Abstract
Background
Cardiovascular diseases (CVDs) are responsible for 31% of all deaths worldwide. Genetic predisposition to CVDs in adolescents remains largely unknown. The aim of this study was to examine the association of UCP1, UCP2 and UCP3 gene polymorphisms with CVD risk factors in European adolescents.
Method
A cross-sectional study that involves 1.057 European adolescents (12–18 years old) from the HELENA study. A total of 18 polymorphisms of UCP1, UCP2 and UCP3 genes were genotyped. We measured serum total cholesterol, high-density lipoprotein,low-density lipoprotein, ApoA1, ApoB, leptin, triglycerides, glucose, insulin and blood pressure, and calculated HOMA (homeostatic model assessment), Quantitative Insulin Sensitivity Check Index (QUICKI) and a CVD risk score.
Results
The G allele of UCP2 rs2735572 and T allele of UCP2 rs17132534 were associated with higher diastolic blood pressure (P = 0.001; false discovery rate [FDR] = 0.009 and P = 8e–04; FDR = 0.009, respectively). We observed that the AATAG haplotype of UCP1 was associated with higher serum ApoB/ApoA1 (P = 0.008; FDR = 0.031) and ApoB levels (P = 0.008; FDR = 0.031). Moreover, the ACC haplotype of UCP3 was associated with a higher CVD risk score (P = 0.0036; FDR = 0.01).
Conclusions
Two UCP2 polymorphisms and haplotypes of UCP1 and UCP3 were associated with CVD risk factors. These findings suggest that UCPs may have a role in the development of CVD already in adolescents.
Similar content being viewed by others
Introduction
Cardiovascular diseases (CVDs) are the main cause of premature death and chronic disability worldwide.1 CVD events occur most frequently during or after the fifth decade of life; however, there is evidence indicating that the precursors of CVD have its origin in the first decade of life.2 Therefore, prevention is fundamental to reduce the incidence of these pathologies, especially in young people.
CVDs are a result of complex harmful interactions between environmental and genetic risk factors. Environmental factors include unhealthy diet, tobacco use or physical inactivity.3 However, efforts have been insufficient to decrease the prevalence and new pathogenic dimensions that come into play. Recent studies have described the association between some single-nucleotide polymorphisms (SNPs) with myocardial infarction4 and other cardiovascular complications.5 For example, uncoupling protein (UCP) genes have been associated with risk factors of CVD, such as prediabetes and type 2 diabetes mellitus (T2DM),6 overweight and obesity,7,8 plasma levels of cholesterol9 or hypertension (HT),10 mainly in adults over 50 years of age.
The most studied UCP genes are (i) UCP1, the main function of which is heat production through non-shivering thermogenesis in brown adipose tissue (BAT);11 (ii) UCP2 may have a regulating role in thermogenesis of BAT, seems to be involved in the control of reactive oxygen species (ROS) production,12,13 the modulation of insulin secretion14 and the regulation of mitochondrial fatty acid oxidation15 and (iii) UCP3, the role of which has been related to the coupling regulation of mitochondrial respiration in skeletal muscle mitochondria16 and fatty acid oxidation,17 and is a mediator of thermogenesis.18 The role played by UCPs in human physiology makes UCPs ideal targets against cardiovascular-associated pathologies. Indeed, several SNPs of UCP2 (rs660339, rs659366)19,20 and UCP3 (rs2075577, rs3781907, rs1800006 and rs1800849)6,19,21,22 have been associated with T2DM, overweight/obesity, serum total and LDL cholesterol and other cardiovascular risk markers. Nevertheless, poor evidence of CVD risk factors, especially in youth has been described.
Data obtained within the Healthy Lifestyle in Europe by Nutrition in Adolescence Cross-Sectional Study (HELENA-CSS) provide an excellent opportunity to study the association of UCP1, UCP2 and UCP3 SNPs with CVD risk factors in European adolescents. The HELENA study was designed to provide reliable data on nutrition and health-related variables in a relatively large sample of European adolescents from nine different countries and include information on 18 SNPs of UCP1, UCP2 and UCP3 genes, as well as a number of CVD risk factors. To our knowledge, UCP polymorphisms have not been identified in GWAS of body weight or body composition in adults or other age groups.
