Abstract
Aims
To examine the strength of evidence available for multiple facet joint injections (FJIs) and medial branch blocks (MBBs), and to report on the variations in the NHS England framework using the getting it right first time (GIRFT) data.
Methods
Systematic review using patient, intervention, comparison, outcome and study strategy. The literature search using Cochrane, MEDLINE and EMBASE databases using MeSH terms: lumbar spine, spinal injection and facet joint (“Appendix A”).
Results
Three studies were identified that investigated the efficacy of multiple FJIs or MBBs. None of these studies reported sustained positive outcomes at long-term follow-up.
Conclusion
There is a paucity of levels I and II evidence available for the efficacy of multiple FJIs and MBBs in treating low back pain. GIRFT data show a high degree of variation in the use of multiple FJIs, which would not be supported by the literature.
Graphic abstract
These slides can be retrieved under Electronic Supplementary Material.



Similar content being viewed by others
References
National Institute for Health and Care Excellence. Low back pain: the acute management of patients with chronic (longer than 6 weeks) non-specific low back pain. https://www.nice.org.uk/guidance/cg88/documents/low-back-pain-final-scope2
Health & Safety Executive (2017) Work-related Musculoskeletal Disorders (WRMSDs) Statistics in Great Britain. https://www.hse.gov.uk/statistics/overall/hssh1617.pdf
Rao M, Smuck M (eds) (2012) Orthopaedic knowledge update: spine 4. American Academy of Orthopaedic Surgeons, Rosemont
Koes BW, van Tulder MW, Thomas S (2006) Diagnosis and treatment of low back pain. BMJ 332(7555):1430–1434
Bogduk N (2004) Management of chronic low back pain. Med J Aust 180(2):79–83
British Orthopaedics Association (2017) Getting It right first time [cited 2017 26th November]. https://www.boa.ac.uk/pro-practice/getting-it-right-first-time/
National Institute for Health and Care Excellence (2016) Low back pain and sciatica in over 16 s: assessment and management. Invasive treatments. NICE guideline NG59. Methods, evidence and recommendations. https://www.nice.org.uk/guidance/ng59/evidence/full-guideline-invasive-treatments-pdf-2726157998
Manchikanti L, Falco FJ, Benyamin RM, Kaye AD, Boswell MV, Hirsch JA (2014) A modified approach to grading of evidence. Pain Physician 17(3):E319–E325
Manchikanti L, Pampati V, Bakhit CE, Rivera JJ, Beyer CD, Damron KS et al (2001) Effectiveness of lumbar facet joint nerve blocks in chronic low back pain: a randomized clinical trial. Pain Physician 4(1):101–117
Manchikanti L, Singh V, Falco FJE, Cash KA, Pampati V (2010) Evaluation of lumbar facet joint nerve blocks in managing chronic low back pain: a randomized, double-blind, controlled trial with a 2-year follow-up. Int J Med Sci 7(3):124–135
Fuchs S, Erbe T, Fischer HL, Tibesku CO (2005) Intraarticular hyaluronic acid versus glucocorticoid injections for nonradicular pain in the lumbar spine. J Vasc Interv Radiol 16(11):1493–1498
Bani A, Spetzger U, Gilsbach JM (2002) Indications for and benefits of lumbar facet joint block: analysis of 230 consecutive patients. Neurosurg Focus 13(2):E11
Beyer F, Geier F, Bredow J, Oppermann J, Schmidt A, Eysel P et al (2016) Non-operative treatment of lumbar spinal stenosis. Technol Health Care 24(4):551–557
Carrera GF (1980) Lumbar facet joint injection in low back pain and sciatica: preliminary results. Radiology 137(3):665–667
Destouet JM, Gilula LA, Murphy WA, Monsees B (1982) Lumbar facet joint injection: indication, technique, clinical correlation, and preliminary results. Radiology 145(2):321–325
Freyhardt P, Hartwig T, De Bucourt M, Maurer M, Renz D, Gebauer B et al (2013) MR-guided facet joint injection therapy using an open 1.0-T MRI system: an outcome study. Eur Radiol 23(12):3296–3303
Lewinnek GE, Warfield CA (1986) Facet joint degeneration as a cause of low back pain. Clin Orthop Relat Res 213:216–222
Lippitt AB (1984) The facet joint and its role in spine pain. Management with facet joint injections. Spine (Phila Pa 1976) 9(7):746–750
Lynch MC, Taylor JF (1986) Facet joint injection for low back pain. A clinical study. J Bone Joint Surg Br 68(1):138–141
Mooney V, Robertson J (1976) The facet syndrome. Clin Orthop Relat Res 115:149–156
