Abstract
Background/Objectives
The results linking body iron stores to the risk of gestational diabetes mellitus (GDM) are conflicting. We aimed to measure the serum ferritin level of women in early pregnancy and evaluate the risk of GDM in a Chinese urban population.
Subjects/Methods
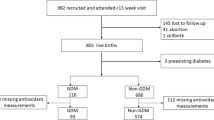
In total, 851 pregnant women between 10 and 20 weeks of gestation took part in the prospective, observational study conducted. The women were divided into four groups by quartiles of serum ferritin levels (Q1–4). Their blood samples were collected and assayed for several biochemical variables at the beginning of the study, and the women were followed up with a 75-g oral glucose tolerance test at 24–28 weeks of gestation.
Results
The participants had an average serum ferritin concentration of 65.67 μg/L. GDM prevalence within each serum ferritin quartile was 9.4%, 14.6%, 18.8% and 19.3%, respectively, (P = 0.016). The odds ratio for GDM in the ferritin Q2–4 was 1.64 (CI: 0.90–2.99), 2.23 (CI: 1.26–3.96) and 2.31 (CI: 1.30–4.10), compared with Q1, respectively. This association persisted after adjusting for potential confounders factors. In addition, in Q4, pregnant women with a pre-pregnancy body mass index ≥24 kg/m2, maternal age ≤35 years old or haemoglobin≥ 110 g/L did have an increased risk of developing GDM.
Conclusions
Elevated serum ferritin concentrations in early gestation are associated with an increased risk of GDM, especially in pregnant women who have a high baseline iron storage status with no anaemia or who are overweight/obese. Individual iron supplementation should be considered to minimize the risk of GDM.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
WHO. Guideline: daily iron and folic acid supplementation in pregnant women. Geneva: World Health Organization; 2012.
Burke RM, Leon JS, Suchdev PS. Identification, prevention and treatment of iron deficiency during the first 1000 days. Nutrients. 2014;6:4093–114.
Wessling-Resnick M. Excess iron: considerations related to development and early growth. Am J Clin Nutr. 2017;106:1600S–5S.
Hansen JB, Tonnesen MF, Madsen AN, Hagedorn PH, Friberg J, Grunnet LG, et al. Divalent metal transporter 1 regulates iron-mediated ROS and pancreatic beta cell fate in response to cytokines. Cell Metab. 2012;16:449–61.
Hansen JB, Moen IW, Mandrup-Poulsen T. Iron: the hard player in diabetes pathophysiology. Acta Physiol. 2014;210:717–32.
Jiang R, Manson JE, Meigs JB, Ma J, Rifai N, Hu FB. Body iron stores in relation to risk of type 2 diabetes in apparently healthy women. J Am Med Assoc. 2004;291:711–7.
Fernandez-Real JM, Lopez-Bermejo A, Ricart W. Cross-talk between iron metabolism and diabetes. Diabetes. 2002;51:2348–54.
Bao W, Rong Y, Rong S, Liu L. Dietary iron intake, body iron stores, and the risk of type 2 diabetes: a systematic review and meta-analysis. BMC Med. 2012;10:119.
Hunnicutt J, He K, Xun P. Dietary iron intake and body iron stores are associated with risk of coronary heart disease in a meta-analysis of prospective cohort studies. J Nutr. 2014;144:359–66.
Zein S, Rachidi S, Awada S, Osman M, Al-Hajje A, Shami N, et al. High iron level in early pregnancy increased glucose intolerance. J Trace Elem Med Biol. 2015;30:220–5.
Chan KKL, Chan BCP, Lam KF, Tam S, Lao TT. Iron supplement in pregnancy and development of gestational diabetes-a randomised placebo-controlled trial. Int J Obstet Gynaecol. 2009;116:789–98.
Kinnunen TI, Luoto R, Helin A, Hemminki E. Supplemental iron intake and the risk of glucose intolerance in pregnancy: re-analysis of a randomised controlled trial in Finland. Matern Child Nutr. 2016;12:74–84.
