Abstract
Background
The present consensus suggests urgent surgical decompression if clinical features of cauda equina syndrome (CES) are supported by MRI evidence of pressure on cauda equina. However, clinical diagnosis has a high false-positive rate and MRI is a poor indicator. Though urodynamic studies (UDS) provide objective information about the lower urinary tract symptoms experienced by patients including neurogenic bladder, its role in the diagnosis of CES is not established.
Objective
To evaluate the ability of an objective urological assessment protocol using uroflowmetry + USG-PVR as screening test and invasive UDS as confirmatory test in patients with suspected CES to rule out neurological impairment of the bladder function.
Methods
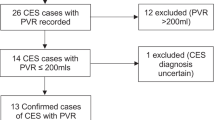
A retrospective study was conducted on all patients who were referred to our institution with equivocal findings of cauda equina syndrome from January 2014 to December 2018 with positive MRI findings. An algorithm using multichannel UDS was followed in all the included patients.
Results
Out of 249 patients who fulfilled the inclusion criteria, 34 patients (13.65%) had normal uroflowmetry and USG-PVR findings; 211 patients underwent the invasive UDS. Only 141(57.6%) patients out of 245 patients had neurovesical involvement due to compression of cauda equina; 67 patients were treated conservatively using the objective protocol. Only one patient treated conservatively had to undergo emergency decompression for deterioration in symptoms.
Conclusions
Multichannel UDS provides an objective diagnostic tool to definitively establish the neurovesical involvement in CES. Utilising multichannel UDS as an adjunct to clinical findings avoids the probability of false-positive diagnosis of CES.
Graphic abstract
These slides can be retrieved under Electronic Supplementary Material.







Similar content being viewed by others
References
Lavy C, James A, Wilson-MacDonald J, Fairbank J (2009) Cauda equina syndrome. BMJ 338:b936. https://doi.org/10.1136/bmj.b936
Schoenfeld AJ, Bader JO (2012) Cauda equina syndrome: an analysis of incidence rates and risk factors among a closed North American military population. Clin Neurol Neurosurg 114:947–950
Deniz K, Pararajasingham J (2011) Cauda Equina Syndrome. InnovAiT Educ Inspir Gen Pract 4(10):551–555. https://doi.org/10.1093/innovait/inq205
Todd NV (2015) Cauda equina syndrome: Is the current management of patients presenting to district general hospitals fit for purpose? A personal view based on a review of the literature and a medicolegal experience. Bone Joint J 97(B):1390–1394
Bell DA, Collie D, Statham PF (2007) Cauda equina syndrome: what is the correlation between clinical assessment and MRI scanning? Br J Neurosurg 21:201–203
Balasubramanian K, Kalsi P, Greenough CG, Kuskoor Seetharam MP (2010) Reliability of clinical assessment in diagnosing cauda equina syndrome. Br J Neurosurg 24:383–386
Domen PM, Hofman PA, van Santbrink H, Weber WE (2009) Predictive value of clinical characteristics in patients with suspected cauda equina syndrome. Eur J Neurol 16:416–419
Boos N, Reider R, Schade V, Spratt KF, Semmer N, Aebi M (1995) The diagnostic accuracy of magnetic resonance imaging, work perception, and psychosocial factors in identifying symptomatic disc herniations. Spine 20:2613–2625
Ahn UM, Ahn NU, Buchowski JM, Garrett ES, Sieber AN, Kostuik JP (2000) Cauda equina syndrome secondary to lumbar disc herniation: a meta-analysis of surgical outcomes. Spine 25:1515–1522
Podnar S (2010) Cauda equina lesions as a complication of spinal surgery. Eur Spine J 19:451–457. https://doi.org/10.1007/s00586-009-1170-y
Venkatesan M, Nasto L, Grevitt MP, Tsegaye MM (2017) Is post-void bladder scan a useful adjunct to the clinical examination for prediction of cauda equine syndrome? Spine J 17(3):S7. https://doi.org/10.1016/j.spinee.2016.12.021
Yamanishi T, Yasuda K, Yuki T, Sakakibara R, Uchiyama T, Kamai T et al (2003) Urodynamic evaluation of surgical outcome in patients with urinary retention due to central lumbar disc prolapse. Neurourol Urodyn 22:670e5
Alan G, Edward G, Tim M (2011) Cauda equina syndrome: a review of the current clinical and medico-legal position. Eur Spine J 20(5):690–697. https://doi.org/10.1007/s00586-010-1668-3
Greenhalgh S, Finucane L, Mercer C, Selfe J (2018) Assessment and management of cauda equina syndrome. Musculoskelet Sci Pract 37:69–74. https://doi.org/10.1016/j.msksp.2018.06.002
Fairbank J, Hashimoto R, Dailey A, Patel AA, Dettori JR (2011) Does patient history and physical examination predict MRI proven cauda equina syndrome? Evid Based Spine Care J. 2(4):27–33
Janardhana AP, Rajagopal RS, Kamath A (2010) Correlation between clinical features and magnetic resonance imaging findings in lumbar disc prolapse. Indian J Orthop 44(3):263–269. https://doi.org/10.4103/0019-5413.65148
McCarthy MJH, Brodie AT, Annesley-Williams D et al (2006) MRI measurements in cauda equina syndrome: reproducibility and prediction of clinical outcome. J Bone Joint Surg Br 88-B(Supp II):218–219
Qureshi A, Sell P (2007) Cauda equina syndrome treated by surgical decompression: the influence of timing on surgical outcome. Eur Spine J 16(12):2143–2151
Schäfer W, Abrams P, Liao L, Mattiasson A, Pesce F, Spangberg A, International Continence Society et al (2002) Good urodynamic practices: uroflowmetry filling cystometry, and pressure-flow studies. Neurourol Urodyn 21:26174
Yamanishi T, Sakakibara R, Uchiyama T, Hirata K (2011) Role of urodynamic studies in the diagnosis and treatment of lower urinary tract symptoms. Urol Sci 22(3):120–128. https://doi.org/10.1016/j.urols.2011.08.007
Kelly CE (2004) Evaluation of voiding dysfunction and measurement of bladder volume. Rev Urol 6(Suppl 1):S32–S37
Griffiths D, Hofner K, van Mastrigt R et al (1997) Standardization of terminology of lower urinary tract function: pressure-flow studies of voiding, urethral resistance, and urethral obstruction. Neurourol Urodyn 16:1–18
George NJR (1990) Clinical uroflowmetry. In: O’Reilly PH, George NJR, Weiss RM (eds) Diagnostic techniques in urology. WB Saunders, Philadelphia
Alothmany N, Mosli H, Shokoueinejad M, Alkashgari R, Chiang M, Webster JG (2018) Critical review of uroflowmetry methods. J Med Biol Eng. https://doi.org/10.1007/s40846-018-0375-0
Abrams PH, Dunn M, George N (1978) Urodynamic findings in chronic retention of urine and their relevance to results of surgery. BMJ 2(6147):1258–1260. https://doi.org/10.1136/bmj.2.6147.1258
Weiss BD (1998) Diagnostic evaluation of urinary incontinence in geriatric patients. Am Fam Phys 57(11):2675–2684
Acknowledgement
The authors would like to thank the concerned patients for allowing the details to be shared.
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The place of study accepts retrospective clinical record evaluation without ethical approval.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kalidindi, K.K.V., Chhabra, H.S., Suman, D. et al. Cauda equina syndrome: false-positive diagnosis of neurogenic bladder can be reduced by multichannel urodynamic study. Eur Spine J 29, 1236–1247 (2020). https://doi.org/10.1007/s00586-019-06277-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-019-06277-7