Abstract
Background
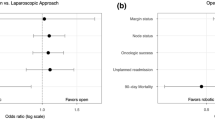
While the ACOSOG and ALaCaRT trials found that laparoscopic resections for rectal cancer failed to demonstrate non-inferiority of pathologic outcomes when compared with open resections, the COLOR II and COREAN studies demonstrated non-inferiority of clinical outcomes, leading to uncertainty regarding the value of minimally invasive (MIS) techniques in rectal cancer surgery. We analyzed differences in pathologic and clinical outcomes between open versus MIS resections for rectal cancer.
Methods
We identified patients who underwent resection for stage II or III rectal adenocarcinoma from the National Cancer Database (2010–2015). Surgical approach was categorized as open or MIS (laparoscopic or robotic). Logistic regression and Cox proportional hazard analysis were used to assess differences in outcomes and survival. Analysis was performed in an intention-to-treat fashion.
Results
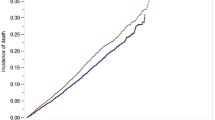
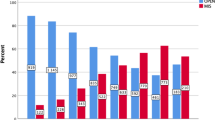
A total of 31,190 patients who underwent rectal adenocarcinoma resection were identified, of whom 52.8% underwent open resection and 47.2% underwent MIS resection (31.0% laparoscopic, 16.2% robotic). After adjustment for patient, tumor, and institutional characteristics, MIS approaches were associated with significantly decreased risk of positive circumferential resection margins (OR 0.82, 95% CI 0.72–0.94), increased likelihood of harvesting ≥ 12 lymph nodes (OR 1.12, 95% CI 1.04–1.21), shorter length of stay (OR 0.57, 95% CI 0.53–0.62), and improved overall survival (HR 0.90, 95% CI 0.83–0.98).
Conclusions
MIS approaches to rectal cancer resection were associated with improved pathologic and clinical outcomes when compared to the open approach. In this nationwide, facility-based sample of cancer cases in the United States, our data suggest superiority of MIS techniques for rectal cancer treatment.



Similar content being viewed by others
References
Clinical Outcomes of Surgical Therapy Study G, Nelson H, Sargent DJ, Wieand HS, Fleshman J, Anvari M, Stryker SJ, Beart RW Jr, Hellinger M, Flanagan R Jr, Peters W, Ota D (2004) A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350:2050–2059
Moghadamyeghaneh Z, Phelan M, Smith BR, Stamos MJ (2015) Outcomes of open, laparoscopic, and robotic abdominoperineal resections in patients with rectal cancer. Dis Colon Rectum 58:1123–1129
Jayne DG, Guillou PJ, Thorpe H, Quirke P, Copeland J, Smith AM, Heath RM, Brown JM, Group UMCT (2007) Randomized trial of laparoscopic-assisted resection of colorectal carcinoma: 3-year results of the UK MRC CLASICC Trial Group. J Clin Oncol 25:3061–3068
Colon Cancer Laparoscopic or Open Resection Study G, Buunen M, Veldkamp R, Hop WC, Kuhry E, Jeekel J, Haglind E, Pahlman L, Cuesta MA, Msika S, Morino M, Lacy A, Bonjer HJ (2009) Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol 10:44–52
Fleshman J, Branda M, Sargent DJ, Boller AM, George V, Abbas M, Peters WR Jr, Maun D, Chang G, Herline A, Fichera A, Mutch M, Wexner S, Whiteford M, Marks J, Birnbaum E, Margolin D, Larson D, Marcello P, Posner M, Read T, Monson J, Wren SM, Pisters PW, Nelson H (2015) Effect of laparoscopic-assisted resection vs open resection of stage II or III rectal cancer on pathologic outcomes: the ACOSOG Z6051 randomized clinical trial. JAMA 314:1346–1355
Stevenson AR, Solomon MJ, Lumley JW, Hewett P, Clouston AD, Gebski VJ, Davies L, Wilson K, Hague W, Simes J, Investigators AL (2015) Effect of laparoscopic-assisted resection vs open resection on pathological outcomes in rectal cancer: the ALaCaRT randomized clinical trial. JAMA 314:1356–1363
Bonjer HJ, Deijen CL, Abis GA, Cuesta MA, van der Pas MH, de Lange-de Klerk ES, Lacy AM, Bemelman WA, Andersson J, Angenete E, Rosenberg J, Fuerst A, Haglind E, Group CIS (2015) A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med 372:1324–1332
Jeong SY, Park JW, Nam BH, Kim S, Kang SB, Lim SB, Choi HS, Kim DW, Chang HJ, Kim DY, Jung KH, Kim TY, Kang GH, Chie EK, Kim SY, Sohn DK, Kim DH, Kim JS, Lee HS, Kim JH, Oh JH (2014) Open versus laparoscopic surgery for mid-rectal or low-rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): survival outcomes of an open-label, non-inferiority, randomised controlled trial. Lancet Oncol 15:767–774
Deyo RA, Cherkin DC, Ciol MA (1992) Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 45:613–619
