Abstract
This study investigated the association between body composition and risk of atrial fibrillation (AF) in postmenopausal women. In a retrospective analysis we assessed data from 5704 postmenopausal women (age 70.7 ± 6.5 yrs.) who in 1999–2001 participated in The Prospective Epidemiological Risk Factor study with body composition assessed by dual-energy X-ray absorptiometry. Outcomes were obtained from Danish Health Registries and body composition association to risk of AF was evaluated by univariable and multivariable Cox Hazard regression. 850 women developed AF after baseline. High lean body mass was associated with increased risk of AF in multivariable analyses, adjusting for body mass index (BMI), height or weight (adjusted for: BMI, hazard ratio (HR) 1.49, 95% Confidence Interval (1.22–1.80); height, HR 1.27 (1.03–1.56); weight, 1.33 (1.06–1.65)). Height and weight were associated with increased risk of AF in multivariable analyses adjusting for body composition measures. When adjusting for total lean mass, only height remained statistically significant (HR 1.34 (1.09–1.64)). In a cohort of elderly Caucasian women, high lean body mass, height and weight were associated with increased risk of AF and the variables remained significant after adjusting for age and other known risk factors of AF.
Similar content being viewed by others
Introduction
Obesity is linked to cardiovascular disease (CVD) including atrial fibrillation (AF) and AF is the most common arrhythmia1 with prevalence that increases with age. In women, AF presents later in life compared to men and AF seldomly manifests before menopause2.
Several risk factors of AF including hypertension, diabetes, heart failure and myocardial infarction have been identified in previous studies3,4,5. While obesity defined by body mass index (BMI; ≥30 kg/m2) is a known modifiable risk factor of AF in both men and women5,6,7, height has also been suggested a risk factor for AF8,9. Furthermor, other less explored body composition measures may be important for development of AF. In a bio-impedance study including middle aged men and women (approx. 60 years, 47.6% males), lean body mass was associated with increased risk of AF10,11. Also, using dual-energy X-ray absorptiometry (DXA) to assess body composition in 60 year old women, lean body mass was associated with increased risk of AF12. Furthermore, in older adults total fat mass9,13, fat free mass9 and height9 were associated with risk of AF. Karas et al. concluded that their evaluation on 1050 incident AF in 4276 participants is the largest study focused on older adults to report on anthropometric variables, along with measures of fat and fat-free mass9. Cohorts on elderly women only are in need as the postmenopausal phase involves high risk for development CVD14 concomitant with significant change in body composition. Thus, women loose subcutaneous fat but gain abdominal fat with age15 paralleled with a progressive decline in muscle mass and strength and muscle function become impaired16. Accumulation of visceral fat involves activation of inflammatory pathways17 with potential for development of atrial fibrosis5. Also pericardial and epicardial fat accumulation associate to AF18,19,20.
To explore further the AF risk in elderly women data from the Prospective Epidemiological Risk Factor Study (PERF) were applied. The PERF cohort represents a large sample of elderly Caucasian females (n = 5855) who had their body composition assessed by DXA. We aimed to investigate whether different body composition measures (fat and lean body mass) and anthropometric measures (BMI, height and weight) are associated to risk of AF in elderly women.
Methods
Study population
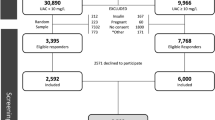
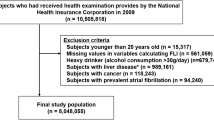
The PERF cohort21 was established to identify risk factors for age-related diseases and includes Danish post-menopausal women who had either been screened for or participated in clinical prevention trials at the Center for Clinical and Basic Research, Denmark. Among the source population, 8875 women were approached by letter in accordance with approval by the Research Ethics Committee of Copenhagen County, Viborg and Northern Jutland, Denmark (KA 99070 gm). Of these, 732 women had died. Following written informed consent 5855 women (age 70.7 ± 6.5 years) were included in the PERF cohort between 1999–200121 (baseline) giving a response rate of 72% of the women alive at time of enrolment in PERF. Inclusion and exclusion criteria at the time of enrolment was limited to women who were postmenopausal and the study is considered a retrospective analysis of a prospective study-design. All participants attended a physical examination and blood was sampled at baseline. Demographics were obtained through interview by a doctor or a nurse. The interview focused on family history of disease, reproduction and previous health status as well as use of medicine including hormonal replacement therapy (HRT) level of education (elementary, secondary, university), and lifestyle habits such as engagement in physical exercise (hours per week), alcohol consumption (units per week) and smoking habits (never, previous, current). Follow-up was ensured with registry-based data using population-based national registries by matching the unique civil registration number for Danish residents. The cohort is considered to be representative for Danish elderly post-menopausal women21 with a detailed description of the PERF cohort published by Neergaard et al.21.
