structures. Prevalence of perforations in the maxilla (43.5%) was higher than in the mandible (11.3%). Inadequate spacing was found in 18.2% of the mesial and distal measurements, which was more prevalent in the maxilla (p < 0.001). Implants perforating adjacent structures or placed with inadequate spacing presented higher prevalence of thread exposure (p < 0.001). No significant difference was found between the presence of perforations or inadequate spacing and presence of graft (p > 0.05).
Conclusions
Implant-related perforations of relevant anatomical structures and inadequate spacing between the implant and the adjacent tooth/implant are relatively prevalent and more common in the maxilla. Both are associated with threads exposure.
Clinical relevance
Information on dental implant-related perforations and inadequate spacing can assist dental surgeons in pre-surgical planning.



Similar content being viewed by others
References
de Groot RJ, Oomens MAEM, Forouzanfar T, Schulten EAJM (2018) Bone augmentation followed by implant surgery in the edentulous mandible: a systematic review. J Oral Rehabil 45:334–343. https://doi.org/10.1111/joor.12605
Sánchez Garcés MA, Escoda-Francolí J, Gay-Escoda C (2011) Implant complications. Implant Dent 9:1–37. https://doi.org/10.5772/19706
Morton D, Gallucci G, Bjarni WL et al (2018) Group 2 ITI consensus report: prosthodontics and implant dentistry. Clin Oral Implants Res 29:215–223. https://doi.org/10.1111/clr.13298
Jung RE, Nawas B Al, Araujo M, et al (2018) Group 1 ITI consensus report: the influence of implant length and design and medications on clinical and patient- reported outcomes. Clin Oral Implants Res 29:69–77 . doi: https://doi.org/10.1111/clr.13342
Misch K, Wang H-L (2008) Implant surgery complications: etiology and treatment. Implant Dent 17:159–168. https://doi.org/10.1097/ID.0b013e3181752f61
Ng K, Fan M, Leung M et al (2018) Peri-implant inflammation and marginal bone level changes around dental implants in relation to proximity with and bone level of adjacent teeth. Aust Dent J 63:467–477. https://doi.org/10.1111/adj.12650
Ramanauskaite A, Roccuzzo A, Schwarz F (2018) A systematic review on the influence of the horizontal distance between two adjacent implants inserted in the anterior maxilla on the inter-implant mucosa fill. Clin Oral Implants Res 29:62–70. https://doi.org/10.1111/clr.13103
Clark D, Barbu H, Lorean A, Mijiritsky E, Levin L (2017) Incidental findings of implant complications on postimplantation CBCTs: a cross-sectional study. Clin Implant Dent Relat Res 19:776–782. https://doi.org/10.1111/cid.12511
Tyndall DA, Price JB, Tetradis S, Ganz SD, Hildebolt C, Scarfe WC, American Academy of Oral and Maxillofacial Radiology (2012) Position statement of the American Academy of oral and maxillofacial radiology on selection criteria for the use of radiology in dental implantology with emphasis on cone beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol 113:817–826. https://doi.org/10.1016/j.oooo.2012.03.005
Jacobs R, Salmon B, Codari M, Hassan B, Bornstein MM (2018) Cone beam computed tomography in implant dentistry: recommendations for clinical use. BMC Oral Health 18:88. https://doi.org/10.1186/s12903-018-0523-5
Harris D, Benic GI, Bornstein MM (2012) E . A . O . Guidelines for the use of diagnostic imaging in implant dentistry 2011 . A consensus workshop organized by the European Association for Osseointegration at the Medical University of Warsaw. Clin Oral Implants Res 1243–1253 . doi: https://doi.org/10.1111/j.1600-0501.2012.02441.x
Al-Johany SS, Al Amri MD, Alsaeed S, Alalola B (2017) Dental implant length and diameter: a proposed classification scheme. J Prosthodont 26:252–260. https://doi.org/10.1111/jopr.12517
Starch-Jensen T, Jensen JD (2017) Maxillary sinus floor augmentation: a review of selected treatment modalities. J Oral Maxillofac Res 8:1–13. https://doi.org/10.5037/jomr.2017.8303
Al-Moraissi E, Elsharkawy A, Abotaleb B et al (2018) Does intraoperative perforation of Schneiderian membrane during sinus lift surgery causes an increased the risk of implants failure?: a systematic review and meta regression analysis. Clin Implant Dent Relat Res 20:882–889. https://doi.org/10.1111/cid.12660
