Abstract
Purpose
A variety of alternative grafts to autologous iliac crest bone (ICBG) have been developed for lumbar spondylodesis, due to frequent complications following ICBG harvest. The optimal alternative graft to ICBG, however, remains elusive till now. The purpose of this study was to compare the efficacy and safety of fusion materials in lumbar degeneration diseases and to provide a ranking spectrum of the grafts.
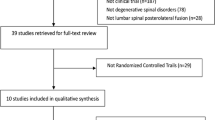
Methods
Randomized controlled trials (RCTs) comparing different bone grafts in lumbar arthrodesis were eligible for inclusion. A network meta-analysis was performed for endpoints including fusion rate and incidence of adverse events.
Results
Twenty-seven RCTs involving 2488 patients and 13 available interventions were included. rhBMP-2 provided the highest fusion rate, being significantly superior to that of ICBG (OR = 0.21, p < 0.001), autograft local bone (ALB) (OR = 0.18, p = 0.022), rhBMP-7 (OR = 0.15, p < 0.001), allograft (OR = 0.13, p = 0.009), and DBM + ALB (OR = 0.07, p = 0.048). The treatment efficacy of allograft could be significantly enhanced by bone marrow concentrate (BMC) supplying (OR = 0.16, p = 0.010). ICBG ranks second on the frequency of complications, which is significantly higher than that of allograft (OR = 0.14, p = 0.041) and ALB (OR = 0.14, p = 0.030). All of the other comparisons showed similar efficacy and safety profiles between groups.
Conclusion
Ranking spectrums of the efficacy and safety for various bone grafts were provided graphically. Though rhBMP-2 was of the highest success rate, the application should be taken with proper caution because of the widely proposed life-threatening adverse events. ALB, ALB plus synthetic ceramic materials and allograft mixed with BMC were also proved to be potentially effective alternative graft to ICBG.
Graphic abstract
These slides can be retrieved under Electronic Supplementary Material.







Similar content being viewed by others
References
Fritzell P, Hägg O, Jonsson D et al (2004) Cost-effectiveness of lumbar fusion and nonsurgical treatment for chronic low back pain in the Swedish Lumbar Spine Study: a multicenter, randomized, controlled trial from the Swedish Lumbar Spine Study Group. Spine (Phila Pa 1976) 29:421–434.
Liu X, Wang Y, Qiu G et al (2014) A systematic review with meta-analysis of posterior interbody fusion versus posterolateral fusion in lumbar spondylolisthesis. Eur Spine J 23:43–56
Pimenta L, Marchi L, Oliveira L et al (2013) A prospective, randomized, controlled trial comparing radiographic and clinical outcomes between stand-alone lateral interbody lumbar fusion with either silicate calcium phosphate or rh-BMP2. J Neurol Surg A Cent Eur Neurosurg 74:343–350
Hurlbert RJ, Alexander D, Bailey S et al (2013) rhBMP-2 for posterolateral instrumented lumbar fusion: a multicenter prospective randomized controlled trial. Spine (Phila Pa 1976) 38:2139–2148.
Shen F, Samartzis D, An H (2005) Cell technologies for spinal fusion. Spine 5:231S–S239
Marchesi DG (2000) Spinal fusions: bone and bone substitutes. Eur Spine J 9:372–378
Myeroff C, Archdeacon M (2011) Autogenous bone graft: donor sites and techniques. J Bone Joint Surg Am 93:2227–2236
Banwart JC, Asher MA, Hassanein RS (1995) Iliac crest bone graft harvest donor site morbidity a statistical evaluation. Spine (Phila Pa 1976) 20:1055–1060.
VonderHoeh NH, Voelker A, Heyde CE (2017) Results of lumbar spondylodeses using different bone grafting materials after transforaminal lumbar interbody fusion (TLIF). Eur Spine J 26:2835–2842
Boden SD, Zdeblick TA, Sandhu HS et al (2000) The use of rhBMP-2 in interbody fusion cages. Definitive evidence of osteoinduction in humans: a preliminary report. Spine (Phila Pa 1976) 25:376–381.
Johnson RG (2014) Bone marrow concentrate with allograft equivalent to autograft in lumbar fusions. Spine (Phila Pa 1976) 39:695–700.