Fleshman J, Branda ME, Sargent DJ, Boller AM, George VV, Abbas MA, Peters WR Jr, Maun DC, Chang GJ, Herline A, Fichera A, Mutch MG, Wexner SD, Whiteford MH, Marks J, Birnbaum E, Margolin DA, Larson DW, Marcello PW, Posner MC, Read TE, Monson JRT, Wren SM, Pisters PWT, Nelson H (2018) Disease-free survival and local recurrence for laparoscopic resection compared with open resection of stage II to III rectal cancer: follow-up results of the ACOSOG Z6051 randomized controlled trial. Ann Surg 269:589–595
Stevenson ARL, Solomon MJ, Brown CSB, Lumley JW, Hewett P, Clouston AD, Gebski VJ, Wilson K, Hague W, Simes J, Australasian Gastro-Intestinal Trials Group Ai (2018) Disease-free survival and local recurrence after laparoscopic-assisted resection or open resection for rectal cancer: the Australasian laparoscopic cancer of the rectum randomized clinical trial. Ann Surg 269:596–602
Zhu XL, Yan PJ, Yao L, Liu R, Wu DW, Du BB, Yang KH, Guo TK, Yang XF (2018) Comparison of short-term outcomes between robotic-assisted and laparoscopic surgery in colorectal cancer. Surg Innov. https://doi.org/10.1177/1553350618797822
Rouanet P, Bertrand MM, Jarlier M, Mourregot A, Traore D, Taoum C, de Forges H, Colombo PE (2018) Robotic versus laparoscopic total mesorectal excision for sphincter-saving surgery: results of a single-center series of 400 consecutive patients and perspectives. Ann Surg Oncol 25:3572–3579
Jayne D, Pigazzi A, Marshall H, Croft J, Corrigan N, Copeland J, Quirke P, West N, Rautio T, Thomassen N, Tilney H, Gudgeon M, Bianchi PP, Edlin R, Hulme C, Brown J (2017) Effect of robotic-assisted vs conventional laparoscopic surgery on risk of conversion to open laparotomy among patients undergoing resection for rectal cancer: the ROLARR randomized clinical trial. JAMA 318:1569–1580
Singal AG, Higgins PD, Waljee AK (2014) A primer on effectiveness and efficacy trials. Clin Transl Gastroenterol 5:e45
Morris EJ, Jordan C, Thomas JD, Cooper M, Brown JM, Thorpe H, Cameron D, Forman D, Jayne D, Quirke P, Trialists C (2011) Comparison of treatment and outcome information between a clinical trial and the National Cancer Data Repository. Br J Surg 98:299–307
Funding
GCL was supported by the National Institutes of Health T32 Research Training in Alimentary Tract Surgery Grant DK007754-13.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Disclosures
Grace C. Lee was supported by the NIH T32 Research Training in Alimentary Tract Surgery grant DK007754-13. Liliana G. Bordeianou is a consultant for Ethicon and legal consultant for CRICO, receives royalty fees from Up-to-Date, and receives research support from 11 Health, all outside the submitted work. Todd D. Francone is a consultant for Intuitive, outside the submitted work. Lawrence S. Blaszkowsky, Robert N. Goldstone, Rocco Ricciardi, and Hiroko Kunitake have no conflicts of interest or financial ties to disclose. Motaz Qadan is a consultant for Olympus, outside the submitted work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Hiroko Kunitake and Motaz Qadan are co-senior authors.
Appendix 1: Definitions of commission on cancer facility types and facility regions
Appendix 1: Definitions of commission on cancer facility types and facility regions
Definitions of Commission on Cancer facility types | |
Community Cancer Program | Facility accessions 100–500 newly diagnosed cancer cases each year. Training resident physicians is optional |
Comprehensive Community Cancer Program | Facility accessions > 500 newly diagnosed cancer cases each year. Training resident physicians is optional |
Academic/Research Program | Facility accessions > 500 newly diagnosed cancer cases each year. Facility participates in training resident physicians in at least four program areas, including internal medicine and general surgery |
Integrated Network Cancer Program | Multiple facilities providing integrated cancer care. At least one facility is a hospital. Training resident physicians is optional, and there is no minimum caseload requirement |
States contained in each United States facility region | |
New England | CT, MA, ME, NH, RI, VT |
Middle Atlantic | NJ, NY, PA |
South Atlantic | DC, DE, FL, GA, MD, NC, SC, VA, WV |
East North Central | IL, IN, MI, OH, WI |
East South Central | AL, KY, MS, TN |
West North Central | IA, KS, MN, MO, ND, NE, SD |
West South Central | AR, LA, OK, TX |
Mountain | AZ, CO, ID, MT, NM, NV, UT, WY |
Pacific | AK, CA, HI, OR, WA |
Rights and permissions
About this article
Cite this article
Lee, G.C., Bordeianou, L.G., Francone, T.D. et al. Superior pathologic and clinical outcomes after minimally invasive rectal cancer resection, compared to open resection. Surg Endosc 34, 3435–3448 (2020). https://doi.org/10.1007/s00464-019-07120-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07120-2