The aim of this study was therefore to examine the association of 18 UCP1, UCP2 and UCP3 SNPs (see Table 1) with CVD risk factors in European adolescents.
Materials and methods
Participants
The HELENA-CSS attempted to report the lifestyle and nutritional status of European adolescents. A total of 3865 participants (12–18 year old) of nine European countries (Greece, Germany, Belgium, France, Hungary, Italy, Sweden, Austria and Spain) were selected to be part of this study. They were randomly selected from public and private schools in each city between October 2006 and December 2007. We collected blood samples of one-third of these participants (N = 1155) with the consequent genetic analysis and clinical biochemistry assays. Finally, 1057 (552 girls) adolescents with UCP SNPs and CVD risk factor data were included in this study. Adolescents and the corresponding parents/guardians were fully informed about the aims and methods of the study such as inclusion criteria,23,24 and signed an informed written consent. Ethical guidelines of the Declaration of Helsinki 1964 (revision of Edinburgh 2000), Good Clinical Practice and legislation about clinical research in humans in each of the participating countries were respected by the study. Human research committees of each centre involved approved the protocol.25
Assessment of cardiovascular risk factors
A total of 30 mL of blood samples were drawn after a 10-h overnight fast at school between 0830 and 0900 h following a standardised blood collection protocol. Serum/plasma was centrifuged directly at the schools at 3500 r.p.m. (for 15 min, at room temperature). After centrifugation, they were stored and transported (4–7 °C) to the central laboratory (Bonn, Germany) where they were deposited at −80 °C as explained in detail elsewhere.26 Serum concentrations of cardiovascular risk factors were measured in centralised laboratories.
The CVD risk factors that were analysed included serum total cholesterol, high-density lipoprotein (HDL) cholesterol, low-density lipoprotein (LDL), ApoA1, ApoB, leptin, triglycerides and glucose, which were measured on the Dimension RxL Clinical Chemistry System (Dade Behring, Schwalbach, Germany) with enzymatic methods. Insulin was measured by a solid-phase two-site chemiluminescent immunometric assay with an Immulite 2000 analyser (DPC Biermann GmbH, Bad Nauheim, Germany). Homoeostasis model assessment (HOMA) was calculated ([glycaemia × insulin]/22.5) as resistance to insulin indicator, along with the Quantitative Insulin Sensitivity Check Index (QUICKI), which was calculated as 1/[log(insulin) + log(glycaemia)]. Blood pressure was measured with an automatic oscillometric device (OMRON M6). Adolescents quietly sat for 5 min before the measurements, conducted on the right arm in an extended position. Two measures of diastolic and systolic blood pressure (DBP and SBP, respectively) were taken 5 min apart, and the mean of both values (in mmHg) was used in analyses.
We computed a CVD risk score with the mean of the standardised value [(value − mean)/standard deviation] of the following variables: total cholesterol/HDL, triglycerides, HOMA, SBP and triceps and subscapular skinfolds.27 The characteristics of the study sample, including CVD risk factors, are shown in Table 2.
Genotyping
Blood for DNA extraction was collected in EDTA K3 tubes, stored at the Analytical Laboratory at the University of Bonn and then sent to the Genomic Analysis Laboratory at the Institut Pasteur de Lille (Lille, France). DNA was extracted from white blood cells with the Puregene kit (Qiagen, Courtaboeuf, France) and stored at 20 °C. Samples were genotyped by an Illumina System (Illumina Inc., San Diego, CA) and the software used was GoldenGate Inc. (San Francisco, CA). High rate of genotyping success was performed (≥97.8%) and each polymorphism respected the Hardy–Weinberg equilibrium (HWE) (P > 0.2 in all cases, Table 1). Several polymorphisms of the same genes showed linkage disequilibrium between them (Figs. 1 and 2).
Boxes with numbers refer to linkage disequilibrium (D′) between SNPs and boxes with no number mean 100% linkage (D′ = 1). Colour legend: Dark grey = high D′; white = low D′ (see Haploview documentation for further details; http://www.broad.mit.edu/mpg/haploview).
Boxes with numbers refer to linkage disequilibrium (D′) between SNPs and boxes with no number mean 100% linkage (D′ = 1). Colour legend: Dark grey = high D′; white = low D′ (see Haploview documentation for further details; http://www.broad.mit.edu/mpg/haploview).
