Abstract
High dietary glycaemic index (GI) and glycaemic load (GL) may increase cancer risk. However, limited information was available on GI and/or GL and head and neck cancer (HNC) risk. We conducted a pooled analysis on 8 case-control studies (4081 HNC cases; 7407 controls) from the International Head and Neck Cancer Epidemiology (INHANCE) consortium. We estimated the odds ratios (ORs) and 95% confidence intervals (CIs) of HNC, and its subsites, from fixed- or mixed-effects logistic models including centre-specific quartiles of GI or GL. GI, but not GL, had a weak positive association with HNC (ORQ4 vs. Q1 = 1.16; 95% CI = 1.02–1.31). In subsites, we found a positive association between GI and laryngeal cancer (ORQ4 vs. Q1 = 1.60; 95% CI = 1.30–1.96) and an inverse association between GL and oropharyngeal cancer (ORQ4 vs. Q1 = 0.78; 95% CI = 0.63–0.97). This pooled analysis indicates a modest positive association between GI and HNC, mainly driven by laryngeal cancer.
Similar content being viewed by others
Background
Most head and neck cancers (HNCs) are attributed to tobacco smoking and/or alcohol drinking.1 Diet has been suggested to play a role in HNC aetiology, with non-starchy vegetables and selected healthy dietary patterns being inversely related with HNC risk.2
Average daily glycaemic index (GI) ranks carbohydrate foods based on the postprandial blood glucose response; average glycaemic load (GL) estimates the impact of carbohydrate consumption using the GI, while taking into account the amount of carbohydrates that are consumed.3 Higher GI and GL are moderately associated with risk of several cancers,4 likely because of stimulation of insulin release and bioactivity of insulin-like growth factor-1, which has proliferative, angiogenic, anti-apoptotic and oestrogen stimulating properties.5
Only two studies6,7 have investigated the effect of GI and GL on HNC risk, with inconsistent findings; one of these studies6 reported results by sub-site, based, however, on a limited number of cases.
The objective of this paper is to assess the association of GI or GL with HNC and its subsites (i.e. oral cavity, oropharynx, hypopharynx and larynx) using pooled dietary data from eight case-control studies participating in the International Head and Neck Cancer Epidemiology (INHANCE) consortium.8
Methods
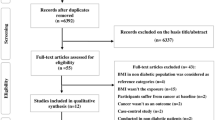
Within data version 1.5 of the INHANCE dataset, information on GI and GL was available from 3 case-control studies. In addition, we calculated GI and/or GL intakes from study-specific food items and food composition databases for another five studies, giving a total of eight studies included in the analysis. Details on individual studies and data pooling methods have been previously described8 and are summarised in Supplementary Table S1. Informed consents and institutional review board approvals were obtained within the framework of the original studies.
Selection of subjects
Cases were included if their cancer had been originally classified as invasive cancer of the oral cavity, pharynx, larynx or unspecified oral cavity/pharynx. Corresponding controls from the original studies were included in the analysis. We excluded subjects with missing information on the site of origin of cancer, or GI or GL value, and those with missing or implausible (<500 or >5500 kcal/day) non-alcohol energy intake. Thus, our analysis included 11,488 subjects, with 4081 HNC cases and 7407 controls (4264 hospital-based and 3143 population-based controls). There were 810 oral cavity, 1172 oropharynx, 343 hypopharynx, 1338 larynx and 418 unspecified oral cavity/pharynx cancer cases.
Specification of variables
Study-specific food-frequency questionnaires (FFQs) and food composition tables allowed us to calculate individual values of GI and GL for the four studies lacking information on both the exposures [Los Angeles, Boston, Seattle (1985–1995) and Memorial Sloan Kettering Cancer Center (MSKCC) studies]. In detail, as described previously,9 the GI of a food was expressed as a percentage of the glycaemic response elicited by white bread as a standard food with a GI of 100. The average daily GI for each subject was computed by summing the products of the GI value of each food times the amount of available carbohydrates in that food consumed per day, divided by the total amount of available carbohydrates (g) consumed per day. The average daily GL (g) was calculated by summing the products of the GI value of each food times the amount of available carbohydrates in that food consumed per day, divided by 100. Each GL unit represents the equivalent of 1 g of carbohydrate from white bread. Therefore, we initially converted frequencies of consumption into servings/day and servings/day into grams/day; then, we assigned the corresponding GI to each food item and applied the previous formulas to derive individual GI and GL values. For the North Carolina (2002–2006) study, information on individual values of GL was originally provided to the INHANCE Consortium Coordinating Center. We estimated GI as 100 multiplied with GL and divided by total available grams of carbohydrate intake (Supplementary Material—text and Table S2 for GI/GL calculation and study-specific GI values).