Murtagh FR (1988) Computed tomography and fluoroscopy guided anesthesia and steroid injection in facet syndrome. Spine 13(6):686–689
Schulte TL, Pietila TA, Heidenreich J, Brock M, Stendel R (2006) Injection therapy of lumbar facet syndrome: a prospective study. Acta Neurochir (Wien) 148(11):1165–1172 (discussion 72)
Shih C, Lin GY, Yueh KC, Lin JJ (2005) Lumbar zygapophyseal joint injections in patients with chronic lower back pain. J Chin Med Assoc 68(2):59–64
Shim E, Lee JW, Lee E, Im T, Kang Y, Ahn JM et al (2017) Facet joint injection versus epidural steroid injection for lumbar spinal stenosis: intra-individual study. Clin Radiol 72(1):96.e7–96.e14
Han SH, Park KD, Cho KR, Park Y (2017) Ultrasound versus fluoroscopy-guided medial branch block for the treatment of lower lumbar facet joint pain: a retrospective comparative study. Medicine (Baltimore) 96(16):e6655
Bogduk N (2005) A narrative review of intra-articular corticosteroid injections for low back pain. Pain Med 6(4):287–296
Carrera GF, Williams AL (1984) Current concepts in evaluation of the lumbar facet joints. Crit Rev Diagn Imaging 21(2):85–104
Raymond J, Dumas JM (1984) Intraarticular facet block: diagnostic test or therapeutic procedure? Radiology 151(2):333–336
Raymond J, Dumas JM, Lisbona R (1984) Nuclear imaging as a screening test for patients referred for intraarticular facet block. J Can Assoc Radiol 35(3):291–292
Lau LS, Littlejohn GO, Miller MH (1985) Clinical evaluation of intra-articular injections for lumbar facet joint pain. Med J Aust 143(12–13):563–565
Moran R, O’Connell D, Walsh MG (1988) The diagnostic value of facet joint injections. Spine (Phila Pa 1976) 13(12):1407–1410
Tp N (1990) Facet joints: intra-articular steroids or nerve block? Pain Clin 3:77–82
Taylor MBER, Bubela CB (1987) Intra-articular facet block in chronic low back pain: results of patient selection based on clinical evaluation. Pain Clin 1:157–162
Lilius G, Laasonen EM, Myllynen P, Harilainen A, Salo L (1989) Lumbar facet joint syndrome. Significance of non-organic signs. A randomized placebo-controlled clinical study. Rev Chir Orthop Reparatrice Appar Mot 75(7):493–500
Lilius G, Laasonen E, Myllynen P, Harilainen A, Gronlund G (1989) Lumbar facet joint syndrome. A randomised clinical trial. J Bone Joint Surg Br 71-B(4):681–684
Carette S, Marcoux S, Truchon R, Grondin C, Gagnon J, Allard Y et al (1991) A controlled trial of corticosteroid injections into facet joints for chronic low back pain. New Engl J Med 325(14):1002–1007
Marks RC, Houston T, Thulbourne T (1992) Facet joint injection and facet nerve block: a randomised comparison in 86 patients with chronic low back pain. Pain 49(3):325–328
Mironer YESJ (1999) Protocol for diagnosis and treatment of facet joint syndrome. Pain Digest 9:188–190
Goupille PFV, Cotty P et al (1993) Arthro-infiltrations des articulaires postérieres lombaries dans les lombalgies chroniques. Resultats chez 206 patients. Rev Thum. 60:797–801
Vadeboncoeur R, Milette PC, Nistor MM (1986) Diagnostic and therapeutic value of infiltrations under fluoroscopic control, in the vertebral facet syndrome. Union Med Can 115(7):458–462
Schleifer JFG, Wolf A, Diehl K (1994) Behandlung des lumbalen Facettensyndroms durch CT-gesteuerte Infiltration der Zwischenwirbelgelenke. Radiologie 34:666–670
Sellier N, Vallee C, Chevrot A, Frantz N, Revel M, Wybier M et al (1986) Posterior lumbar vertebral arthrography. Pathologic aspects. J Radiol 67(6–7):497–506
Theron J, Blais M, Casasco A, Courtheoux P, Adam Y, Derlon JM et al (1983) Therapeutic radiology of the lumbar spine Disk chemonucleolysis, infiltration and coagulation of posterior articulations. J Neuroradiol 10(3):209–230
Ribeiro LH, Furtado RNV, Konai MS, Andreo AB, Rosenfeld A, Natour J (2013) Effect of facet joint injection versus systemic steroids in low back pain: a randomized controlled trial. Spine 38(23):1995–2002
Kawu A, Olawepo A, Salami A (2011) Facet joints infiltration: a viable alternative treatment to physiotherapy in patients with low back pain due to facet joint arthropathy. Niger J Clin Pract 14(2):219–222
Mayer TG, Gatchel RJ, Keeley J, McGeary D, Dersh J, Anagnostis C (2004) A randomized clinical trial of treatment for lumbar segmental rigidity. Spine 29(20):2199–2205