Statistical analysis
Deviations from HWE were determined by means of an exact test and considering a P value of 0.05 as a threshold. Associations between genetic markers and CVD risk factors were assessed through linear models. Five inheritance models (dominant, recessive, log additive, codominant and overdominant) were used for all analyses, except in those where rs2071416, rs2735572 and rs17132534 SNPs were involved. These polymorphisms were analysed using only a dominant model due to the low number of minor homozygotes (minor allele frequency < 0.1, Table 1). Previous findings show the association between nonadditive models with UCPs, which indicates the interest of performance of these five models and compare the additive models with nonadditive ones.28 Adjustment variables were body mass index (calculated as weight in kilograms divided by height in metres squared), age, gender and centre. For each SNP, P values were computed using the likelihood ratio test between a model with the polymorphism and a null model without it. These analyses were performed with the “SNPassoc” R package.29 We considered the associations between all SNPs and each phenotype under a given heritage model such as the family test, that is, the number of tests were equal to the number of SNPs analysed for a given phenotype. We selected the significant genotype–phenotype associations to perform haplotype analysis, that is, only SNPs and phenotypes significantly associated were considered for next analyses. Given the exploratory nature of these analyses and the reduced number of independent tests (markers are in linkage disequilibrium), the Bonferroni correction could be too conservative.30 Instead of this method, we performed an exploratory selection of associations using an approach that controls the expected proportion of false positives (false discovery rate [FDR]).31 Therefore, associations with FDR < 0.1 were used in haplotype analyses.
Linkage disequilibrium between polymorphisms and haplotype block structures were evaluated with Haploview 4.2 (http://www.broad.mit.edu/mpg/haploview) and the R package haplo.stats.32 First, haplotype blocks were generated by the algorithm of four-gamete rules33 using Haploview. For each block, we tested if the observed frequencies of haplotypes were deviated from those expected under linkage equilibrium using “haplo.em” {haplo.stats} (P = 0 in all blocks). Finally, we assessed the association between haplotypes and phenotypes by means of a permutation procedure performed with haplo.score {haplo.stats}. Only additive and dominant models were considered given the low frequency of some haplotypes. For those significant associations, we performed regressions between haplotypes and phenotypes with the purpose of testing significant differences between haplotype levels. These regressions were performed with haplo.glm {haplo.stats}. Again, the FDR was calculated from the P values for differences between the reference haplotype (the most frequent) and other haplotypes.
Results
Association between UCP polymorphisms and CVD risk factors
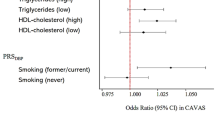
Two UCP2 SNPs were individually associated with CVD risk factors after multiple-comparison corrections with an FDR < 0.05 threshold. Associations with FDR < 0.1 were also selected as a screening method to further haplotype analyses (Fig. 3). All individual comparisons between genotypes and CVD risk factors are presented in the Supplementary file. We observed that the G major allele of rs2735572 SNP and the T major allele of rs17132534 SNP were associated with higher DBP under a dominant inheritance model (β coefficient = 0.04, P = 0.001; FDR = 0.009 and β coefficient = 0.04, P = 8e − 04; FDR = 0.009, respectively; β coefficients obtained from models with the response variable log transformed, Fig. 3).
Association between UCP polymorphism haplotypes and CVD risk factors
UCP1 block contains the rs12502572, rs11932232, rs6822807, rs6818140 and rs2071416 SNPs (Fig. 1). The AATAG haplotype of UCP1 was significantly associated with a higher ApoB/ApoA1 ratio than the reference GATAT haplotype (global P = 0.046; difference between groups = 0.06; 95% confidence interval [CI] = 0.02–0.10; P = 0.008; FDR = 0.031; under additive model; differences between groups obtained from models with the response variable log transformed, respectively). The AATAG haplotype was also associated with higher ApoB levels than the reference GATAT haplotype (global P = 0.045; difference between groups = 0.06; 95% CI = 0.02–0.10; P = 0.008; FDR = 0.031; under additive model). Also an association between the UCP3 block 2 (rs7930460, rs2075577 and rs2734828, Fig. 2) and the risk score was observed. The ACC haplotype was associated with a higher risk score compared with the ATC haplotype (global P = 0.008; difference between groups = 0.06; 95% CI = 0.02–0.10; P = 0.0036; FDR = 0.01; under dominant model).
