Abstract
Objective
The objective is to compare new bone formation in critical defects in healthy, diabetic, and osteoporotic rats filled with hydroxyapatite (HA) alone and HA combined with simvastatin (SV).
Materials and methods
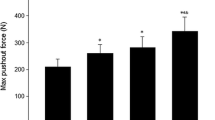
A total of 48 adult female Sprague-Dawley rats were randomized into three groups (n = 16 per group): Group, 1 healthy; Group 2, diabetics; and Group 3, osteoporotics. Streptozotocin was used to induce type 1 diabetes in Group 2, while bilateral ovariectomy was used to induce osteoporosis in Group 3. The central portion of the rat mandibular symphysis was used as a physiological critical bone defect. In each group, eight defects were filled with HA alone and eight with HA combined with SV. The animals were sacrificed at 4 and 8 weeks, and the mandibles were processed for micro-computed tomography to analyze radiological union and bone mineral density (BMD); histological analysis of the bone union; and immunohistochemical analysis, which included immunoreactivity of vascular endothelial growth factor (VEGF) and bone morphogenetic protein 2 (BMP-2).
Results
In all groups (healthy, diabetics, and osteoporotics), the defects filled with HA + SV presented greater radiological bone union, BMD, histological bone union, and more VEGF and BMP-2 positivity, in comparison with bone defects treated with HA alone.
Conclusions
Combined application of HA and SV improves bone regeneration in mandibular critical bone defects compared with application of HA alone in healthy, diabetic, and osteoporotic rats.
Clinical relevance
This study might help to patients with osteoporosis or uncontrolled diabetes type 1, but future studies should be done.




Similar content being viewed by others
References
Cacaci C, Ackermann KL, Barth T, Kistler S, Stiller M, Schlee M (In press) A non-interventional multicenter study to document the implants success and survival rates in daily dental practices of the CONELOG screw-line implant. Clin Oral Investig.
Guijarro-Martínez R, Miragall Alba L, Marqués Mateo M, Puche Torres M, Pascual Gil JV (2011) Autologous fat transfer to the cranio-maxillofacial region: updates and controversies. 39:359-363
Huang YF, Chang CT, Muo CH, Hong HH, Shen YF, Lin CC et al (2018) The association of variables of fibular reconstructed mandible and bite force in oral cancer patients with dental implant rehabilitation. J Craniomaxillofac Surg 46:1979–1983
Maddalone M, Mirabelli L, Venimo PM, Karanxha L, Porcaro G, Del Fabbro M (2018) Long-term stability of autologous bone graft of intraoral origin after lateral sinus floor elevation with simultaneous implant placement. Clin Implant Dent Relat Res 20:713–721
Raghoebar GM, Meijndert L, Kalk WW, Vissink A (2007) Morbidity of mandibular bone harvesting: a comparative study. Int J Oral Maxillofac Implants 22:359–365
Johansson B, Grepe A, Wannfors K, Hirsch JM (2001) A clinical study of changes in the volume of bone grafts in the atrophic maxilla. Dentomaxillofac Radiol 30:157–161
John HD, Wenz B (2004) Histomorphometric analysis of natural bone mineral for maxillary sinus augmentation. Int J Oral Maxillofac Implants 19:199–207
Rojbani H, Nyan M, Ohya K, Kasugai S (2011) Evaluation of the osteoconductivity of α-tricalcium phosphate, β-tricalcium phosphate, and hydroxyapatite combined with or without SV in rat calvarial defect. J Biomed Mater Res A 98:488–498
Shetty V, Han TJ (1991) Alloplastic materials in reconstructive periodontal surgery. Dent Clin North Am 35:521–530
Rey C (1990) Calcium phosphate biomaterials and bone mineral. Differences in composition, structures and properties. Biomaterials 11:13–15
Heinz B, Kasaj A, Teich M, Jepsen S (2010) Clinical effecs of nanocrystalline hydroxyapatite paste in the treatment of intraboy periodontal defects: a randomized clinical study. Clin Oral Investig 14:525–531
Rodríguez A, Anastasov GE, Lee H, Buchbinder D, Wettan H (2003) Maxillary sinus augmentation with deproteinated bovine bone and palatet rich plasma with simultaneous insertion of endosseus implants. Int J Oral Maxillofac Surg 61:157–163