Ackerman WE 3rd, Ahmad M (2008) Pain relief with intraarticular or medial branch nerve blocks in patients with positive lumbar facet joint SPECT imaging: a 12-week outcome study. South Med J 101(9):931–934
Schütz U, Cakir B, Dreinhöfer K, Richter M, Koepp H (2011) Diagnostic value of lumbar facet joint injection: a prospective triple cross-over study. PLoS ONE 6(11):e27991
Annaswamy TM, Armstead C, Carlson L, Elkins NJ, Kocak D, Bierner SM (2017) Intraarticular triamcinolone versus hyaluronate injections for low back pain with symptoms suggestive of lumbar zygapophyseal joint arthropathy: a pragmatic, double blind randomized controlled trial. Am J Phys Med Rehabil 97(4):278–284
Yun DH, Kim HS, Yoo SD, Kim DH, Chon JM, Choi SH et al (2012) Efficacy of ultrasonography-guided injections in patients with facet syndrome of the low lumbar spine. Ann Rehabil Med 36(1):66–71
Al-Tawil K, Lopez D, Blackman M, Suresh S (2018) Oblique “Scotty dog” versus antero-posterior (AP) views in performing x-ray guided facet joint injections. J Clin Orthop Trauma 9(Suppl 1):S145–S148
Sae-Jung S, Jirarattanaphochai K (2016) Outcomes of lumbar facet syndrome treated with oral diclofenac or methylprednisolone facet injection: a randomized trial. Int Orthop 40(6):1091–1098
Celik B, Er U, Simsek S, Altug T, Bavbek M (2011) Effectiveness of lumbar zygapophysial joint blockage for low back pain. Turk Neurosurg 21(4):467–470
Kaplan M, Dreyfuss P, Halbrook B, Bogduk N (1998) The ability of lumbar medial branch blocks to anesthetize the zygapophysial joint: a physiologic challenge. Spine 23(17):1847–1852
Kennedy DJ, Huynh L, Wong J, Mattie R, Levin J, Smuck M et al (2018) Corticosteroid injections into lumbar facet joints: a prospective, randomized, double-blind placebo-controlled trial. Am J Phys Med Rehabil 97(10):741–746
McCall IW, Park WM, O’Brien JP (1979) Induced pain referral from posterior lumbar elements in normal subjects. Spine (Phila Pa 1976) 4(5):441–446
Ackerman WE, Munir MA, Zhang JM, Ghaleb A (2004) Are diagnostic lumbar facet injections influenced by pain of muscular origin? Pain Pract 4(4):286–291
Blackmore CC, Mecklenburg RS, Kaplan GS (2011) At Virginia Mason, collaboration among providers, employers, and health plans to transform care cut costs and improved quality. Health Aff (Millwood) 30(9):1680–1687
National Institute for Health and Care Excellence. Low back pain and sciatica in over 16s: assessment and management https://www.nice.org.uk/guidance/NG592016
Chou R, Loeser JD, Owens DK, Rosenquist RW, Atlas SJ, Baisden J et al (2009) Interventional therapies, surgery, and interdisciplinary rehabilitation for low back pain: an evidence-based clinical practice guideline from the American Pain Society. Spine (Phila Pa 1976) 34(10):1066–1077
Manchikanti L, Abdi S, Atluri S, Benyamin RM, Boswell MV, Buenaventura RM et al (2013) An update of comprehensive evidence-based guidelines for interventional techniques in chronic spinal pain. Part II: guidance and recommendations. Pain Physician 16(2):S49–S283
North RB, Kidd DH, Zahurak M, Piantadosi S (1996) Specificity of diagnostic nerve blocks: a prospective, randomized study of sciatica due to lumbosacral spine disease. Pain 65(1):77–85
Stojanovic MP, Dey D, Hord ED, Zhou Y, Cohen SP (2005) A prospective crossover comparison study of the single-needle and multiple-needle techniques for facet-joint medial branch block. Reg Anesth Pain Med 30(5):484–490
Hwang SY, Lee JW, Lee GY, Kang HS (2013) Lumbar facet joint injection: feasibility as an alternative method in high-risk patients. Eur Radiol 23(11):3153–3160
Gorbach C, Schmid MR, Elfering A, Hodler J, Boos N (2006) Therapeutic efficacy of facet joint blocks. AJR Am J Roentgenol 186(5):1228–1233
da Rocha ID, Cristante A, Marcon RM, Oliveira RP, Letaif OB, de Barros Filho TEP (2014) Controlled medial branch anesthetic block in the diagnosis of chronic lumbar facet joint pain: the value of a three-month follow-up. Clinics (Sao Paulo) 69(8):529–534
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendices
Appendix A
Manchikanti et al.’s [8] modified grading of qualitative evidence with best evidence synthesis for diagnostic accuracy and therapeutic interventions.