Inclusion and exclusion criteria
The present evaluation included all PERF women in whom the diagnosis code of AF in accordance with ICD-8 or ICD-10 was absent at baseline (Table 1). The registries used were the Danish National Patient Register, the Danish National Diabetes Register, and the Danish Register of Causes of Death. Latest linkage used for present study was January 2015.
Variables included in analysis
The variables included in the analysis for AF risk were those obtained from the baseline assessment including the DXA derived body compositions. AF was identified as the first registered diagnosis of AF in the Danish National Patient Registry. Also ischaemic heart disease (IHD), congestive heart failure (CHF), peripheral arterial disease (PAD), and thyroid disease prior to or at baseline were identified. Both ICD-8 and ICD-10 diagnostic codes were used (Table 1).
We also included diagnostic variables of hypertension, hyperlipidaemia and diabetes. Hypertension was defined in accordance to ICD-8 or ICD-10 classification or whether a participant was reported to use antihypertensive medication. A participant was also considered with hypertension if the baseline systolic pressure was above 145 mmHg or if the diastolic pressure was higher than 95 mmHg. A 5 mmHg higher limit for hypertension than normally used22 was chosen to minimise the risk of false positive. Hyperlipidaemia was defined as (i) baseline fasting s-cholesterol above 7.5 mmol/L23, (ii) relevant ICD-8 or ICD-10 classification, or (iii) hyperlipidaemia noted in the baseline questionnaire. A participant was considered diabetic in accordance to the ICD-8 or ICD-10 codes, or if the participant was listed in the National Diabetes register or if the baseline blood sample showed fasting s-glucose ≥7 mmol/L24.
Body composition measures
The included DXA scan derived body composition measures were total body fat mass (total fat mass (kg)), body fat percentage (fat %), total lean body mass (total lean mass (kg)) and lean body mass index (LBMi; total lean mass(kg)/height(m)2). The DXA scans were performed on three different machines [Lunar Prodigy (GE Lunar Corporation, Madison, WA), QDR 2000, or QDR 4500 (Hologic Inc., Waltham, MA)] and the body composition measures were calibrated by bone mineral content. The three groups of body composition measures were controlled to be normally distributed and then normalised by the median to assure comparability. Fat % was the percentage fat mass of total mass (total mass = total bone mineral content + total fat mass + lean body mass). In order to compare anthropometric measures and the DXA derived body composition measures weight, height and BMI were included in the analysis. The BMI was categorised as normal (<25 kg/m2), overweight (25− < 30 kg/m2), or obese (≥30 kg/m2). Height, weight and the derived body composition measures were categorised into tertiles: lowest (tertile 1 = T1), middle (tertile 2 = T2) and highest (tertile 3 = T3) with tertile 1 as the reference.
Statistical analysis
Baseline demographic characteristics of women with and without AF at end of the study were compared by a two-sided t-test for continuous variables and chi-square test for categorical variables. In the event of missing data for one or more variables, subjects were excluded from the individual analysis and the number included in analysis is reported for each individual analysis. The association between AF and the anthropometric measures or DXA scan derived body composition measures were evaluated by univariable proportional Cox hazard regressions. To adjust for confounders, two different multivariable Cox proportional hazards regression analysis were applied. Model 1 adjusted for age (in years) only. Model 2 adjusted for age (in years), previous/current smoker (yes/no), alcohol consumption ≥7 units/week (yes/no), level of education, physical activity ≥1 h/week (yes/no), HRT (yes/no) and comorbidities such as hypertension, hyperlipidaemia, diabetes, IHD, PAD, CHF. The scanner model was added as a covariable due to the data from the DXA scanners were not calibrated for all body composition measures. Models 1 and 2 were performed individually for the 3 anthropometric measures (BMI, height, weight) and the 4 body composition measures obtained from DXA scans (total fat mass, fat %, total lean mass, and LBMi).
