Abstract
Purpose
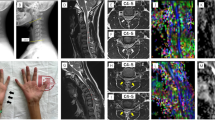
Patients with Hirayama disease (HD) present with a larger range of neck flexion and show signs of cervical spine instability. Cervical spine stability largely relies on cervical spine muscles. The purpose of this study was to compare the cross-sectional areas (CSAs) of cervical spine muscles between patients with HD and healthy controls, providing some insights into whether there is cervical spine muscle weakness and incongruence in HD patients.
Methods
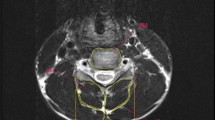
In this retrospective study, cervical spine muscles CSAs of 44 HD patients, as well as that of 44 age- and sex-matched healthy counterparts, were measured on the T2-weighted axial MR images. The ratios of cervical spine muscles CSA to the corresponding vertebral body areas, defined as R-CSAs, and the flexor/extensor CSA ratios were computed and compared between two groups.
Results
Compared with healthy counterparts, R-CSAs of total cervical spine muscles, total extensors, superficial extensors, and deep flexors were significantly lower in HD patients. HD patients also demonstrated a significantly greater superficial flexor/superficial extensor CSA ratio than the healthy counterparts, indicating a mismatch between superficial flexors CSA and superficial extensors CSA in HD patients.
Conclusions
In this pioneering study, HD patients had decreased size in most cervical spine muscles and a mismatch between CSAs of superficial flexor and that of superficial extensors. These results indicate generalized weakness and incongruence of cervical spine muscles, which may predispose cervical spine of HD patients to a less stable situation.
Graphic abstract
These slides can be retrieved under Electronic Supplementary Material.


Similar content being viewed by others
Abbreviations
- BMI:
-
Body mass index
- CSA:
-
Cross-sectional area
- DEs:
-
Deep extensors
- DFs:
-
Deep flexors
- HD:
-
Hirayama disease
- MRI:
-
Magnetic resonance imagine
- R-CSA:
-
Relative cross-sectional area
- ROI:
-
Region of interest
- SEs:
-
Superficial extensors
- SF:
-
Superficial flexor
- TEs:
-
Total extensors
- TFs:
-
Total flexors
- TCMs:
-
Total cervical spine muscles
- VBA:
-
Vertebral body area
References
Hirayama K, Tokumaru Y (2000) Cervical dural sac and spinal cord in juvenile muscular atrophy of distal upper extremity. Neurology 54:1922–1926
Tashiro K, Kikuchi S, Itoyama Y et al (2006) Nationwide survey of juvenile muscular atrophy of distal upper extremity (Hirayama disease) in Japan. Amyotroph Lateral Scler 7:38–45. https://doi.org/10.1080/14660820500396877
Watanabe K, Hasegawa K, Hirano T et al (2005) Anterior spinal decompression and fusion for cervical flexion myelopathy in young patients. J Neurosurg Spine 3:86–91. https://doi.org/10.3171/spi.2005.3.2.0086
Huang YL, Chen CJ (2011) Hirayama disease. Neuroimaging Clin N Am 21:939–950. https://doi.org/10.1016/j.nic.2011.07.009
Lai V, Wong YC, Poon WL et al (2011) Forward shifting of posterior dural sac during flexion cervical magnetic resonance imaging in Hirayama disease: an initial study on normal subjects compared to patients with Hirayama disease. Eur J Radiol 80:724–728. https://doi.org/10.1016/j.ejrad.2010.07.021
Goel A, Dhar A, Shah A (2017) Multilevel spinal stabilization as a treatment for Hirayama disease: report of an experience with five cases. World Neurosurg 99:186–191. https://doi.org/10.1016/j.wneu.2016.11.143
Yin B, Liu L, Geng DY (2011) Features of Hirayama disease on fully flexed position cervical MRI. J Int Med Res 39:222–228. https://doi.org/10.1177/147323001103900124
Xu X, Han H, Gao H et al (2011) The increased range of cervical flexed motion detected by radiographs in Hirayama disease. Eur J Radiol 78:82–86. https://doi.org/10.1016/j.ejrad.2010.08.012
Wang H, Sun C, Yang S et al (2018) Dynamic cervical radiographs in patients with Hirayama disease: an unneglectable factor on the choice of surgery options. World Neurosurg 114:e433–e440. https://doi.org/10.1016/j.wneu.2018.03.004
Liu X, Sun Y (2013) The correlation analysis of the cervical spine alignment flexion ROM of adjacent segments with the spinal cord atrophy in Hirayama disease. Chin J Spine Spinal Cord 23:514–519
Panjabi MM, Cholewicki J, Nibu K et al (1998) Critical load of the human cervical spine: an in vitro experimental study. Clin Biomech (Bristol, Avon) 13:11–17
Thakar S, Mohan D, Furtado SV et al (2014) Paraspinal muscle morphometry in cervical spondylotic myelopathy and its implications in clinicoradiological outcomes following central corpectomy: clinical article. J Neurosurg Spine 21:223–230. https://doi.org/10.3171/2014.4.SPINE13627
Jones EJ, Bishop PA, Woods AK, Green JM (2008) Cross-sectional area and muscular strength: a brief review. Sport Med 38:987–994. https://doi.org/10.2165/00007256-200838120-00003