Level I | Evidence obtained from multiple relevant high quality randomised controlled trials |
Or | |
Evidence obtained from multiple high quality diagnostic accuracy studies | |
Level II | Evidence obtained from at least one relevant high quality randomised controlled trial or multiple relevant moderate or low quality randomised controlled trials |
Or | |
Evidence obtained from at least one high quality diagnostic accuracy study or multiple moderate or low quality diagnostic accuracy studies | |
Level III | Evidence obtained from at least one relevant moderate or low quality randomised controlled trial study |
Or | |
Evidence obtained from at least one relevant high quality non-randomised trial or observational study with multiple moderate or low quality observational studies | |
Or | |
Evidence obtained from at least one moderate quality diagnostic accuracy study in addition to low quality studies | |
Level IV | Evidence obtained from multiple moderate or low quality relevant observational studies |
Or | |
Evidence obtained from multiple relevant low quality diagnostic accuracy studies | |
Level V | Opinion or consensus of large group of clinicians and/or scientists |
Search strategy
-
1.
“Lumbar spine” [MeSH]
-
2.
“Spinal injection” [MeSH]
-
3.
1 AND 2
-
4.
“Facet joint” [MeSH] OR “zygapophyseal joint”
-
5.
4 AND “intervention”
-
6.
4 AND “spinal injection”
-
7.
3 AND “medial branch facet block”
-
8.
4 AND “medial branch facet block”
-
9.
3 AND “medial branch nerve block”
-
10.
4 AND “medial branch nerve block”.
Appendix B
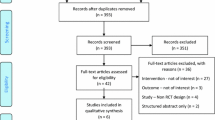
Preferred reporting items for systematic reviews (PRISMA) flow chart.

Appendix C
Levels I and II studies reporting multiple facet joint injections and medial branch blocks.
Author and references | Trial type | Interventions | Participants | Assessment tool | Outcome |
|---|---|---|---|---|---|
Medial branch blocks | |||||
Manchikanti [9] | RCT | I (lidocaine/bupivacaine LA + Sarapin) versus II (LA + Sarapin + methylprednisolone) | 73 (32 in I, 41 in II) | Verbal pain scale | Cumulative significant pain relief with 1–3 injections was 100% up to 1–3 months, 82% for 4–6 months, 21% for 7–12 months and 10% after 12 months, with a mean relief of ~ 6.6 months. Significant improvement also noted in overall health status and quality of life |
Mean number of procedures/interventions was ~ 8.4 in 13–32 months | No significant differences between both groups | ||||
Manchikanti [10] | Double-blind, RCT | IA (control group-lumbar facet joint nerve block using bupivacaine) versus IB (facet block using bupivacaine and Sarapin) versus IIA (facet block using bupivacaine + steroids) versus IIB (facet block using bupivacaine + steroids + Sarapin) | 120 (30 per group) | Numeric rating scale (NRS) + Oswestry Disability Index (ODI), opioid intake, and work status; at baseline, 3, 6, 12, 18 and 24 months | Significant pain relief and functional improvement seen in 85% in Group I and 90% of Group II at 2-year follow-up. Pain relief experienced for 82–84 of 104 weeks, requiring 5–6 injections (mean relief—19 weeks per injection) |
Facet joint injections | |||||
Fuchs [11] | Single-blind (observer) RCT | 10 mg sodium hyaluronate (SH) versus 10 mg triamcinolone acetonide (TA). Both into bilateral facet joints at levels S1–L5, L5–L4 and L4–L3. Done once a week for study duration | 60 (30 to SH, 30 to TA) | VAS, Rowland–Morris Questionnaire, ODI, low back outcomes score, short form-36 | Both showed long-lasting pain reduction, improved function and improved quality of life (at 6 months). SH-group showed better benefits, particularly in pain reduction |
Levels I and II studies reporting single facet joint injections and medial branch blocks.