To explore the relationship between body composition and the risk of AF, we performed another set of Cox proportional hazards regression analysis using all the variables in model 2 as well as including one anthropometric measure (BMI, height or weight) and one DXA-scan derived body composition measure (lean body mass, LBMi, total fat mass or fat %). Multicollinearity is underreported in epidemiological studies25. To test for multicollinearity between the body composition measures and the anthropometric measures, we used the Variance Inflation Factor (VIF)-test26. A Cox proportional hazards regression analysis using the variables of model 2 was used for the VIF-test. Since the cut-off value for the VIF-factor has to be interpreted with caution26 a cut-off of and above 2.5 was chosen.
R-software (R vers. 3.4.2, R Development Core Team, 2017) was used for analysis. The following packages were used with default settings: rms (V.5.1-3.1) and survival (V.2.4.3-3). Statistical significance was accepted at a p-value < 0.05.
Results
Baseline characteristics
Of the 5855 women in the PERF cohort, 5704 women (mean age 70.7 ± 6.5 yrs.) had no history of AF at baseline, but 850 women were diagnosed with new-onset AF after baseline (Table 2). Total follow-up was 14.4 years and as 1848 women (404 with AF and 1444 without) died before reaching the end of the follow-up, the average follow-up period was 11.5 years (SD +/− 4.3 years). The average time to AF was 7.6 years (SD +/− 4.1 years).
Table 2 shows demographics of women with and without AF. The women with AF after baseline were approx. three years older than women without AF while level of education, alcohol and smoking habits were similar in the two groups. The women with AF exercised less frequently and their systolic and diastolic blood pressures were significantly higher compared to women without AF. In the women with AF hypertension, diabetes, thyroid disease and heart disease including IHD and CHF, were significantly more prevalent than the women without AF. In contrast, hyperlipidaemia was less prevalent in women with compared to the women without AF. Women with AF were significantly taller, weighed more, had a larger total fat mass, larger lean body mass, and larger LBMi compared to the women without AF.
Body composition and the risk of AF
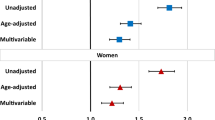
Table 3 shows the univariable and multivariable Cox hazard regression analysis of the DXA scan derived body composition and anthropometric variables association to risk of AF. The number of participants included in the individual analyses varied between 5119 and 5496.
Obese BMI, weight and height in T3 were significantly associated with an increased risk of AF in the two multivariable models. In the univariable analysis only obese BMI was significantly associated with increased risk of AF. Of the DXA scan derived body composition measures total fat mass and fat % in T3 were significantly associated with increased risk of AF in model 1 that adjusted for age only. The measures for lean mass, total lean mass and LBMi, total lean mass and LBMi in T3 were significantly associated with increased risk of AF in the univariable analysis. In the multivariable model 1 and 2, the T2 and T3 of total lean mass were significantly associated with increased risk of AF. The T3 of LBMi was associated with increased risk of AF in model 1. C-stat of the univariable analyses reached 0.52 or 0.53.
Multicollinearity
Multicollinearity was noted for all anthropometric variables and DXA scan derived measures, except for the T2 data on height (VIF 1.82), total lean mass (VIF 2.45) and LBMi (VIF 2.04) T2 (Table 3). Due to this multicollinearity, multivariable Cox hazard regression adjusting the DXA scan derived body composition measures for the anthropometric measures and vice versa were conducted. Table 4 shows that only total lean mass remained significantly associated with an increased risk of AF when adjusting for height, weight or BMI, but failed to remain significant when adjusting for both height and weight. Weight in T3 was significantly associated with increased risk of AF when adjusting for fat %, total fat mass and LBMi, but when adjusting for lean mass the association failed to remain significant. In all four analyses height in T3 was associated with a 34–56% increased risk of AF when adjusting for body fat, total fat mass, total lean mass, and LBMi.
Discussion
In this study on elderly post-menopausal women who were followed for 11.5 years, high lean body mass, high total fat mass, obese BMI, height and weight were all associated with an increased risk of atrial fibrillation (AF). Importantly, accumulation of fatty tissue to obese body stature was associated with AF risk in both univariable and multivariable analysis supporting AF risk evaluations in mixed gender populations7,9,13,27. When testing for correlations between the anthropometric measures and DXA scan derived body composition measures, lean body mass, weight and height remained associated with increased risk of AF.