Simmonds MC, Brown JV, Heirs MK et al (2013) Safety and effectiveness of recombinant human bone morphogenetic protein-2 for spinal fusion: a meta-analysis of individual-participant data. Ann Intern Med 158:877–889
Papakostidis C, Kontakis G, Bhandari M et al (2008) Efficacy of autologous iliac crest bone graft and bone morphogenetic proteins for posterolateral fusion of lumbar spine: a meta-analysis of the results. Spine (Phila Pa 1976) 33:E680–692.
Fu R, Selph S, McDonagh M et al (2013) Effectiveness and harms of recombinant human bone morphogenetic protein-2 in spine fusion: a systematic review and meta-analysis. Ann Intern Med 158:890–902
Ye F, Zeng Z, Wang J et al (2018) Comparison of the use of rhBMP-7 versus iliac crest autograft in single-level lumbar fusion: a meta-analysis of randomized controlled trials. J Bone Miner Metab 36:119–127
Parajón A, Alimi M, Navarro-Ramirez R et al (2017) Minimally Invasive Transforaminal Lumbar Interbody Fusion: Meta-analysis of the Fusion Rates. What is the Optimal Graft Material? Neurosurgery 81:958–971
Moher D, Liberati A, Tetzlaff J et al (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:b2535
Higgins JPT, Altman DG, Gøtzsche PC et al (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928
Higgins JPT, Green S (2011) Cochrane handbook for systematic reviews of interventions version 5.1.0. The Cochrane Collaboration, 2011. Available from www. cochrane-handbook.org.
Salanti G, Ades AE, Ioannidis JP (2011) Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol 64:163–171
Tan SH, Cooper NJ, Bujkiewicz S et al (2014) Novel presentational approaches were developed for reporting network meta-analysis. J Clin Epidemiol 67:672–680
Egger M, Davey Smith G, Schneider M et al (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634
Cho JH, Lee JH, Yeom JS et al (2017) Efficacy of Escherichia coli-derived recombinant human bone morphogenetic protein-2 in posterolateral lumbar fusion: an open, active-controlled, randomized, multicenter trial. Spine J 17:1866–1874
Delawi D, Jacobs W, van Susante JL et al (2016) OP-1 Compared with Iliac Crest Autograft in Instrumented Posterolateral Fusion: A Randomized, Multicenter Non-Inferiority Trial. J Bone Joint Surg Am 98:441–448
Kang J, An H, Hilibrand et al (2012) A Grafton and local bone have comparable outcomes to iliac crest bone in instrumented single-level lumbar fusions. Spine (Phila Pa 1976) 37:1083–1091.
Delawi D, Dhert WJ, Rillardon L et al (2010) A prospective, randomized, controlled, multicenter study of osteogenic protein-1 in instrumented posterolateral fusions: report on safety and feasibility. Spine (Phila Pa 1976) 35:1185–91.
Dawson E, Bae HW, Burkus JK et al (2009) Recombinant human bone morphogenetic protein-2 on an absorbable collagen sponge with an osteoconductive bulking agent in posterolateral arthrodesis with instrumentation. A prospective randomized trial. J Bone Joint Surg Am 91:1604–1613
Dimar JR 2nd, Glassman SD, Burkus JK et al (2009) Clinical and radiographic analysis of an optimized rhBMP-2 formulation as an autograft replacement in posterolateral lumbar spine arthrodesis. J Bone Joint Surg Am 91:1377–1386
Dai LY, Jiang LS (2008) Single-level instrumented posterolateral fusion of lumbar spine with beta-tricalcium phosphate versus autograft: a prospective, randomized study with 3-year follow-up. Spine (Phila Pa 1976) 33:1299–1304.
Glassman SD, Carreon LY, Djurasovic M et al (2008) RhBMP-2 versus iliac crest bone graft for lumbar spine fusion: a randomized, controlled trial in patients over sixty years of age. Spine (Phila Pa 1976) 33:2843–2849.
Dimar JR, Glassman SD, Burkus KJ et al (2006) Clinical outcomes and fusion success at 2 years of single-level instrumented posterolateral fusions with recombinant human bone morphogenetic protein-2/compression resistant matrix versus iliac crest bone graft. Spine (Phila Pa 1976) 31:2534–2539.