Author and references | Trial type | Interventions | Participants | Assessment tool | Outcome |
|---|---|---|---|---|---|
Facet joint injections | |||||
Lilius [35] | RCT | I (6 mL [30 mg] bupivacaine hydrochloride + 2 mL [80 mg] methylprednisolone acetate] bilaterally into L3–L4 and L4–L5 versus II (same mixture as above into facet joint pericapsular space of same joint) versus III (8 mL saline into same joints as above) | 109 (28 to I, 39 to II, 42 to III) | VAS | Mean probability for p value differences in pain between groups (combined cortisone vs. saline) = 0.3375 |
(mean and SD) pain score on a scale of 0–100 mm for all 109 patients: | |||||
Before injection = 49.2 (22.3). 1 h = 30.9 (25.6). 2 weeks = 35.8 (25.9). 6 weeks = 40.7 (25.7). 3 months = 43.3 (26.6). p < 0.0001 | |||||
Mean probability for p value differences in disability between groups (combined cortisone vs. saline) = 0.1206 | |||||
(mean and SD) Disability score ranging from 6 to 18 constructed from 6 variables scoring from 1 to 3: (standing, walking, sitting, sitting with legs extended, climbing onto examination table and dressing) | |||||
Before injection = 10.3 (1.7). 1 h = 8.9 (2.3). 2 weeks = 9.1 (2.1). 6 weeks = 9.1 (1.9). p < 0.0001 | |||||
No significant between-group differences in pain intensity at each follow-up | |||||
Mean pain intensity differences from baseline across all groups were: − 18.7 at 1 h post-injection, − 13.4 at 2 week follow-up, − 8.5 at 6 weeks, and − 5.9 (all p ≤ 0.0001) | |||||
Carette [36] | Double-blind RCT | 20 mg methylprednisolone acetate (1 mL + 1 mL of isotonic saline) versus 2 mL isotonic saline Bilateral L4–L5 and L5–S1 facet injection | 97 (49 to steroid, 48 to saline) | Pain visual analogue scale (VAS) + McGill Pain Intensity Questionnaire + modified Sickness Impact Profile | Mean present pain intensity, intervention, baseline = 2.7 Mean present pain intensity, control, baseline = 2.8 Mean present pain intensity, intervention, 1 month = 2.3, control = 2.6 Mean present pain intensity, intervention, 6 months = 2.1, control = 2.9 Baseline mean VAS, intervention, 6.3, control, 6.2 1 month mean VAS intervention, 4.5, control 4.7 Difference (95% CI) = − 0.2 (− 1.1 to 0.8) 6 month mean VAS (0–10 cm scale) = 4.0 (methyl) = 5.0 (placebo) Difference (95% CI) = − 1.0 (− 2.0 to − 0.1) Mean sickness impact profile, intervention, baseline, 11.4, control 13.4 Mean sickness impact profile intervention, 1 month 9.3 control 9.8 Difference (95% CI) = − 0.5 (− 2.8 to 1.7) Mean sickness impact profile, intervention, 6 month, 7.8 control 10.8 Difference (95% CI) = − 3.0 (− 6.2 to 0.2) After 1 month, 42% of steroid group and 33% of saline group reported improvement in VAS and pain intensity which was marked or better from baseline pain levels (95% CI for difference, − 11 to 28; p = 0.53) Similar results at 3 months At 6 months, 22% of steroid group and 10% of saline group had sustained improvement from 1st to 6th month (95% CI for difference, − 2 to 26; p = 0.19) When concurrent interventions (physical therapy, antidepressant medication, peridural injections) taken into account, 31% of steroid group and 17% of saline group had sustained improvement at 6th month (95% CI for difference, − 3 to 31; p = 0.17) |
Marks [37] | Double-blind RCT | 0.5 mL Depomedrone (20 mg methylprednisolone acetate) + 1.5 mL lignocaine (1%) at L5–S1 versus 0.5 mL Depomedrone + 1.5 mL lignocaine facet nerve blocks of the L1–L5 medial articular branches of the posterior primary rami | 83 (41 to joint injection, 42 to nerve block) | Level of pain relief + ROM (range of motion) provocative test | At 2 weeks, 43% and 45% of patients reported good or excellent pain severity improvements in joint injection and nerve block groups, respectively |
At 1 month, this was 36% and 20.5% | |||||
At 3 months, this was 22% and 14% | |||||
All reported changes were statistically significant (p < 0.05) | |||||
Ribeiro [44] | Double-blind RCT | Bilateral facet joint injections of 1 mL (20 mg) triamcinolone hexacetonide into L3–L4, L4–L5 and L5–S1 joints (6 injections, 120 mg total) + 1 mL lidocaine [EG] versus bilateral intramuscular injections of 1 mL (20 mg) of triamcinolone acetonide + 1 mL lidocaine on 6 surface points of lumbar paravertebral musculature (120 mg total) [CG] | 60 (31 to EG, 29 to CG) | Pain VAS + pain VAS during extension of the spine + Likert scale + improvement percentage scale + Roland-Morris + 36-Item Short Form Health Survey + accountability of medications taken | At 1 week, 90% of EG and 86% of CG reported “better” or “much better” pain improvements in a Likert scale. The difference between groups was statistically significant (p = 0.029) |