The risk of developing AF doubles every 10th years of age28 and in a number of studies evaluating anthropometric measures such as BMI, obesity was associated with risk of AF7,9,13,27. The importance of height for AF risk in the elderly (age 72.4 years) was indicated by analysis of data from participants in the Cardiovascular Health Study8,9. Our data failed to yield a univariate association between height and risk of AF but when adjusting for age and potential confounders, height was associated with increased risk of AF. Thus, attempts to avoid stratification for age could mask the association between height and risk of AF, especially in elderly people. The c-statistics support that analysis should be adjusted for age.
In women, AF presents differently than in men2. Women are older at AF onset and they experience worse and longer-lasting symptoms2 with a higher risk of severe outcome including stroke5,29. These sex-related differences in manifestation of AF are not understood5. Men are taller than women, and also body composition could differentiate sex-related manifestation of AF. Thus, height of a person and atrial enlargement are risk factors of AF30. In the Framingham study and in the Framingham Offspring cohort, the risk of AF related to obesity diminished when adjusting for left atrial diameter7. Structural remodelling including atrial wall fibrosis31 mediates AF and although the atria are smaller in women, tendency to develop atrial wall fibrosis is greater in women than in men5 and obesity-induced inflammation may lead to atrial fibrosis and AF32,33. Notably, pericardial adipose tissue and in turn adipocyte infiltration causes fibrosis32,33 that disturbs cardiac electrical conduction32.
In a mixed gender cohort (average age range approximately 60 years,)10,11, larger weight, height, BMI, waist circumference, bioimpedance derived measures of body fat mass, fat % and lean body mass were associated with increased risk of AF11. Lean body mass was associated with an increased risk of AF when adjusting for any of the other anthropometric measures (BMI, height, weight, fat mass, fat %, hip circumference, waist circumference, and waist/hip-ratio)10. When adjusting the other measures for lean body mass, only height was associated with increased risk of AF10,11. Also, in a multiracial cohort an association between DXA-scan derived measures of lean body mass and risk of AF12 is described and a mendelian randomization study points to the importance of lean body mass and fat mass34.
Multicollinearity seems underreported in epidemiological studies25 and here evaluated by the VIF test26, although the cut off values of the VIF-test remain debated25. As expected, multicollinearity was identified and lean body mass is not considered the single driver of associations between body composition and increased risk of AF. The relationship between AF and other measures of body composition and anthropometry needs to be considered.
Clinical relevance
The clinical relevance is that large body stature might mediate AF35. The modifiable risk factors of AF are important when trying to decrease risk of developing AF. Height is a fixed value, but weight and obesity are modifiable. Getting access to data on a patients’ lean mass requires, e.g. bioimpedance or DXA scans, whereas assessment of weight and height are easier on-the-spot measures. Of importance, the obese person needs a large skeletal muscle mass to carry the fat mass. Cardiac hypertrophy may develop secondary to increased cardiac output and may further increase risk of AF35. Yet, how obesity mediates AF needs to be established.
Strength and limitations
The study is restricted to elderly females of Caucasian origin. Information regarding life-style habits and use of medication was obtained through interview, and thus based on memory with potential risk for type 2 error and recall bias. We consider this risk of minimal importance since the questionnaire was performed by professional health-care staff and the questions were simple. It is also a limitation that only four women had a BMI <18.5 kg/m2.
A strength of the study is the prospective design and the long follow-up period. Likewise, the overall good quality of variables for analysis including DXA scans and access to the Danish registries add to the strength. Secondly, when differentiation between occurrence of atrial fibrillation vs. atrial flutter is avoided, the AF diagnosis is highly valid36. Although use of diagnosis in registries may have limitations, the national Danish registries are unique in that they are the oldest where individuals are coded in accordance to their personal identification number. Further, data were cross-referenced with other national databases. In addition, completeness of the different diagnoses including CVD is high in Danish registries37,38 except that uncomplicated hypertension and diabetes may be incomplete. Adding information about previous hypertensive treatment, blood pressure at baseline and a diagnosis of hypertension improved quality of the diagnosis of hypertension in our study. Regarding diagnosis of diabetes we added information from the Danish National Diabetes Register and blood glucose levels indicative of diabetes.
In conclusion, in a cohort of elderly Caucasian women who were followed for 11.5 years, high lean body mass, height and weight were associated with increased risk of AF. This effect remained significant after adjusting for age and other known risk factors of AF. We suggest that tall elderly women with large muscle mass need specific attention on AF risk.