Kanayama M, Hashimoto T, Shigenobu K et al (2006) A prospective randomized study of posterolateral lumbar fusion using osteogenic protein-1 (OP-1) versus local autograft with ceramic bone substitute: emphasis of surgical exploration and histologic assessment. Spine (Phila Pa 1976) 31:1067–1074.
Korovessis P, Koureas G, Zacharatos S et al (2005) Correlative radiological, self-assessment and clinical analysis of evolution in instrumented dorsal and lateral fusion for degenerative lumbar spine disease. Autograft versus coralline hydroxyapatite. Eur Spine J 14:630–638
Glassman SD, Dimar JR, Carreon LY et al (2005) Initial fusion rates with recombinant human bone morphogenetic protein-2/compression resistant matrix and a hydroxyapatite and tricalcium phosphate/collagen carrier in posterolateral spinal fusion. Spine (Phila Pa 1976) 30:1694–1698.
Johnsson R, Strömqvist B, Aspenberg P (2002) Randomized radiostereometric study comparing osteogenic protein-1 (BMP-7) and autograft bone in human noninstrumented posterolateral lumbar fusion: 2002 Volvo Award in clinical studies. Spine (Phila Pa 1976) 27:2654–2661.
Vaccaro AR, Patel T, Fischgrund J et al (2004) A pilot study evaluating the safety and efficacy of OP-1 Putty (rhBMP-7) as a replacement for iliac crest autograft in posterolateral lumbar arthrodesis for degenerative spondylolisthesis. Spine (Phila Pa 1976) 29:1885–1892.
Vaccaro AR, Whang PG, Patel T et al (2008) The safety and efficacy of OP-1 (rhBMP-7) as a replacement for iliac crest autograft for posterolateral lumbar arthrodesis: minimum 4-year follow-up of a pilot study. Spine J 8:457–465
Coughlan M, Davies M, Mostert AK et al (2018) A Prospective, Randomized, Multicenter Study Comparing Silicated Calcium Phosphate versus BMP-2 Synthetic Bone Graft in Posterolateral Instrumented Lumbar Fusion for Degenerative Spinal Disorders. Spine (Phila Pa 1976) 43:E860-E868.
Hart R, Komzák M, Okál F et al (2014) Allograft alone versus allograft with bone marrow concentrate for the healing of the instrumented posterolateral lumbar fusion. Spine J 14:1318–1324
Ohtori S, Suzuki M, Koshi T et al (2011) Single-level instrumented posterolateral fusion of the lumbar spine with a local bone graft versus an iliac crest bone graft: a prospective, randomized study with a 2-year follow-up. Eur Spine J 20:635–639
Nandyala SV, Marquez-Lara A, Fineberg SJ et al (2014) Prospective, randomized, controlled trial of silicate-substituted calcium phosphate versus rhBMP-2 in a minimally invasive transforaminal lumbar interbody fusion. Spine (Phila Pa 1976) 39:185–191.
Huang H, Jiang C, Feng Z et al (2014) Comparing the process of creeping substitution between allograft bone and local bone grafting in lumbar interbody fusion. Eur Spine J 23:2068–2074
Sys J, Weyler J, Van Der Zijden T et al (2011) Platelet-rich plasma in mono-segmental posterior lumbar interbody fusion. Eur Spine J 20:1650–1657
Putzier M, Strube P, Funk JF et al (2009) Allogenic versus autologous cancellous bone in lumbar segmental spondylodesis: a randomized prospective study. Eur Spine J 18:687–695
Burkus JK, Sandhu HS, Gornet MF (2006) Influence of rhBMP-2 on the healing patterns associated with allograft interbody constructs in comparison with autograft. Spine (Phila Pa 1976) 31:775–781.