No statistically significant differences in pain improvement and disability between groups at 4, 12 and 24 weeks | |||||
Kawu [45] | RCT | Intraarticular 0.5 mL of 0.25% bupivacaine + 0.5 mL (20 mg) of methylprednisolone acetate versus Physiotherapy (McKenzie regimen) | 18 (10 to injection, 8 to physiotherapy) | VAS, ODI | At 6 months, mean visual analogue scale scores lower in injection group (4), compared with physio group (5) [p = 0.032] |
FJI group fared consistently better with a low mean ODI score against the mean score of the physiotherapy group. No direct information specifically reported for the ODI except graph showing ODI against time | |||||
Mayer [46] | Single-blind RCT | A [(Multi-level (3) bilateral facet injections of 1 mL 2% lidocaine + 1 mL 0.5% bupivacaine + 1 mL steroid) + home stretching exercise programme versus B [exercise programme only—twice a week in facility and concurrent home stretching programme] | 70 (36 to A, 34 to B) | VAS | At 5–7 week follow-up, mean pain intensity decreased in A (mean change 0.9, p ≤ 0.003) and in B (mean change 0.8, p ≤ 0.004) |
No difference between groups at follow-up (p = 0.27) | |||||
Ackerman [47] | Double-blind RCT | Lumbar FJ SPECT-positive I (Intraarticular) versus II (Medial branch nerve blocks) of triamcinolone and lidocaine | 46 (23 to each) | Numeric Pain Intensity (NPS) score, ODI | Pain relief and improved disability were observed in 61% and 53% of patients in group I, and in 26% and 31% of group II. This difference was statistically significant (p < 0.05) |
Schütz [48] | Single-blind, triple crossover RCT | 3 bilateral facet joint injections: verum (1.5 mL 1% Mepivacaine), placebo (1.5 mL 0.9% isotonic sodium chloride solution), sham (extraarticular positioning of needle without volume application) | 60 (10 to each) | VAS | Study was into diagnostic value of facet joint injections. It concluded that there were no significant differences between the three different injection types and that a single intraarticular block with local anaesthetic was not useful in diagnosing facet joint pain |
Participants randomised to 6 parallel groups based on sequence of injections received | |||||
Annaswamy [49] | Double-blind RCT | Bilateral L3–S1 FJIs | VAS and Pain disability questionnaire (PDQ) | ||
Triamcinolone versus Synvisc-One | |||||
Yun [50] | RCT | Intraarticular FJI of 10 mg triamcinolone + 2 mL of 1% lidocaine; bilateral or unilateral; into L4–L5 and/or L5–S1 | 57 (32 to FL, 25 to US) | VAS, physician’s and patient’s global assessment (PhyGA, PaGA), modified Oswestry Disability Index (ODI) | Significant decrease in VAS at 1 week (mean change − 3.31), 1 month (mean difference − 3.40) and at 3 months (mean difference − 2.87) [p = < 0.001 for all changes] |
Fluoroscopy-guided (FL) versus ultrasound-guided (US) | Similarly, significant decreases at each follow-up in PaGA, PhyGA and modified ODI | ||||
No significant differences between groups at each follow-up | |||||
Al-Tawil [51] | Single-blind RCT | Intraarticular FJI using oblique versus antero-posterior (AP) x-ray guidance | 29 (17 to AP, 12 to oblique) | Numerical 11 point pain rating scale questionnaire | Statistically significant difference in pain scores between pre- and post-op in both groups |
No significant differences between groups | |||||
Sae-Jung [52] | RCT | 100 mg/day oral diclofenac for? how long (D) versus 80 mg intraarticular methylprednisolone into each symptomatic facet joint (IA) versus both (B) | 99 (33 to D, 32 to IA, 34 to B) | VAS and ODI | Initial ODI (mean ± SD) was 45.1 ± 9.3, 42.9 ± 15.6, 42.2 ± 11.5 for D, IA and B groups, respectively. Respective 4-week ODI was 30.1 ± 8.1, 20.2 ± 8.0 and 15.1 ± 5.5. The 12-week ODI was 42.4 ± 9.0, 32.2 ± 15.6 and 26.2 ± 11.7 |
Initial VAS was 7.1 ± 1.2, 7.6 ± 1.1 and 7.3 ± 1.0. The 4 week VAS was 5.3 ± 1.4, 3.6 ± 0.7 and 3.3 ± 1.1. The 12-week VAS was 6.1 ± 1.1, 5.8 ± 1.4 and 5.1 ± 0.9 | |||||
Combined treatment was more effective than either treatment alone. IA also had better ODI scores than D | |||||
Celik [53] | RCT | Bilateral L4/5 and L5/S1 facet joints block with prilocaine (skin preparation) 10 mg bupivacaine and 5 mg methylprednisolone versus diclofenac sodium 100 mg/day thiocolchicoside 8 mg/day for 5 days and recommended bed rest for 4 days | 80 (40 to each) | ODI, VAS | Intervention group: |
VAS pre-treatment = 8. Immediately after = 2. 1st month = 1. 3rd month = 5. 6th month = 2 | |||||
Control group: | |||||
VAS pre-treatment = 7. Immediately after = 3. 1st month = 2. 3rd month = 4. 6th month = 5 | |||||
Decrease in VAS scores in post-treatment at 1st, 3rd and 6th month was not statistically significant (p > 0.005) | |||||
Intervention group: | |||||