Data availability
The data are not publicly available due to legal and ethical reasons. The data are however available on request from the corresponding author on the condition that the researchers have the appropriate permissions from the Danish Data Protection agency and sign a confidentiality agreement.
References
Chugh, S. S. et al. Worldwide epidemiology of atrial fibrillation: A global burden of disease 2010 study. Circulation 129, 837–847 (2014).
Feinberg, W. M. Prevalence, Age Distribution, and Gender of Patients With Atrial Fibrillation. Arch. Intern. Med. 155, 469–73 (1995).
Frost, L., Hune, L. J. & Vestergaard, P. Overweight and obesity as risk factors for atrial fibrillation or flutter: The Danish Diet, Cancer, and Health Study. Am. J. Med. 118, 489–495 (2005).
Perez, M. V. et al. Risk factors for atrial fibrillation and their population burden in postmenopausal women: the Women’s Health Initiative Observational Study. Heart 99, 1173–1178 (2013).
Ko, D. et al. Atrial fibrillation in women: epidemiology, pathophysiology, presentation, and prognosis. Nat. Rev. Cardiol. 13, 321–332 (2016).
Overvad, T. F. et al. Body Mass Index and Adverse Events in Patients with Incident Atrial Fibrillation. Am. J. Med. 126, 640.e9–640.e17 (2013).
Wang, T. J. et al. Obesity and the Risk of New-Onset Atrial Fibrillation. Jama 292, 2471 (2004).
Rosenberg, M. A. et al. The impact of height on the risk of atrial fibrillation: The Cardiovascular Health Study. Eur. Heart J. 33, 2709–2717 (2012).
Karas, M. G. et al. Measures of Body Size and Composition and Risk of Incident Atrial Fibrillation in Older People. Am. J. Epidemiol. 183, 998–1007 (2016).
Fenger-Grøn, M., Overvad, K., Tjønneland, A. & Frost, L. Lean Body Mass Is the Predominant Anthropometric Risk Factor for Atrial Fibrillation. J. Am. Coll. Cardiol. 69, 2488–2497 (2017).
Frost, L. et al. Body fat, body fat distribution, lean body mass and atrial fibrillation and flutter. A Danish cohort study. Obesity (Silver Spring). 22, 1546–52 (2014).
Azarbal, F. et al. Lean body mass and risk of incident atrial fibrillation in post-menopausal women. Eur. Heart J. 37, 1606–1613 (2016).
Aronis, K. N. et al. Associations of obesity and body fat distribution with incident atrial fibrillation in the biracial health aging and body composition cohort of older adults. Am. Heart J. 170, 498–505.e2 (2015).
Hu, F. B. et al. Age at Natural Menopause and Risk of Cardiovascular Disease. Arch. Intern. Med. 159, 1061 (1999).
Lizcano, F. & Guzmán, G. Estrogen deficiency and the origin of obesity during menopause. Biomed Res. Int. 2014 (2014).
Cruz-Jentoft, A. J. et al. Sarcopenia: European consensus on definition and diagnosis. Age Ageing 39, 412–423 (2010).
Farb, M. G. et al. Arteriolar function in visceral adipose tissue is impaired in human obesity. Arterioscler. Thromb. Vasc. Biol. 32, 467–473 (2012).
Wong, C. X. et al. Pericardial fat is associated with atrial fibrillation severity and ablation outcome. J. Am. Coll. Cardiol. 57, 1745–1751 (2011).
Wong, C. X. et al. Associations of Epicardial, Abdominal, and Overall Adiposity with Atrial Fibrillation. Circ. Arrhythmia Electrophysiol. 9, e004378 (2016).
Lee, J. J., Yin, X., Hoffmann, U., Fox, C. S. & Benjamin, E. J. Relation of Pericardial Fat, Intrathoracic Fat, and Abdominal Visceral Fat With Incident Atrial Fibrillation (from the Framingham Heart Study). Am. J. Cardiol. 118, 1486–1492 (2016).
Neergaard, J. S. et al. Cohort Profile: The Prospective Epidemiological Risk Factor (PERF) study. Int. J. Epidemiol. 46, 1104–1104i (2017).
Mancia, G. et al. ESH/ESC guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur. Heart J. 34, 2159–2219 (2013).