Discussion
We observed that the UCP2 G and T alleles of the rs2735572 and rs17132534 SNPs were associated with higher DBP in European adolescents. Moreover, we found that the UCP1 AATAG haplotype was associated with higher serum ApoB/ApoA1 and ApoB levels. Finally, the UCP3 ACC haplotype was associated with a higher CVD risk score. Taken together, these findings suggest that UCPs may have an important role in cardiovascular health already in the first decade of life.
To our knowledge, this is the first study investigating the association between UCPs and CVD risk factors in European adolescents. Several studies with smaller sample sizes6,21,22,34 reported an association of single polymorphisms of UCP3 SNPs or combined haplotypes of UCP2/UCP3 with several CVD risk factors such as TC and LDL levels, insulin or HOMA in adults. In contrast, we observed no association of these UCP SNPs with CVD risk factors in European adolescents. These discordances may be due to the fact that they are population dependent, with possibly different allele frequencies and penetrance in these populations. Also differences in age, inter-country differences in lifestyle behaviours and sample sizes are important and could lead to differences across studies.
A plausible mechanism to partially explain the observed associations is that polymorphisms or haplotypes of UCPs could alter UCP functions and predispose to cardiovascular risk or an increased risk score (due to make up of cardiovascular risk factors). This dysfunction may explain the phenotypes observed with CVD risk through (i) dysfunction of the process of oxidation of fatty acids, leading to altered serum lipid levels such as TC, LDL, HDL or TG,9,15 (ii) in relation to ROS regulation mediated by UCP2, Pierelli et al.35 showed that knockout mice deletion of the UCP2 gene contributes to atherosclerosis lesion development and a significantly shorter lifespan. Several studies in humans and cultured cells suggested that excessive ROS production is involved in the atherosclerotic plaque formation and progression.36,37 Therefore, evidence suggests that decreasing ROS production is a remarkable target to prevent the atherosclerotic process. UCP2 negatively regulates intracellular ROS production,12,13 making it a potential therapeutic target for the treatment of vascular diseases, (iii) UCPs have also been related to blood pressure control. Dhamrait et al.38 described the role of UCPs in the regulation of angiotensin-converting enzyme (ACE). This enzyme plays a pivotal component of the endocrine renin–angiotensin system (RAS), also playing a key role in the regulation of the human circulation. ACE favours the rise of angiotensin II and aldosterone, leading to salt and water retention by the kidney, and to constriction of small blood vessels in the arterial tree. Taken together, these actions serve to elevate blood pressure. Moreover, Dhamrait et al.38 showed that some UCP3 and UCP2 SNPs were associated with higher age-adjusted ACE activity, which could contribute to a hypertension status, which is also consistent with our findings. CVDs are pathologies with a long-term latency period and modifiable cardiovascular risk factors, which make prevention fundamental, especially in these populations with genetic predisposition.
A limitation of our study is its cross-sectional nature. Our results should be considered carefully and studies with larger sample size could help to further confirm this possible genetic predisposition.
In conclusion, we observed an association between the UCP2 rs2735572 and rs17132534 SNPs with higher DBP in adolescents from nine European countries. We also observed a haplotype association of UCP1 and UCP3 with higher blood apolipoprotein levels and risk score, respectively. These findings suggest that UCPs may have an important role in the development of CVD predisposition already in European adolescents.
References
Roth, G. A. et al. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J. Am. Coll. Cardiol. 70, 1–25 (2017).
Shah, S. Primary prevention of cardiovascular disease. World Health Organ. 364, 937 (2011).
World Health Organization. Global status report on noncommunicable diseases 2010. World Health 176, http://whqlibdoc.who.int/publications/2011/9789240686458_eng.pdf (2010).
Nasibullin, T. R. et al. Genotype/allelic combinations as potential predictors of myocardial infarction. Mol. Biol. Rep. 43, 11–16 (2016).