ODI pre-treatment = 23. Immediately after = 5. 1st month = 5. 3rd month = 11. 6 months = 3 | |||||
Control group: ODI pre-treatment = 21. Immediately after = 9. 1st month = 4. 3rd month = 7. 6th month = 11 Reduction in ODQ scores in intervention group was greater than in control group (p < 0.005) | |||||
Between-group differences were not reported | |||||
Kennedy [55] | Double-blind, RCT | Triamcinolone 20 mg versus saline | 28 (14 to each group) | ODI, Numeric Pain Rating (NPR) scale | No statistical difference in the subsequent need for radiofrequency neurotomy |
North [62] | RCT | 3 mL of 0.5% bupivacaine | 33 | Standardised 0–10 rating pain scale | False positive results were common |
3 different nerve blocks [paraspinal lumbosacral root block, medial branch posterior ramus block (at or proximal to the pathology and sciatic nerve blocks (distal or collateral to the pathology)] versus control lumbar subcutaneous injection of identical volume | For sciatic nerve block specificity was 24%–36% | ||||
For root blocks sensitivity was 9%–42% | |||||
All the different nerve blocks produced temporary pain relief in majority of patients | |||||
Statistical analysis of clinical and technical prognostic factors revealed that the only association with pain relief by any block was the effects of other blocks. The strongest association was between relief by sciatic nerve block and relief by medial branch posterior primary ramus (facet) block (P = 0.001, odds ratio 16.0). | |||||
Medial branch blocks | |||||
Kaplan [54] | Single-blind RCT | Two saline injections versus two 2% lidocaine medial branch injection | 14 (9 to medial branch block, 5 to control) | Repeat capsular distension (30 min after) in order to elicit pain | All 5 control individuals who received saline medial branch injections felt pain on repeat capsular distention |
Of the 9 individuals who received 2% lidocaine medial branch blocks, 8 felt no pain and 1 felt pain on repeat capsular distention | |||||
Stojanovic [63] | Crossover-comparison RCT | 2 separate diagnostic medial branch blocks (single-needle versus multiple-needle technique) | 24 | VAS | Single-needle technique resulted in less procedure-related pain (p = .0003), required less superficial local anaesthesia (p = .0006) and took less time to complete (p < .0001) than the multiple-needle approach |
Multiple variables compared | Single-needle technique also provided same degree of accuracy | ||||
Levels III–V studies reporting single and multiple FJIs.
Author and year | Trial type | Interventions | Participants | Assessment tool | Outcome |
|---|---|---|---|---|---|
Bani [12] | Prospective case series | Intraarticular FJI with LA and/or steroid | 715 FJIs in 230 patients | Pain relief | 18.7% of patients reported lasting pain relief at 10 months |
1st injection: 1 mL bupivacaine 1% | 15.2% noticed general pain improvement | ||||
2nd injection (if 1st successful): betamethasone | 11.7% reported relief of low back pain but not leg pain | ||||
3.9% suffered no back pain but still leg pain | |||||
50.4% experienced no improvement in pain at all | |||||
In two cases, the procedure had to be interrupted because of severe pain | |||||
Beyer [13] | Prospective study | Repeated epidural injections and FJIs and also physiotherapy during 1-week hospitalisation | 38 | VAS, ODI, Core Outcome Measures Index (COMI), Short-Form 36 Health Survey Questionnaire(SF-36) | Significant improvements in back and leg pain VAS up to 3 months |
Carrera [14] | Prospective case series | Fluoroscopically-guided intraarticular FJ blocks of local anaesthetic and steroid | 20 | Pain relief | 13/20 patients had immediate pain relief, confirming diagnosis |
6/20 patients pain free for 6 months following single block | |||||
Destouet [15] | Prospective case series | 1 mL 0.25% bupivacaine and 40 mg depot methylprednisolone | 54 | Pain relief | 54% of patients had initial relief (up to 3 months). 38% had continued pain relief for 3 months or longer |
11% of patients were pain free for 6–12 months | |||||
Freyhardt [16] | Prospective case series | MR fluoroscopic-guided FJ block of local anaesthetic and steroid | 166 facet joints in 45 patients | VAS | 38 patients completed study |
63% had pain relief immediately | |||||
34% had lasting pain relief at 6 months | |||||
24% had lasting pain relief at 12 months | |||||
Mean VAS was reduced from 7.1 ± 1.7 (baseline) to 3.5 ± 2.2, 4.1 ± 3.0, 3.8 ± 2.9 and 4.6 ± 2.9 at 1 week, 3, 6 and 12 months (p < 0.01) | |||||
Lewinnek [17] | Prospective case series | Intraarticular FJI with local anaesthetic and steroid | 21 | Pain relief | 75% of patients had initial positive response |
33% still had positive response at 3 months | |||||