Klinge B, Alberius P, Isaksson S, Jönsson J (1992) Osseous response to implanted natural bone and synthetic hydroxyapatite ceramic in the repair of experimental skulls bone defects. J Oral Maxillofac Surg 50:241–249
Thaller SR, Hoyt J, Dart A, Bojerson K, Tesluk H (1994) Repair of experimental calvarial defects with Bio-Oss particles and collagen sponges in a rabbit model. J Craniofac Surg 5:242–246
Hallman M, Lundgren S, Sennerby L (2001) Histologic analysis of clinical biopsies taken 6 months and 3 years after maxillary sinus floor augmentation with 80% bovine hydroxyapatite and 20% autogenous bone mixed with fibrin glue. Clin Implant Dent Relat Res 3:87–96
Slotte C, Lundgren D, Burgos PM (2003) Placement of autogenic bone chips or bovine one mineral in guided bone augmentation: a rabbit skull study. Int J Oral Maxillofac Implants 18:795–806
Taschieri S, Corbella S, Weinstein R, Di Giancamillo A, Mortellaro C, Del Fabbro M (2016) Maxillary Sinus Floor Elevation Using Platelet-Rich Plasma Combined With Either Biphasic Calcium Phosphate or Deproteinized Bovine Bone. J Craniofac Surg 27:702–707
DurmuŞlar MC, Alpaslan C, Alpaslan G, Çakır M (2014) Clinical and radiographic evaluation of the efficacy of platelet-rich plasma combined with hydroxyapatite bone graft substitutes in the treatment of intra-bony defects in maxillofacial region. Acta Odontol Scand 72:948–953
Wu S, Xiao Z, Song J, Li M, Li W (2018) Evaluatioin of BMP-2 Enhances the Osteoblast Differentiation of Human Ammion Mesenchymal Stem Cells Seeded on Nano-Hydroxyapatite/Collagen/Poly(L-Lactide). Int J Mol Sci 25(19):E2171
Wang G, Roohani-Esfahani SI, Zhang W, Lv K, Yang G, Ding X et al (2017) Effects of Sr-HT-Gahnite on osteogenesis and angiongenesis by adipose derived stem cells for critical-sized calvarial defect repair. Sci Rep 20:41135
Wang M, Sa Y, Li P, Guo Y, Du Y, Deng H et al (2018) A versatile and injectable ply(methyl methacrylate) cement functionalized with quaternized chitosan-glycerophosphate/nanosized hydroxyapatite hydrogels. Mater Sci Eng C Mater Biol Appl 90:264–272
Iqbal H, Ali M, Zeeshan R, Mutahir Z, Iqbal F, Nawaz MAH (2017) Chitosan/hydrozyapatite (HA)/hydroxypropylmethyl cellulose (HPMC) spongy scaffolds-synthesis and evaluation as potential alveolar bone substitutes. Colloids Surf B Biointerfaces 160:553.563
Chu C, Deng J, Man Y, Qu Y (2017) Evaluation of nanohydroxyapatite (nano-HA) coated epigallocatechin-3-gallete (EGCG) cross-linked collagen membranes. Mater Sci Eng C Mater Biol Appl 78:258–264
Ma X, He Z, Han F, Zhong Z, Chen L, Li B (2016) Preparation of collagen/hydroxyapatite/alendronate hybrid hydrogles as potential scaffolds for bone regeneration. Colloids Surf B Biointerfaces 142:81–87
Pradeep AR, Karvekar S, Nagpal K, Patnaik K, Rajau A, Singh P (2016) Rosuvastatin 1.2 mg In Situ Gel Combined With 1:1 Mixture of Autologous Platelet-Rich Fibrin and Porous Hydroxyapatite Bone Graft in Surgical Treatment of Mandibular Class II Furcation Defects: A randomized Clinical Control Trial. J Periodontol 87:5–13
Li Y, Zhang Z, Zhang Z (2018) Porous Chitosan/Nano-Hydroxyapatite Composite Scaffolds Incorporing SV-Loaded PLGA Microspheres for Bone Repair. Cells Tissues Organs 205:20–31
Hao J, Chou J, Kuroda S, Otsuka M, Kasugai S, Lang NP (2018) Injectable SV gel for minimally invasive periosteal distraction: In vitro and in vivo studies in rat. Clin Oral Implants Res 29:227–234
Shahrezaine M, Moshiri A, Shekarchi B, Oryan A, Maffulli N, Parvizi J (2018) Effectiveness of tissue engineered three-dimensional bioactive graft on bone healing and regeneration: an in vivo study with significant clinical value. J Tissue Eng Regen Med 12:936–960
Yu WL, Sun TW, Qi C, Zhao HK, Ding ZY, Zhang ZW (2017) Enhanced osteogenesis and angiogenesis by mesoporous hydroxyapatitie microspheres-derived SV sustained release system for superior bone regeneration. Sci Rep 7:44129
Tao ZS, Zhou WS, Bai BL, Cui W, Lv YX, Yu XB et al (2016) The effects of combined human parathyroid hormone (1-34) and SV treatment on the interface of hydroxyapatite-coated titanium rods implanted into osteopenic rats femurs. J Mater Sci Mater Med 27:43