Fiatal, S. & Ádány, R. Application of single-nucleotide polymorphism-related risk estimates in identification of increased genetic susceptibility to cardiovascular diseases: a literature review. Front. Public Health 5, http://journal.frontiersin.org/article/10.3389/fpubh.2017.00358/full (2018).
Hsu, Y.-H. et al. Genetic variants in the UCP2-UCP3 gene cluster and risk of diabetes in the Women’s Health Initiative Observational Study. Diabetes 57, 1101–1107 (2008).
Pascual-Gamarra, J. M. et al. Association between UCP1, UCP2, and UCP3 gene polymorphisms with markers of adiposity in European adolescents: the HELENA study. Pediatr. Obes. http://doi.wiley.com/10.1111/ijpo.12504, e12504 (2019).
Brondani, L. A. et al. Meta-analysis reveals the association of common variants in the uncoupling protein (UCP) 1-3 genes with body mass index variability. PLoS ONE 9, e96411 (2014).
Kotani, K. et al. The association between the uncoupling protein-1 gene A −3826G polymorphism and high-density lipoprotein cholesterol in a general japanese population: a consideration of the obesity status. J. Clin. Med. Res. 3, 319–324 (2011).
Kotani, K. et al. The uncoupling protein-1 gene −3826A/G polymorphism and hypertension in Japanese subjects. Clin. Chem. Lab. Med. 45, 1186–1189 (2007).
Golozoubova, V., Cannon, B. & Nedergaard, J. UCP1 is essential for adaptive adrenergic nonshivering thermogenesis. Am. J. Physiol. Endocrinol. Metab. 291, E350–E357 (2006).
Moukdar, F. et al. Reduced antioxidant capacity and diet-induced atherosclerosis in uncoupling protein-2-deficient mice. J. Lipid Res. 50, 59–70, (2009).
Arsenijevic, D. et al. Disruption of the uncoupling protein-2 gene in mice reveals a role in immunity and reactive oxygen species production. Nat. Genet. 26, 435–439 (2000).
Zhang, C. Y. et al. Uncoupling protein-2 negatively regulates insulin secretion and is a major link between obesity, beta cell dysfunction, and type 2 diabetes. Cell 105, 745–755 (2001).
Pecqueur, C., Alves-Guerra, C., Ricquier, D. & Bouillaud, F. UCP2, a metabolic sensor coupling glucose oxidation to mitochondrial metabolism? IUBMB Life 61, 762–767 (2009).
Vidal-Puig, A. J. et al. Energy metabolism in uncoupling protein 3 gene knockout mice. J. Biol. Chem. 275, 16258–16266 (2000).
Bezaire, V. et al. Constitutive UCP3 overexpression at physiological levels increases mouse skeletal muscle capacity for fatty acid transport and oxidation. FASEB J. 19, 977–979 (2005).
Riley, C. L. et al. The complementary and divergent roles of uncoupling proteins 1 and 3 in thermoregulation. J. Physiol. 594, 7455–7464 (2016).
Su, M. et al. UCP2 and UCP3 variants and gene–environment interaction associated with prediabetes and T2DM in a rural population: a case control study in China. BMC Med. Genet. 19, 1–9 (2018).
Andersen, G. et al. The frequent UCP2 −866G>A polymorphism protects against insulin resistance and is associated with obesity: a study of obesity and related metabolic traits among 17 636 Danes. Int. J. Obes. 37, 175–181 (2013).
Mottagui-Tabar, S. et al. Association of ADRB1 and UCP3 gene polymorphisms with insulin sensitivity but not obesity. Horm. Res. 69, 31–36 (2007).
Ochoa, M. C. et al. Association between obesity and insulin resistance with UCP2-UCP3 gene variants in Spanish children and adolescents. Mol. Genet. Metab. 92, 351–358 (2007).
Moreno, L. A. et al. Design and implementation of the healthy lifestyle in europe by nutrition in adolescence cross-sectional study. Int. J. Obes. 32, S4–S11 (2008).
Moreno, L. A. et al. Assessing, understanding and modifying nutritional status, eating habits and physical activity in European adolescents: the HELENA (Healthy Lifestyle in Europe by Nutrition in Adolescence) Study. Public Health Nutr. 11, 288–299 (2008).