Zein S, Rachidi IS, Shang N, Sharara I, Cheikh-Ali K, Gauchez AS, et al. Association between iron level, glucose impairment and increased DNA damage during pregnancy. J Trace Elem Med Biol. 2017;43:52–7.
Afkhami-Ardekani M, Rashidi M. Iron status in women with and without gestational diabetes mellitus. J Diabetes Complicat. 2009;23:194–8.
Soubasi V, Petridou S, Sarafidis K, Tsantali C, Diamanti E, Buonocore G, et al. Association of increased maternal ferritin levels with gestational diabetes and intra-uterine growth retardation. Diabetes Metab. 2010;36:58–63.
Zein S, Rachidi S, Hininger-Favier I. Is oxidative stress induced by iron status associated with gestational diabetes mellitus? J Trace Elem Med Biol. 2014;28:65–9.
Bowers K, Yeung E, Williams MA, Qi L, Tobias DK, Hu FB, et al. A prospective study of prepregnancy dietary iron intake and risk for gestational diabetes mellitus. Diabetes Care. 2011;34:1557–63.
Gu Y, Su X, Li Y, Tang Y, Bao Y, Ying H. Do free thyroxine levels influence the relationship between maternal serum ferritin and gestational diabetes mellitus in early pregnancy? Diabetes Res Clin Pract. 2019;151:114–9.
Amiri FN, Basirat Z, Omidvar S, Sharbatdaran M, Tilaki KH, Pouramir M. Comparison of the serum iron, ferritin levels and total iron-binding capacity between pregnant women with and without gestational diabetes. J Nat Sci Biol Med. 2013;4:302–5.
Wang Z, Fan HB, Yang WW, Mao XD, Xu SH, Ma XP, et al. Correlation between plasma ferritin level and gestational diabetes mellitus and its impact on fetal macrosomia. J Diabetes Investig. 2018;9:1354–9.
Kataria Y, Wu Y, Horskjaer PH, Mandrup-Poulsen T, Ellervik C. Iron status and gestational diabetes-a meta-analysis. Nutrients. 2018;10:621.
Wang C, Wei Y, Zhang X, Zhang Y, Xu Q, Sun Y, et al. A randomized clinical trial of exercise during pregnancy to prevent gestational diabetes mellitus and improve pregnancy outcome in overweight and obese pregnant women. Am J Obstet Gynecol. 2017;216:340–51.
Metzger BE, Gabbe SG, Persson B, Buchanan TA, Catalano PM, Damm P, et al. International Association of Diabetes and Pregnancy Study Groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care. 2010;33:676–82.
Xiong X, Saunders LD, Wang FL, Demianczuk NN. Gestational diabetes mellitus: prevalence, risk factors, maternal and infant outcomes. Int J Gynecol Obstet. 2001;75:221–8.
MacDonald SC, Bodnar LM, Himes KP, Hutcheon JA. Patterns of gestational weight gain in early pregnancy and risk of gestational diabetes mellitus. Epidemiology. 2017;28:419–27.
Chen XH, Scholl TO, Stein TP. Association of elevated serum ferritin levels and the risk of gestational diabetes mellitus in pregnant women - the Camden study. Diabetes Care. 2006;29:1077–82.
Soheilykhah S, Mojibian M, Jannati Moghadam M. Serum ferritin concentration in early pregnancy and risk of subsequent development of gestational diabetes: a prospective study. Int J Reprod Biomed. 2017;15:155–60.
Abdul-Ghani MA, Abdul-Ghani T, Ali N, DeFronzo RA. One-hour plasma glucose concentration and the metabolic syndrome identify subjects at high risk for future type 2 diabetes. Diabetes Care. 2008;31:1650–5.
Abdul-Ghani MA, Lyssenko V, Tuomi T, DeFronzo RA, Groop L. Fasting versus postload plasma glucose concentration and the risk for future type 2 diabetes results from the Botnia study. Diabetes Care. 2009;32:281–6.