Papadimitriou K, Karkavelas G, Vouros I, Kessopoulou E, Konstantinidis A (2015) Effects of local application of SV on bone regeneration in femoral bone defects in rabbit. J Craniomaxillofac Surg 43:232–237
Shah SR, Werlang CA, Kasper FK, Mikos AG (2015) Novel applications of statins for bone regeneration. Natl Sci Rev 2:85–99
Jamal SM, Eisenberg MJ, Christopoulos S (2004) Rhabdomyolysis associated with hydroxymethylglutaryl-coenzyme A reductase inhibitors. Am Heart J 147:956–965
Maeda T, Kawane T, Horiuchi N (2003) Statins augment vascular endothelial growth factor expression in osteoblastic cells via inhibition of protein penylation. Endocrinology 144:681–692
Nyan M, Sato D, Kihara H, Machida T, Ohya K, Kasugai S (2009) Effects of combination with alpha-tricalcium phosphate and SV on bone regeneration. Clin Oral Implants Res 20:280–287
Tylin MR, McConnell JC, Schmid MJ, Reckling RR, Ojha J, Bhattacharyya I et al (2002) Effects of SV gels on murine calvarial bone. J Periodontol 73:1141–1148
Ezirganlı Ş, Kazancıoğlu HO, Mihmanlı A, Aydın MŞ, Sharifov R, Alkan A (2014) The effect of local SV application on critical size defects in the diabetic rats. Clin Oral Implants Res 25:969–976
Zhang Q, Jing D, Zhang Y, Miron RJ (2018) Histomorphometric study of Study of New Bone Formation Comparing Defect Healing with Three Bone Grafting Materials: The Effect of Osteoporosis on Graft Consolidation. Int J Oral Maxillofac Implants 33:645–652
da Cunha MR, Gushiken V, Mardegan Issa JP, Iatecola A, Pettian M, Santos AR Jr (2011) Osteoconductive capacity of hydroxyapatite implanted into the skull of diabetics. J Craniofac Surg 22:2048–2052
Olei L, Rivadeneira F, Zillikens MC, Oei EH (2015) Diabetes, diabetic complications, and fracture risk. Curr Osteoporos Rep 13:106–115
Antonopoulou M, Bahtiyar G, Banerji MA, Sacerdote AS (2013) Diabetes and bone health. Maturitas 76:253–259
Starup-Linde J (2013) Diabetes, biochemical markers of bone turnover, diabetes control, and bone. Front Endocrinol (Lausanne) 4:21
Pacifici R (1996) Estrogen cytokines, and pathogenesis of postmenopausal osteoporosis. J Bone Mier Res 11:1043–1051
von Wowern N (2001) General and oral aspects of osteoporosis: a review. Clin Oral Investig 5:71–82
Liu X, Bao C, Xu HHK, Pan J, Hu J, Wang P et al (2016) Osteoprotegerin gene-modified BMSCs with hydroxyapatite scaffold for treating critical-sized mandibular defects in ovarectomized osteoporotic rats. Acta Biomater 42:378–388
Schmitz JP, Hollinger JO (1986) The critical size defect as an experimental model for craniomandibulofacial nonunions. Clin Orthop Relat Res 205:299–308
Yagyuu T, Kirita T, Hattori K, Tadokoro M, Ohgushi H (2015) Unique and reliable rat model for the assessment of cell therapy: bone unión in the rat mandibular symphysis using bone marrow stromal cells. J Tissue Eng Regen Med 9:276–285
Ueyama Y, Yagyuu T, Maeda M, Imada M, Akahane M, Kawate K (2016) Maxillofacial bone regeneration with osteogenic matrix cell sheets: An experimental study in rats. Arch Oral Biol 72:138–145
Nascimento-Saba CC, Breitenbach MM, Rosenthal D (1997) Pituitary-thyroid axis in short- and long-term experimental diabetes mellitus. Braz J Med Biol Res 30:269–274
Barbirato DDS, Fogacci MF, Gusman H, Takiya CM, Carvalho DP, Samsone C (2018) Hydroxyapatite calvaria graft repair in experimental diabetes mellitus in rats. J Craniomaxillofac Surg 46:1576–1585
Kidder LS, Chen X, Schmidt AH, Lew WD (2009) Osteogenic protein-1 overcomes inhibition of fracture healing in the diabetic rat: a pilor study. Clin Orthop Relat Res 467:3249–3256
Zhang Y, Cheng N, Miron R, Shi B, Cheng X (2012) Delivery of PDGF-B and BMP-7 by mesoporous bioglass/silk fibriin scaffolds for the repair of osteoporotic defects. Biomaterials 33:6698–6708
Oliveira GR, Vargas-Sanchez PK, Fernandes RR, Ricoldi MST, Semeghini MS, Pitol DL et al (In press) Lycopene influences osteoblast functioinal activity and prevents femur bone loss in female rats submitted to an experimental model of osteoporosis. J Bone Miner Metab.