Catapano, A. L. et al. ESC/EAS Guidelines for the Management of Dyslipidaemias. Eur. Heart J. 37, 2999–3058l (2016).
WHO & IDF. Definition and diagnosis of diabetes mellitus and intermediate hyperglycaemia. (WHO; IDF;, 2006).
Vatcheva, K. P., Lee, M., Mccormick, J. B., Rahbar, M. H. & Vetcheva, K. P. Multicollinearity in Regression Analyses Conducted in Epidemiologic Studies. Epidemiology 6, 1–20 (2016).
O’brien, R. M. A Caution Regarding Rules of Thumb for Variance A Caution Regarding Rules of Thumb for Variance Inflation Factors. Qual. Quant. 41, 673 (2007).
Benjamin, E. J. et al. Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Heart Study. Jama 271, 840–4 (1994).
Tedrow, U. B. et al. The Long- and Short-Term Impact of Elevated Body Mass Index on the Risk of New Atrial Fibrillation. The WHS (Women’s Health Study). J. Am. Coll. Cardiol. 55, 2319–2327 (2010).
Friberg, J., Scharling, H., Gadsbøll, N., Truelsen, T. & Jensen, G. B. Comparison of the impact of atrial fibrillation on the risk of stroke and cardiovascular death in women versus men (The Copenhagen City Heart Study). Am. J. Cardiol. 94, 889–894 (2004).
Mont, L. et al. Physical activity, height, and left atrial size are independent risk factors for lone atrial fibrillation in middle-aged healthy individuals. Europace 10, 15–20 (2008).
Andrade, J., Khairy, P., Dobrev, D. & Nattel, S. The clinical profile and pathophysiology of atrial fibrillation: Relationships among clinical features, epidemiology, and mechanisms. Circ. Res. 114, 1453–1468 (2014).
Wong, C. X., Ganesan, A. N. & Selvanayagam, J. B. Epicardial fat and atrial fibrillation: Current evidence, potential mechanisms, clinical implications, and future directions. Eur. Heart J. 38, 1294–1302 (2017).
Hu, Y.-F., Chen, Y.-J., Lin, Y.-J. & Chen, S.-A. Inflammation and the pathogenesis of atrial fibrillation. Nat. Rev. Cardiol. 12, 230–243 (2015).
Tikkanen, E. et al. Body composition and atrial fibrillation: A Mendelian randomization study. Eur. Heart J. 40, 1277–1282 (2019).
Nattel, S. Atrial Fibrillation and Body Composition Is it Fat or Lean That Ultimately Determines the Risk? J. Am. Coll. Cardiol. 69, 2498–2501 (2017).
Rix, T. A. et al. Validity of the diagnoses atrial fibrillation and atrial flutter in a Danish patient registry. Scand. Cardiovasc. J. 46, 149–153 (2012).
Schmidt, M. et al. The Danish National patient registry: A review of content, data quality, and research potential. Clin. Epidemiol. 7, 449–490 (2015).
Sundbøll, J. et al. Positive predictive value of cardiovascular diagnoses in the Danish National Patient Registry: A validation study. BMJ Open 6 (2016).
Acknowledgements
We would like to acknowledge the Danish Research Foundation (Den Danske Forskningsfond) for financial support.
Author information
Authors and Affiliations
Contributions
H.B.N., C.B. and M.S.W. contributed to the conception and design of the study. M.S.W., C.B. and J.P.B. performed the statistical analysis and prepared tables. C.C. and B.J.R. performed and funded PERF as well as contributed to design of present study. M.S.W., H.B.N., C.B., J.P.B. and N.H.S. wrote the manuscript. All authors reviewed the manuscript and approved the final version to be published.
Corresponding author
Ethics declarations
Competing interests
C.B. and J.P.B. are employees at Proscion. H.B.N. is an employee at Sanos Clinic. C.C. and B.J.R. hold stocks at Nordic Bioscience. M.S.W. and N.H.S. have no competing interests to declare.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Worm, M.S., Bager, C.L., Blair, J.P.M. et al. Atrial fibrillation is associated with lean body mass in postmenopausal women. Sci Rep 10, 573 (2020). https://doi.org/10.1038/s41598-019-57167-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-57167-3
This article is cited by
-
The physiology of rowing with perspective on training and health
European Journal of Applied Physiology (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.