Phelps RL, Honig GR, Green D, Metzger BE, Frederiksen MC, Freinkel N. Biphasic changes in hemoglobin A1c concentrations during normal human pregnancy. Am J Obstet Gynecol. 1983;147:651–3.
Hinkle SN, Tsai MY, Rawal S, Albert PS, Zhang C. HbA1c measured in the first trimester of pregnancy and the association with gestational diabetes. Sci Rep. 2018;8:12249.
Hashimoto K, Noguchi S, Morimoto Y, Hamada S, Wasada K, Imai S, et al. A1C but not serum glycated albumin is elevated in late pregnancy owing to iron deficiency. Diabetes Care. 2008;31:1945–8.
Shanthi B, Revathy C, Manjula Devi AJ, Subhashree. Effect of iron deficiency on glycation of haemoglobin in nondiabetics. J Clin Diagn Res. 2013;7:15–7.
Coban E, Ozdogan M, Timuragaoglu A. Effect of iron deficiency anemia on the levels of hemoglobin A1c in nondiabetic patients. Acta Haematol. 2004;112:126–8.
Lurie S, Mamet Y. Red blood cell survival and kinetics during pregnancy. Eur J Obstet Gynecol Reprod Biol. 2000;93:185–92.
Kumari AS. Pregnancy outcome in women with morbid obesity. Int J Gynecol Obstet. 2001;73:101–7.
Baeten JM, Bukusi EA, Lambe M. Pregnancy complications and outcomes among overweight and obese nulliparous women. Am J Public Health. 2001;91:436–40.
Lao TT, Ho LF. Impact of iron deficiency anemia on prevalence of gestational diabetes mellitus. Diabetes Care. 2004;27:650–6.
Rawal S, Hinkle SN, Bao W, Zhu Y, Grewal J, Albert PS, et al. A longitudinal study of iron status during pregnancy and the risk of gestational diabetes: findings from a prospective, multiracial cohort. Diabetologia. 2017;60:249–57.
Bowers KA, Olsen SF, Bao W, Halldorsson TI, Strom M, Zhang C. Plasma concentrations of ferritin in early pregnancy are associated with risk of gestational diabetes mellitus in women in the Danish National Birth Cohort. J Nutr. 2016;146:1756–61.
Acknowledgements
The authors would like to give special thanks to all the participants of the study.
Funding
This study was supported by funds from the National Natural Science Foundation of China (Grant no. 81471469) and funds from the Science and Technology Commission of Shanghai Municipality (Grant no. 15411952900 and Grant no.14411965600).
Author information
Authors and Affiliations
Contributions
HDC conceptualized the project. QYZ designed the study. HDC and QYZ reviewed the manuscript and take primary responsibility for the final content. YC and TTL analysed the data and wrote the manuscript. MLH and SPL organized the participants. KW and ZWM performed data collection. JXL and JBL performed the laboratory work. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethics approval and consent to participate
This study was approved by the Ethics Committee of the Obstetrics and Gynecology Hospital, Fudan University, and all pregnant women provided consent to participate in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cheng, Y., Li, T., He, M. et al. The association of elevated serum ferritin concentration in early pregnancy with gestational diabetes mellitus: a prospective observational study. Eur J Clin Nutr 74, 741–748 (2020). https://doi.org/10.1038/s41430-019-0542-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-019-0542-6
This article is cited by
-
Ferritin and iron supplements in gestational diabetes mellitus: less or more?
European Journal of Nutrition (2024)
-
The associations of ferritin, serum lipid and plasma glucose levels across pregnancy in women with gestational diabetes mellitus and newborn birth weight
BMC Pregnancy and Childbirth (2023)
-
Association of Serum Ferritin Level in Early Second Trimester of Pregnancy with Development of Gestational Diabetes Mellitus: A Prospective Observational Study
The Journal of Obstetrics and Gynecology of India (2023)
-
Association of pre- and early-pregnancy factors with the risk for gestational diabetes mellitus in a large Chinese population
Scientific Reports (2021)