Haid RW Jr, Branch CL Jr, Alexander JT et al (2004) Posterior lumbar interbody fusion using recombinant human bone morphogenetic protein type 2 with cylindrical interbody cages. Spine J 4:527–538
Cha CW, Boden SD (2003) Gene therapy applications for spine fusion. Spine 28:S74–84
Agarwal R, Williams K, Umscheid CA et al (2009) Osteoinductive bone graft substitutes for lumbar fusion: a systematic review. J Neurosurg Spine 11:729–740
Carlisle E, Fischgrund JS (2005) Bone morphogenetic proteins for spinal fusion. Spine J 5:240S–249S
Chen Z, Ba G, Shen T et al (2012) Recombinant human bone morphogenetic protein-2 versus autogenous iliac crest bone graft for lumbar fusion: a meta-analysis of ten randomized controlled trials. Arch Orthop Trauma Surg 132:1725–1740
Cahill KS, Chi JH, Day A et al (2009) Prevalence, complications, and hospital charges associated with use of bone-morphogenetic proteins spinal fusion procedures. JAMA 302:58–66
Benglis D, Wang MY, Levi AD (2008) A comprehensive review of the safety profile of bone morphogenetic protein in spine surgery. Neurosurgery 62:ONS423–431.
Kanatani M, Sugimoto T, Kaji H et al (1995) Stimulatory effect of bone morphogenetic protein-2 on osteoclast-like cell formation and bone-resorbing activity. J Bone Miner Res 10:1681–1690
Carragee EJ, Hurwitz EL, Weiner BK (2011) A critical review of recombinant human bone morphogenetic protein-2 trials in spinal surgery: emerging safety concerns and lessons learned. Spine J 11:471–491
Rowan FE, O’Malley N, Poynton A (2012) RhBMP-2 use in lumbar fusion surgery is associated with transient immediate post-operative leg pain. Eur Spine J 21:1331–1337
Poorman GW, Jalai CM, Boniello A (2017) Bone morphogenetic protein in adult spinal deformity surgery: a meta-analysis. Eur Spine J 26:2094–2102
Wozney JM (2002) Overview of bone morphogenetic proteins. Spine (Phila Pa 1976) 27:S2–8
Eder C, Chavanne A, Meissner J et al (2011) Autografts for spinal fusion: osteogenic potential of laminectomy bone chips and bone shavings collected via high speed drill. Eur Spine J 20:1791–1795
Lee JH, Lee DH, Ryu HS et al (2003) Porous beta-calcium pyrophosphate as a bone graft substitute in a canine bone defect model. Key Eng Mater 240–2:399–402
Zimmermann G, Moghaddam A (2011) Allograft bone matrix versus sythetic bone graft substitutes. Injury 42:S16–21
Miyazaki M, Tsumura H, Wang JC et al (2009) An update on bone substitutes for spinal fusion. Eur Spine J 18:783–799
Kraiwattanapong C, Boden SD, Louis-Ugbo J et al (2005) Comparison of Healos/bone marrow to INFUSE(rhBMP-2/ACS) with a collagen-ceramic sponge bulking agent as graft substitutes for lumbar spine fusion. Spine 30:1001–1007
Tortolani PJ, Park AE, Louis-Ugbo J et al (2004) The effects of doxorubicin (adriamycin) on spinal fusion: An experimental model of posterolateral lumbar spinal arthrodesis. Spine J 4:669–674
Goodwin CB, Brighton CT, Guyer RD et al (1999) A double-blind study of capacitively coupled electrical stimulation as an adjunct to lumbar spinal fusions. Spine 24:1349–1356
Malloy KM, Hilibrand AS (2002) Autograft versus allograft in degenerative cervical disease. Clin Orthop Relat Res 394:27–38
Brodsky AE, Kovalsky ES, Khalil MA et al (1991) Correlation of radiologic assessment of lumbar spine fusions with surgical exploration. Spine 16:S261–S265
Dawson EG, Clader TJ, Bassett LW et al (1985) A comparison of different methods used to diagnose pseudarthrosis following posterior spinal fusion for scoliosis. J Bone Joint Surg Am 67:1153–1159
Acknowledgments
I would like to express special thanks to my partners for the encouragement and support they gave me during my study.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix
Appendix
See Table
2.
Rights and permissions
About this article
Cite this article
Feng, Jt., Yang, Xg., Wang, F. et al. Efficacy and safety of bone substitutes in lumbar spinal fusion: a systematic review and network meta-analysis of randomized controlled trials. Eur Spine J 29, 1261–1276 (2020). https://doi.org/10.1007/s00586-019-06257-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-019-06257-x