Statistical analysis
Multiple logistic regression models were used to estimate the odds ratios (ORs) of HNC and the corresponding 95% confidence intervals (CIs) according to centre-specific quartiles of GI or GL among controls (Supplementary Tables S3 for descriptive statistics of GI and GL distributions). In the presence of heterogeneity of GI or GL intakes across centres, we used a random-slope logistic regression model, whereas a fixed-effects model was used otherwise.10 The models included the following potential confounders: age, sex, race/ethnicity, study centre, education, cigarette smoking intensity, cigarette smoking duration, cigar smoking status, pipe smoking status, alcohol drinking intensity and the product term of cigarette smoking and alcohol drinking intensities. For GI, models were further adjusted for energy intake without alcohol; for GL, models were further adjusted for energy intake without alcohol and carbohydrates. For both GI and GL models, we used centre-specific control-based quartiles of energy intake. Separate analyses were carried out by HNC subsites and in strata of selected covariates. In sensitivity analyses, we further adjusted for history of diabetes or excluded subjects with diabetes (information available for 6 studies). Analyses were performed using the SAS software (version 9.4, SAS Institute, Cary, NC).
Results
Characteristics of our sample were presented in Supplementary Table S4. The highest GI quartile category (Q4) was associated with a higher HNC risk (ORQ4 vs. Q1 = 1.16; 95% CI = 1.02–1.31, ptrend = 0.037, Table 1). Across HNC subsites, GI was associated with an increased laryngeal cancer risk (ORQ4 vs. Q1 = 1.60; 95% CI = 1.30–1.96, ptrend < 0.001), but excluding laryngeal cancer cases, the ORQ4 vs. Q1 was 1.01 (95% CI = 0.88–1.16, ptrend = 0.90) (data not shown). Little associations between GL and cancers of the oral cavity, hypopharynx and larynx were observed. An inverse association was found between oropharyngeal cancer risk and GL (ORQ4 vs. Q1 = 0.78; 95% CI = 0.63–0.97, ptrend = 0.009). Results did not materially change when excluding subjects with diabetes or when additionally adjusting models by diabetes history. No heterogeneity was observed in strata of covariates (Supplementary Table S5).
Discussion
In this large dataset, we observed a positive association between GI and HNC risk, essentially driven by laryngeal cancer. GL was not associated with the risk of overall HNC or its subsites, except for a possible inverse association with oropharyngeal cancer.
Inconsistent associations of GI and GL with HNC risk may be partly due to differences in the underlying dietary patterns. Indeed, higher dietary GL is strongly associated with higher carbohydrate intakes, while a higher GI is also associated with lower intakes of dairy products, legumes, fruit and vegetables.11 In line with this hypothesis, an overlapping INHANCE-based analysis including seven of the eight current studies showed a positive association of laryngeal cancer with an “Animal products and cereals” dietary pattern, which was simultaneously based on high-GI (e.g. cereals) and low-GL (e.g. meat) foods.10
Only two previous studies6,7 have examined the association between GI or GL and HNC risk, with one of them partially overlapping with the current dataset.6 An analysis6 of three Italian case-control studies on upper aero-digestive tract cancers reported a positive association with higher GI (ORQ5 vs. Q1 = 1.5; 95% CI = 1.1–2.0) and GL (ORQ5 vs. Q1 = 1.8; 95% CI = 1.1–2.9) in quintiles. Although in the same direction, the association was weaker with oral and pharyngeal cancers combined or laryngeal cancer.6 Findings from the National Institutes of Health–AARP Diet and Health Study (1239 HNC cases; 446,177 participants) reported a null association with GI and a possible inverse association with GL in women (ORQ5 vs. Q1 = 0.63; 95% CI = 0.34–1.19), in the absence of a clear dose-response relationship.7
Limitations of the current analyses included possible recall bias and non-differential misclassification of GI/GL quartiles. In addition, food items contributing to GI differed in part across regions (Supplementary Table S2). However, all our FFQs were either reproducible and valid or were modifications of existing FFQs, already tested for reproducibility and validity. We were able to adjust for major potential confounders and our large sample size provided the necessary statistical power to examine the association in HNC subsites and strata.8
In conclusion, findings from this large-scale pooled analysis support a positive effect of average daily GI on the risk of HNC, and in particular of laryngeal cancer.
References
Anantharaman, D., Marron, M., Lagiou, P., Samoli, E., Ahrens, W., Pohlabeln, H. et al. Population attributable risk of tobacco and alcohol for upper aerodigestive tract cancer. Oral. Oncol. 47, 725–731 (2011).
Su, H. I., Sammel, M. D., Velders, L., Horn, M., Stankiewicz, C., Matro, J. et al. Association of cyclophosphamide drug-metabolizing enzyme polymorphisms and chemotherapy-related ovarian failure in breast cancer survivors. Fertil. Steril. 94, 645–654 (2010).
Augustin, L. S., Kendall, C. W., Jenkins, D. J., Willett, W. C., Astrup, A., Barclay, A. W. et al. Glycemic index, glycemic load and glycemic response: an International Scientific Consensus Summit from the International Carbohydrate Quality Consortium (ICQC). Nutr. Metab. Cardiovasc. Dis. 25, 795–815 (2015).
