Abstract
Purpose
A-pattern exotropia, superior oblique muscle overaction, and dissociated vertical deviation may coexist and are referred to as triad exotropia. The present study evaluated the postoperative stability of horizontal ocular alignment of triad exotropia and possible prognostic factors.
Methods
Medical records of patients with triad exotropia who had one-step triple surgery of superior oblique muscle weakening, superior rectus muscle recession, and lateral rectus muscle recession were reviewed. The horizontal alignment and postoperative drift of triad exotropia were analyzed and compared with constant exotropia.
Results
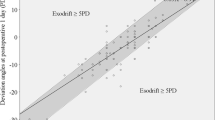
The triad exotropia showed a mean of 7.7△ (± 8.5△) eso-drift, while the constant exotropia was (3.5△ ± 3.4△) exo-drift. Multiple linear regression analysis showed that the degree of superior oblique muscle overaction after surgery (P = 0.011) was the only factor associated with horizontal drift. Patients with superior oblique muscle underaction showed larger eso-drift when compared to patients without superior oblique muscle underaction (− 18.0△ ± 11.1△ vs. − 5.1△ ± 5.7△; P = 0.024). The final success rates of the triad exotropia and constant exotropia groups were 53.3% and 69.2%, respectively, and the overcorrection rates were 26.7% and 2.6% (P = 0.035).
Conclusions
An overall trend of eso-drift in primary position occurred in triad exotropia after triple surgery up to a follow-up of 25 months. Patients presenting superior oblique muscle underaction after surgery seemed to have large angles of eso-drift, which might be taken into account in surgical planning and follow-up.






Similar content being viewed by others
References
Velez FG, Ela-Dalman N, Velez G (2009) Surgical management of dissociated vertical deviation associated with A-pattern strabismus. J Am Assoc Pediatr Ophthalmol Strabismus 13:31–35. https://doi.org/10.1016/j.jaapos.2008.09.006
Helveston EM (1969) A-exotropia, alternating sursumduction, and superior oblique overaction. Am J Ophthalmol 67:377–380
Ha SG, Suh YW, Kim SH (2017) Clinical features and surgical outcome of triad exotropia. J Pediatr Ophthalmol Strabismus 54:363–368. https://doi.org/10.3928/01913913-20170329-03
Melek NB, Mendoza T, Ciancia AO (1998) Bilateral recession of superior rectus muscles: its influence on A and V pattern strabismus. J AAPOS 2:333–335
McCall LC, Rosenbaum AL (1991) Incomitant dissociated vertical deviation and superior oblique overaction. Ophthalmology 98:911–918. https://doi.org/10.1016/s0161-6420(91)32202-4
Pineles SL, Rosenbaum AL, Demer JL (2009) Decreased postoperative drift in intermittent exotropia associated with A and V patterns. J AAPOS 13:127–131. https://doi.org/10.1016/j.jaapos.2008.10.013
Mohney BG, Holmes JM (2006) An office-based scale for assessing control in intermittent exotropia. Strabismus 14:147–150. https://doi.org/10.1080/09273970600894716
Hunter LR, Parks MM (1990) Response of coexisting underacting superior oblique and overacting inferior oblique muscles to inferior oblique weakening. J Pediatr Ophthalmol Strabismus 27:74–79
Li Y, Ma H, Zhao K (2016) Effects of bilateral superior oblique “hang-back” recession in treatment of A-pattern strabismus with superior oblique overaction. Strabismus 24:1–6. https://doi.org/10.3109/09273972.2015.1130063
Xie F, Zhao K, Zhang W (2019) Comparison of surgical outcomes between bilateral recession and unilateral recession-resection in moderate-angle intermittent exotropia. J AAPOS 23:79.e71–79.e77. https://doi.org/10.1016/j.jaapos.2018.11.007
Yam JC, Wu PK, Chong GS, Wong US, Chan CW, Ko ST (2012) Long-term ocular alignment after bilateral lateral rectus recession in children with infantile and intermittent exotropia. J AAPOS 16:274–279. https://doi.org/10.1016/j.jaapos.2012.01.005