Béghin, L. et al. Quality assurance of ethical issues and regulatory aspects relating to good clinical practices in the HELENA Cross-Sectional Study. Int. J. Obes. (Lond.) 32(Suppl. 5), S12–S18 (2008).
Gonzalez-Gross, M. et al. Sampling and processing of fresh blood samples within a European multicenter nutritional study: evaluation of biomarker stability during transport and storage. Int. J. Obes. (Lond.). 32(Suppl. 5), S66–S75 (2008).
Lobelo, F., Pate, R. R., Dowda, M., Liese, A. D. & Ruiz, J. R. Validity of cardiorespiratory fitness criterion-referenced standards for adolescents. Med. Sci. Sports Exerc. 41, 1222–1229 (2009).
Krishnan, M. et al. Analysis of association of gene variants with obesity traits in New Zealand European children at 6 years of age. Mol. BioSyst. 13, 1524–1533 (2017).
González, J. R. et al. SNPassoc: an R package to perform whole genome association studies. Bioinformatics 23, 644–645 (2007).
Sham, P. C. & Purcell, S. M. Statistical power and significance testing in large-scale genetic studies. Nat. Rev. Genet. 15, 335–346 (2014).
Qu, H.-Q., Tien, M. & Polychronakos, C. Statistical significance in genetic association studies. Clin. Investig. Med. 33, E266–E270 (2010).
Sinnwell, J. P. & Schaid, D. J. Statistical Analysis of Haplotypes with Traits and Covariates when Linkage Phase is Ambiguous (2016). http://www.mayo.edu/research/labs/statistical-genetics-genetic-epidemiology/.
Wang, N., Akey, J. M., Zhang, K., Chakraborty, R. & Jin, L. Distribution of recombination crossovers and the origin of haplotype blocks: the interplay of population history, recombination, and mutation. Am. J. Hum. Genet. 71, 1227–12342 (2002).
Salopuro, T. et al. Variation in the UCP2 and UCP3 genes associates with abdominal obesity and serum lipids: the Finnish Diabetes Prevention Study. BMC Med. Genet. 10, 94 (2009).
Pierelli, G. et al. Uncoupling protein 2: a key player and a potential therapeutic target in vascular diseases. Oxid. Med. Cell Longev. https://doi.org/10.1155/2017/7348372 (2017).
Chisolm, G. M. & Steinberg, D. The oxidative modification hypothesis of atherogenesis: an overview. Free Radic. Biol. Med. 28, 1815–1826 (2000).
Mallat, Z. et al. The relationship of hydroxyeicosatetraenoic acids and F2-isoprostanes to plaque instability in human carotid atherosclerosis. J. Clin. Invest. 103, 421–427 (1999).
Dhamrait, S. S. et al. Mitochondrial uncoupling proteins regulate angiotensin-converting enzyme expression: crosstalk between cellular and endocrine metabolic regulators suggested by RNA interference and genetic studies. BioEssays 38, S107–S118 (2016).
Acknowledgements
The HELENA Study is supported by contract FOOD-CT-2005-007034 from the European Community Sixth RTD Framework Programme. The study was supported by the Spanish Ministry of Education (FPU16/02127, FPU13/03410), by the University of Granada Plan Propio de Investigación 2016 (Excellence actions: Unit of Excellence on Exercise and Health [UCEES]), by the Junta de Andalucía, Consejería de Conocimiento, Investigación y Universidades, by the European Regional Development Fund (ERDF), ref. SOMM17/6107/UGR and by Redes Temáticas de Investigación Cooperativa RETIC grant Red SAMID RD16/0022.
Author information
Authors and Affiliations
Contributions
I.L., A.I.R., C.L., A.M., S.G., L.A.M., A.M., M.J.C., D.S.-T., J.M.P.-G. and J.R.R. designed the study; D.S.-T. performed all analyses; J.M.P.-G., D.S.-T. and J.R.R. wrote the initial draft and all co-authors significantly contributed to the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Pascual-Gamarra, J.M., Salazar-Tortosa, D.F., Labayen, I. et al. Association of UCP1, UCP2 and UCP3 gene polymorphisms with cardiovascular disease risk factors in European adolescents: the HELENA study. Pediatr Res 88, 265–270 (2020). https://doi.org/10.1038/s41390-019-0735-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-019-0735-7