Turati, F., Galeone, C., Augustin, L. S. A., La Vecchia, C. Glycemic index, glycemic load and cancer risk: an updated meta-analysis. Nutrients 11, pii: E2342, https://doi.org/10.3390/nu11102342 (2019).
Biddinger, S. B. & Ludwig, D. S. The insulin-like growth factor axis: a potential link between glycemic index and cancer. Am. J. Clin. Nutr. 82, 277–278 (2005).
Augustin, L. S., Gallus, S., Franceschi, S., Negri, E., Jenkins, D. J., Kendall, C. W. et al. Glycemic index and load and risk of upper aero-digestive tract neoplasms (Italy). Cancer Causes Control. 14, 657–662 (2003).
George, S. M., Mayne, S. T., Leitzmann, M. F., Park, Y., Schatzkin, A., Flood, A. et al. Dietary glycemic index, glycemic load, and risk of cancer: a prospective cohort study. Am. J. Epidemiol. 169, 462–472 (2009).
Edefonti, V., Hashibe, M., Parpinel, M., Turati, F., Serraino, D., Matsuo, K. et al. Natural vitamin C intake and the risk of head and neck cancer: a pooled analysis in the International Head and Neck Cancer Epidemiology Consortium. Int. J. Cancer 137, 448–462 (2015).
Hu, J., La Vecchia, C., Augustin, L. S., Negri, E., de Groh, M., Morrison, H. et al. Glycemic index, glycemic load and cancer risk. Ann. Oncol. 24, 245–251 (2013).
De Vito, R., Lee, Y. C. A., Parpinel, M., Serraino, D., Olshan, A. F., Zevallos, J. P. et al. Shared and study-specific dietary patterns and head and neck cancer risk in an International Consortium. Epidemiology 30, 93–102 (2019).
Mendez, M. A., Covas, M. I., Marrugat, J., Vila, J. & Schroder, H. Glycemic load, glycemic index, and body mass index in Spanish adults. Am. J. Clin. Nutr. 89, 316–322 (2009).
Acknowledgements
The authors would like to thank Marta Rossi for her useful suggestions in performing the statistical analysis on GI and GL.
Author information
Authors and Affiliations
Contributions
C. Chang contributed to write, review and/or revision of the manuscript; Y.A.L. contributed to the acquisition of the pooled data; C. Chang contributed to the analysis, and V.E. performed statistical support; C.L.V., V.E., F.T. and Z.Z. contributed substantially to the interpretation of data and were involved in drafting and revising the manuscript; D.S., A.F.O., J.P.Z., Z.Z., H.M., C.L.V., F.L., W.G., K.K., M.M., C. Chen, S.M.S., S.S. and G.Y. conducted research and provided single-study databases; L.S.A.A. and M.P. provided advice on nutritional issues; P.B., Y.A.L. and M.H. are the INHANCE study coordinators; all authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Informed consent and institutional review board approval were obtained within the framework of the original studies, according to the rules existing at the time of data collection. In addition, a central Institutional Review Board approval was obtained from the University of Utah, #42912.
Consent to publish
Not applicable.
Data availability
The dataset used and analysed during the current study is available from the corresponding author on reasonable request.
Competing interests
The authors declare no competing interests.
Funding information
The INHANCE Pooled Data Project was supported by grants from the National Institutes of Health (NIH), National Cancer Institute (NCI) [R03CA113157], and National Institute of Dental and Craniofacial Research (NIDCR) [R03DE016611]. Individual studies were funded by the following grants: (1) Italy multicenter study: Italian Association for Research on Cancer (AIRC), Italian League Against Cancer and Italian Ministry of Research; (2) North Carolina (2002–2006) study: NCI [R01CA90731–01] and National Institute of Environmental Health Sciences (NIEHS) [P30ES010126]; (3) Los Angeles study: NIH [P50CA090388, R01DA011386, R03CA077954, T32CA009142, U01CA096134 and R21ES011667] and the Alper Research Program for Environmental Genomics of the UCLA Jonsson Comprehensive Cancer Center; (4) Swiss study: Swiss League against Cancer and the Swiss Research against Cancer/Oncosuisse [KFS-700, OCS-1633]; (5) Milan (2006–2009) study: AIRC and Italian Ministry of Education [PRIN 2009 X8YCBN]; (6) Boston study: NIH [R01CA078609 and R01CA100679]; (7) Seattle (1985–1995) study: NIH [R01CA048996 and R01DE012609]; (8) MSKCC study: NIH [R01CA051845].
Additional information
Note This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution 4.0 International (CC BY 4.0).
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chang, CP., La Vecchia, C., Serraino, D. et al. Dietary glycaemic index, glycaemic load and head and neck cancer risk: a pooled analysis in an international consortium. Br J Cancer 122, 745–748 (2020). https://doi.org/10.1038/s41416-019-0702-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-019-0702-4
This article is cited by
-
Dietary glycemic index, glycemic load and cancer risk: a meta-analysis of prospective cohort studies
European Journal of Nutrition (2022)