Blazevich AJ, Coleman DR, Horne S, Cannavan D (2009) Anatomical predictors of maximum isometric and concentric knee extensor moment. Eur J Appl Physiol 105:869–878. https://doi.org/10.1007/s00421-008-0972-7
Okada E, Matsumoto M, Ichihara D et al (2011) Cross-sectional area of posterior extensor muscles of the cervical spine in asymptomatic subjects: a 10-year longitudinal magnetic resonance imaging study. Eur Spine J 20:1567–1573. https://doi.org/10.1007/s00586-011-1774-x
Thakar S, Kurudi Siddappa A, Aryan S et al (2017) Does the mesodermal derangement in Chiari Type I malformation extend to the cervical spine? Evidence from an analytical morphometric study on cervical paraspinal muscles. J Neurosurg Spine 27:421–427. https://doi.org/10.3171/2016.12.SPINE16914
Elliott JM, Jull GA, Noteboom JT et al (2007) Magnetic resonance imaging study of cross-sectional area of the cervical extensor musculature in an asymptomatic cohort. Clin Anat 20:35–40. https://doi.org/10.1002/ca.20252
Takeuchi K, Yokoyama T, Aburakawa S et al (2005) Axial symptoms after cervical laminoplasty with C3 laminectomy compared with conventional C3–C7 laminoplasty: a modified laminoplasty preserving the semispinalis cervicis inserted into axis. Spine (Phila Pa 1976) 30:2544–2549
Hirayama K (2008) Juvenile muscular atrophy of unilateral upper extremity (Hirayama disease)–half-century progress and establishment since its discovery. Brain Nerve 60:17–29
Garfin SR, Eismont FJ, Bell GR et al (2018) Rothman-Simeone and Herkowitz’s, the spine, 7th edn. Elsevier, Philadelphia
Ozaki H, Kubota A, Natsume T et al (2018) Effects of drop sets with resistance training on increases in muscle CSA, strength, and endurance: a pilot study. J Sport Sci 36:691–696. https://doi.org/10.1080/02640414.2017.1331042
Enix DE, Scali F, Pontell ME (2014) The cervical myodural bridge, a review of literature and clinical implications. J Can Chiropr Assoc 58:184–192
Yoon SY, Moon HI, Lee SC et al (2018) Association between cervical lordotic curvature and cervical muscle cross-sectional area in patients with loss of cervical lordosis. Clin Anat 31:710–715. https://doi.org/10.1002/ca.23074
Cheng CH, Lin KH, Wang JL (2008) Co-contraction of cervical muscles during sagittal and coronal neck motions at different movement speeds. Eur J Appl Physiol 103:647–654. https://doi.org/10.1007/s00421-008-0760-4
Cheng CH, Cheng HY, Chen CP et al (2014) Altered Co-contraction of cervical muscles in young adults with chronic neck pain during voluntary neck motions. J Phys Ther Sci 26:587–590. https://doi.org/10.1589/jpts.26.587
Lin MS, Kung WM, Chiu WT et al (2010) Hirayama disease. J Neurosurg Spine 12:629–634. https://doi.org/10.3171/2009.12.SPINE09431
Lu F, Wang H, Jiang J et al (2013) Efficacy of anterior cervical decompression and fusion procedures for monomelic amyotrophy treatment: a prospective randomized controlled trial: clinical article. J Neurosurg Spine 19:412–419. https://doi.org/10.3171/2013.4.SPINE12575
Tokumaru Y, Hirayama K (2001) Cervical collar therapy for juvenile muscular atrophy of distal upper extremity (Hirayama disease): results from 38 cases. Rinsho Shinkeigaku 41:173–178
Fu Y, Qin W, Sun QL, Fan DS (2016) Investigation of the compliance of cervical collar therapy in 73 patients with Hirayama disease. Zhonghua Yi Xue Za Zhi 96:3485–3488. https://doi.org/10.3760/cma.j.issn.0376-2491.2016.43.009
Borisut S, Vongsirinavarat M, Vachalathiti R, Sakulsriprasert P (2013) Effects of strength and endurance training of superficial and deep neck muscles on muscle activities and pain levels of females with chronic neck pain. J Phys Ther Sci 25:1157–1162. https://doi.org/10.1589/jpts.25.1157
Gross AR, Paquin JP, Dupont G et al (2016) Exercises for mechanical neck disorders: a cochrane review update. Man Ther 24:25–45. https://doi.org/10.1016/j.math.2016.04.005
Acknowledgements
We thank the support from colleagues in our department. Our special thanks go to Dr. Eric Rebich, from Harborview Medical Center, University of Washington, Seattle, USA, for providing language help. We also appreciate the grant from the Startup Fund for scientific research, Fujian Medical University (2018QH1072).
Funding
This study was supported by a grant from Startup Fund for scientific research, Fujian Medical University (2018QH1072).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Li, Z., Zhang, W., Wu, W. et al. Is there cervical spine muscle weakness in patients with Hirayama disease? A morphological study about cross-sectional areas of muscles on MRI. Eur Spine J 29, 1022–1028 (2020). https://doi.org/10.1007/s00586-020-06290-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-020-06290-1