Choi J, Chang JW, Kim SJ, Yu YS (2012) The long-term survival analysis of bilateral lateral rectus recession versus unilateral recession-resection for intermittent exotropia. Am J Ophthalmol 153(343–351):e341. https://doi.org/10.1016/j.ajo.2011.06.024
Richard JM, Parks MM (1983) Intermittent exotropia. Surgical results in different age groups. Ophthalmology 90:1172–1177
Stoller SH, Simon JW, Lininger LL (1994) Bilateral lateral rectus recession for exotropia: a survival analysis. J Pediatr Ophthalmol Strabismus 31:89–92
Kushner BJ (1998) Selective surgery for intermittent exotropia based on distance/near differences. Arch Ophthalmol 116:324–328. https://doi.org/10.1001/archopht.116.3.324
Ekdawi NS, Nusz KJ, Diehl NN, Mohney BG (2009) Postoperative outcomes in children with intermittent exotropia from a population-based cohort. J AAPOS 13:4–7. https://doi.org/10.1016/j.jaapos.2008.06.001
Leow PL, Ko ST, Wu PK, Chan CW (2010) Exotropic drift and ocular alignment after surgical correction for intermittent exotropia. J Pediatr Ophthalmol Strabismus 47:12–16. https://doi.org/10.3928/01913913-20100106-04
Na KH, Kim SH (2016) Comparison of clinical features and long-term surgical outcomes in infantile constant and intermittent exotropia. J Pediatr Ophthalmol Strabismus 53:99–104. https://doi.org/10.3928/01913913-20160122-05
Isenberg SJ, Abdarbashi P (2009) Drift of ocular alignment following strabismus surgery. Part 2: using adjustable sutures. Br J Ophthalmol 93:443–447. https://doi.org/10.1136/bjo.2007.136382
Park H, Kim WJ, Kim MM (2016) The stabilization of postoperative exo-drift in intermittent exotropia after surgical treatment. Korean J Ophthalmol 30:60–65. https://doi.org/10.3341/kjo.2016.30.1.60
Souza-Dias C (2011) Horizontal effect of the surgical weakening of the oblique muscles. Arq Bras Oftalmol 74:382. https://doi.org/10.1590/s0004-27492011000500017
Jin YH, Sung KR, Kook MS (1999) The immediate effect of bilateral superior obliuqe tenotomy on primary position horizontal binocular alignment. Binocular vision & strabismus quarterly 14:33–38
Diamond GRPM (1981) The effect of superior oblique weakening procedures on primary position horizontal alignment. J Pediatr Ophthalmol Strabismus 18:35–38
Harley RD, Manley DR (1969) Bilateral superior oblique tenectomy in A-pattern exotropia. Trans Am Ophthalmol Soc 67:324–338
Pollard ZF (1978) Superior oblique tenectomy in a pattern strabismus. Ann Ophthalmol 10:211–215
Ung T, Raoof N, Burke J (2011) Effect of superior oblique weakening on vertical alignment and horizontal and vertical incomitance in patients with A-pattern strabismus. J Am Assoc Pediatr Ophthalmol Strabismus 15:9–13. https://doi.org/10.1016/j.jaapos.2010.11.007
Fierson WM, Boger WP 3rd, Diorio PC, Petersen RA, Robb RM (1980) The effect of bilateral superior oblique tenotomy on horizontal deviation in A-pattern strabismus. J Pediatr Ophthalmol Strabismus 17:364–371
Ron Y, Snir M, Axer-Seigel R, Friling R (2009) Z-tenotomy of the superior oblique tendon and horizontal rectus muscle surgery for A-pattern horizontal strabismus. J Am Assoc Pediatr Ophthalmol Strabismus 13:27–30. https://doi.org/10.1016/j.jaapos.2008.09.004
Funding
This study was funded by the National Natural Science Foundation of China (Grant No. 81600765); the Foundation of Shanghai Municipal Commission of Health and Family Planning (Project No. 201640120); Shanghai Outstanding Academic Leaders (2017BR013); and Excellent Academic Leaders of Shanghai (18XD1401000).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional review board of Eye and ENT Hospital, Fudan University and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wu, L., Xia, W., Li, L. et al. The stability of horizontal ocular alignment of triad exotropia after one-step triple surgery. Graefes Arch Clin Exp Ophthalmol 258, 899–908 (2020). https://doi.org/10.1007/s00417-019-04599-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-019-04599-2