Repeat injections, when done, always led to temporary relief, but only to lasting relief in 20% (1 in 5) of those who had repeat injections | |||||
Lippitt [18] | Retrospective review | Intraarticular injection of 1 mL 1% lidocaine and 80 mg depot methylprednisolone | 99 | Pain relief | 42% of patients had initial relief, which declined to 14% at 6 months |
Lynch and Taylor [19] | Case series | Bilateral intraarticular 0.5% lignocaine + 60 mg methylprednisolone mixed | 50 | Level of pain relief | Intraarticular injection into two joints more effective than one. Both effective but improvements reduce with time. Intraarticular FJI more effective than “failed” extraarticular FJI |
Murtagh [21] | Prospective case series | Repeat intraarticular injections of lidocaine and 6 mg betamethasone | 100 | Pain relief | 54% of patients had more than 3 months of pain relief |
Schulte [22] | Case series | Up to 6 intraarticular FJIs of prednisolone acetate, lidocaine 1% and phenol 5% | 39 | Pain Disability Index, MacNab criteria, VAS | “Excellent” or “good” response seen in 62% of patients after 1 month, 41% after 3 months and 36% after 6 months |
Positive effect on pain in short term. Effects reduce within 3 months | |||||
Shih [23] | Case series | 1–3 Intraarticular injections of 0.3–1.5 mL lignocaine with betamethasone dipropionate (Diprosan) + iopamidol (1:1:0.5) | 277 | VAS | 73.6% had pain relief for at least 1 week. Effects reduced with time |
Bilateral in 42.2% of patients | |||||
Shim [24] | Retrospective case series | Patients receiving multiple injections for lumbar canal stenosis | 73 | Five-point satisfaction scale | 50/73 patients had 3rd injection |
Review of which injection (FJI or epidural steroid injection [ESI]) was used as 3rd injection after sequential injections of FJI and ESI | 33 underwent FJI as the 3rd injection | ||||
Out of 19/73 patients who experienced ineffective first ESI, 13 (68.4%) reported 2nd FJI as effective | |||||
Out of the 6/13 patients who reported the 2nd FJI as ineffective, 3/6 (50%) reported the 2nd ESI as effective | |||||
Authors conclude that FJIs can be administered as an alternative to ESIs in cases of lumbar canal stenosis | |||||
Han [25] | Retrospective study | Ultrasound versus fluoroscopy-guided MBB | 146 (68 to USS, 78 to FL) | VAS, ODI, VNS (verbal numeric scale) | ODI and VNS scores improved at 1, 3 and 6 months after last injections in both groups. No significant differences between both groups |
Lau [30] | Retrospective case series | Bilateral intraarticular 1.5 mL bupivacaine hydrochloride (0.5% Marcain) and 20 mg methylprednisolone acetate (Depo-Medrol) | 34 | Pain relief percentage scale | 63% reported relief of greater than 70% for 6 months or longer |
Moran [31] | Prospective case series | Intraarticular 1.5 mL bupivacaine | 143 facet joints in 54 patients | Pain provocation and pain relief | Diagnosis was confirmed in only 16.7% (nine) of patients |
Mooney and Robertson [37] | Case series | 3 Intraarticular FJIs of 1 mL of Depo-Medrol and 2–5 mL local anaesthetic | 100 | Questionnaire | Intraarticular steroid + LA mixture effective but effects reduce by 6 months |
Hwang [64] | Retrospective case series | Single-level bilateral FJI with steroid | 42 | Five-point patient satisfaction scale | 59.5% of patients considered the treatment to have been effective |
72% of the 25 patients with mild-to-moderate central canal stenosis had symptom relief | |||||
7 of the 17 (41.2%) patients with severe central canal stenosis had symptom relief (p < 0.05) | |||||
Other outcome predictors were not statistically significant | |||||
Gorbach [65] | Prospective case series | Single-level or two-level FJ block with 0.5 mL of local anaesthetic and 0.5 mL of steroid | 42 | VAS | Positive immediate effect was seen in 31 patients (74%) |
Positive medium-term effect was found in 14 patients (33%) | |||||
Pain alleviated by motion (p = 0.035) and the absence of joint-blocking sensation (p = 0.042) predicted pain relief | |||||
Extent of facet joint osteoarthritis on MRI and CT was not a significant predictor for outcome (p = 0.57–0.95) | |||||
da Rocha [66] | Prospective case series | Sham blockade (with saline injection) and then controlled medial branch block with 0.5 mL lidocaine 2% | 104 | VAS | 52% of patients demonstrated > 50% improvements in pain after the blockade |
False positive results seen in 67% of patients |
Rights and permissions
About this article
Cite this article
Onafowokan, O.O., Fine, N.F., Brooks, F. et al. Multiple injections for low back pain: What’s the future?. Eur Spine J 29, 564–578 (2020). https://doi.org/10.1007/s00586-019-06258-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-019-06258-w