van Houdt CIA, Ulrich DJO, Jansen JA, van den Beuchen JJJP (2016) The performance of CPC/PLGA and Bio-Oss® for bone regeneration in healthy and osteoporotic rats. J Biomed Mater Res B Appl Biomater 106:131–142
Nyan M, Miyahara T, Noritake K, Hao J, Rodriguez R, Kuroda S et al (2010) Molecular and tissue responses in the healing of rat calvarial defects after local application of SV combined with alpha tricalcium phosphate. J Biomed Mater Res B Appl Biomater 93:65–73
Camacho-Alonso F, Davia-Peña RS, Vilaplana-Vivo C, Tudela-Mulero MR, Merino JJ, Martínez-Beneyto Y (2018) Synergistic effect of photodynamic therapy and alendronate on alveolar bone loss in rats with ligature-induced periodontitis. J Periodontal Res 53:306–314
Salkeld SL, Patron LP, Barrack RL, Cook SD (2001) The effect of osteogenic protein-1 on the healing of segmental bone defects treated with autograft or allograft bone. J Bone Joint Surg Am 83A:803–816
Gothard D, Smith EL, Kanczler JM, Rashidi H, Qutachi O, Henstock J et al (2014) Tissue engineered bone using select growth factors: A comprehensive review of animal studies and clinical translation studies in man. Eur Cell Mater 28:166–207
Pilia M, Guda T, Appleford M (2013) Development of composite scaffolds for load-bearing segmental bone defects. Biomed Res Int 2013:458253
O’Loughlin PF, Morr S, Bogunovic L, Kim AD, Park B, Lane JM (2008) Selection and development of preclinical models in fracture-healing research. J Bone Joint Surg Am 90:79–84
Pinheiro FA, Mourão CF, Diniz VS, Silva PC, Meirelles L, Santos Junior E et al (2014) IN-vivo bone response to titanium screw implants anodized in sodium sulfate. Acta Cir Bras 29:376–382
Malhotra A, Pelletier MH, Yu Y, Christou C, Walsh WR (2014) A sheep model for cancellous bone healing. Front Surg 1:37
van Houdt CIA, Ulrich DJO, Jansen JA, van den Beucken JJJP (2018) The performance of CPC/PLGA and Bio-Oss® for bone regeneration in healthy and osteoporotic rats. J Biomed Mater Res B Appl Biomater 106:131–142
Schortinghuis J, Ruben JL, Raghoebar GM, Stegenga B (2004) Ultrasound to stimulate mandibular bone defect healing: a placebo-controlled single-blind study in rats. J Oral Maxillofac Surg 62:194–201
Park JB (2009) The use of simvastatin in bone regeneration. Med Oral Patol Oral Cir Bucal 14:e485–e488
Gutierrez GE, Lalka D, Garrett IR, Rossini G, Mundy GR (2006) Transdermal application of lovastatin to rats causes profound increases in bone formation and plasma concentrations. Ostoporosis Int 17:1033–1042
Fernández-Tresguerres-Hernández-Gil I, Alobera-Gracia MA, del-Canto-Pingarrón M, Blanco-Jerez L (2006) Physiological bases of bone regeneration I. Histology and physiology of bone tissue. Med Oral Patol Oral Cir Bucal 11:E47–E51
Mellado-Valero A, Ferrer-García JC, Calvo-Catalá J, Labaig-Rueda C (2010) Implant treatment in patients with osteoporosis. Med Oral Patol Oral Cir Bucal 15:e52–e57
Fang W, Zhao S, He F, Liu L, Yang G (2015) Influence of simvastatin-loaded implants on osseointegration in an ovarectomized animal model. Biomed Res Int 2015:831504
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The procedures and study protocol described here were approved by the University of Murcia Bioethics Committee (Spain) and the competent authority (A13160607).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Camacho-Alonso, F., Martínez-Ortiz, C., Plazas-Buendía, L. et al. Bone union formation in the rat mandibular symphysis using hydroxyapatite with or without simvastatin: effects on healthy, diabetic, and osteoporotic rats. Clin Oral Invest 24, 1479–1491 (2020). https://doi.org/10.1007/s00784-019-03180-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-019-03180-9