Misch CE, Resnik R (2010) Mandibular nerve neurosensory impairment after dental implant surgery: management and protocol. Implant Dent 19:378–386. https://doi.org/10.1097/ID.0b013e3181effa92
de Mello JS, Faot F, Correa G, Chagas Júnior OL (2017) Success rate and complications associated with dental implants in the incisive canal region: a systematic review. Int J Oral Maxillofac Surg 46:1584–1591. https://doi.org/10.1016/j.ijom.2017.05.002
Arruda JA, Silva P, Silva L et al (2017) Dental implant in the canalis sinuosus: a case report and review of the literature. Case Rep Dent 2017:1–5. https://doi.org/10.1155/2017/4810123
Wolff J, Karagozoglu KH, Bretschneider JH, Forouzanfar T, Schulten EA (2016) Altered nasal airflow: an unusual complication following implant surgery in the anterior maxilla. Int J Implant Dent 2:6. https://doi.org/10.1186/s40729-016-0045-3
de-Azevedo-Vaz SL, Peyneau PD, Ramirez-Sotelo LR, et al (2016) Efficacy of a cone beam computed tomography metal artifact reduction algorithm for the detection of peri-implant fenestrations and dehiscences. Oral Surg Oral Med Oral Pathol Oral Radiol 121:550–556 . doi: https://doi.org/10.1016/j.oooo.2016.01.013
Law C, Alam P, Borumandi F (2017) Floor-of-mouth hematoma following dental implant placement: literature review and case presentation. J Oral Maxillofac Surg 75:2340–2346. https://doi.org/10.1016/j.joms.2017.07.152
Kumar S, Shah A, Thukral R, Prasant MC, Sadrani SM, Baxi H (2016) Assessment of various risk factors for success of delayed and immediate loaded dental implants: a retrospective analysis. J Contemp Dent Pract 17:853–856. https://doi.org/10.5005/jp-journals-10024-1943
Chrcanovic BR, Albrektsson T, Wennerberg A (2014) Reasons for failures of oral implants. J Oral Rehabil 41:443–476. https://doi.org/10.1111/joor.12157
Javed F, Romanos GE (2015) Role of implant diameter on long-term survival of dental implants placed in posterior maxilla: a systematic review. Clin Oral Investig 19:1–10. https://doi.org/10.1007/s00784-014-1333-z
Tolentino da Rosa de Souza P, Binhame Albini Martini M, Reis Azevedo-Alanis L (2018) Do short implants have similar survival rates compared to standard implants in posterior single crown?: a systematic review and meta-analysis. Clin Implant Dent Relat Res 20:890–901. https://doi.org/10.1111/cid.12634
Tarnow DP, Cho SC, Wallace SS (2000) The effect of inter-implant distance on the height of inter-implant bone crest. J Periodontol 71:546–549. https://doi.org/10.1902/jop.2000.71.4.546
Elian N, Bloom M, Dard M, Cho SC, Trushkowsky RD, Tarnow D (2011) Effect of interimplant distance (2 and 3 mm) on the height of interimplant bone crest: a histomorphometric evaluation. J Periodontol 82:1749–1756. https://doi.org/10.1902/jop.2011.100661
Wismeijer D, Joda T, Flügge T, Fokas G, Tahmaseb A, Bechelli D, Bohner L, Bornstein M, Burgoyne A, Caram S, Carmichael R, Chen CY, Coucke W, Derksen W, Donos N, el Kholy K, Evans C, Fehmer V, Fickl S, Fragola G, Gimenez Gonzales B, Gholami H, Hashim D, Hui Y, Kökat A, Vazouras K, Kühl S, Lanis A, Leesungbok R, Meer J, Liu Z, Sato T, de Souza A, Scarfe WC, Tosta M, Zyl P, Vach K, Vaughn V, Vucetic M, Wang P, Wen B, Wu V (2018) Group 5 ITI consensus report : digital technologies. Clin Oral Implants Res 29:436–442. https://doi.org/10.1111/clr.13309
Funding
This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior-Brasil (CAPES)-Finance Code 001.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was carried out after local Institutional Review Board approval (protocol no. 91544518.3.0000.5418).
Informed consent
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gaêta-Araujo, H., Oliveira-Santos, N., Mancini, A.X.M. et al. Retrospective assessment of dental implant-related perforations of relevant anatomical structures and inadequate spacing between implants/teeth using cone-beam computed tomography. Clin Oral Invest 24, 3281–3288 (2020). https://doi.org/10.1007/s00784-020-03205-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-020-03205-8