Abstract
Objectives
To assess percent of patients undergoing multiple CT exams that leads to cumulative effective dose (CED) of ≥ 100 mSv and determine their age distribution.
Methods
Data was retrieved retrospectively from established radiation dose monitoring systems by setting the threshold value of 100 mSv at four institutions covering 324 hospitals. The number of patients with CED ≥ 100 mSv only from recurrent CT exams during a feasible time period between 1 and 5 years was identified. Age and gender distribution of these patients were assessed to identify the magnitude of patients in the relatively lower age group of ≤ 50 years.
Results
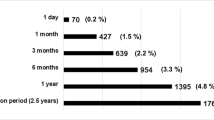
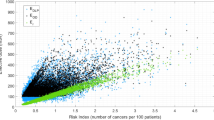
Of the 2.5 million (2,504,585) patients who underwent 4.8 million (4,819,661) CT exams during the period of between 1 and 5 years, a total of 33,407 (1.33%) patients received a CED of ≥ 100 mSv with an overall median CED of 130.3 mSv and maximum of 1185 mSv. Although the vast majority (72–86%) of patients are > 50 years of age, nearly 20% (13.4 to 28%) are ≤ 50 years. The minimum time to accrue 100 mSv was a single day at all four institutions, an unreported finding to date.
Conclusions
We are in an unprecedented era, where patients undergoing multiple CT exams and receiving CED ≥ 100 mSv are not uncommon. While underscoring the need for imaging appropriateness, the consideration of the number and percent of patients with high exposures and related clinical necessities creates an urgent need for the industry to develop CT scanners and protocols with sub-mSv radiation dose, a goal that has been lingering.
Key Points
• We are in an era where patients undergoing multiple CT exams during a short span of 1 to 5 years are not uncommon and a sizable fraction among them are below 50 years of age.
• This leads to cumulative radiation dose to individual patients at which radiation effects are of real concern.
• There is an urgent need for the industry to develop CT scanners with sub-mSv radiation dose, a goal that has been lingering.


Similar content being viewed by others
Abbreviations
- AAPM:
-
American Association of Physicists in Medicine
- BEIR:
-
Biological Effects of Ionizing Radiation Board
- CDS:
-
Clinical decision support
- CED:
-
Cumulative effective dose
- DLP:
-
Dose-length-product
- ED:
-
Effective dose
- IAEA:
-
International Atomic Energy Agency
- ICRP:
-
International Commission on Radiological Protection
- NCRP:
-
National Council on Radiation Protection and Measurements
- UNSCEAR:
-
United Nations Scientific Committee on Effects of Atomic Radiation
- WHO:
-
World Health Organization
References
United Nations Scientific Committee on the Effects of Atomic Radiation (2010) Sources and Effects of Ionizing Radiation. United Nations Scientific Committee on the Effects of Atomic Radiation. UNSCEAR 2008 Report. Volume I: Sources: Report to the General Assembly, Scientific Annexes A and B. New York. Accessed June 18, 2019
Holmberg O, Malone J, Rehani M, Mclean D, Czarwinski R (2010) Current issues and actions in radiation protection of patients. Eur J Radiol 76(1):15–19. https://doi.org/10.1016/j.ejrad.2010.06.033
National Council on Radiation Protection and Measurements (2009) Ionizing radiation exposure of the population of the United States. NCRP Report 160. NCRP Bethesda, MD
Rehani MM (2015) What makes and keeps radiation risks associated with CT a hot topic? AJR Am J Roentgenol 204(3). https://doi.org/10.2214/ajr.14.12860
Rogers LF (2001) Taking care of children. AJR Am J Roentgenol 176(2):287. https://doi.org/10.2214/ajr.176.2.1760287
Sternberg S (2001) CT scans in children linked to cancer. USA Today 2001 Jun 19. https://usatoday30.usatoday.com/news/nation/2001-01-22-scans.htm Published January 19, 2001. Accessed August 7, 2018
Richwine L (2009) U.S. probing more cases of CT radiation overexposure. Reuters Dec 7. https://www.reuters.com/article/us-scans-fda/u-s-probing-more-cases-of-ct-radiation-overexposure-idUSTRE5B638O20091207. Published December 7, 2009. Accessed August 7, 2018
Malone J, Guleria R, Craven C et al (2012) Justification of diagnostic medical exposures: some practical issues. Report of an International Atomic Energy Agency Consultation. Br J Radiol 85(1013):523–538. https://doi.org/10.1259/bjr/42893576
Pearce MS, Salotti JA, Little MP et al (2012) Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet 380(9840):499–505. https://doi.org/10.1016/S0140-6736(12)60815-0
Mathews JD, Forsythe AV, Brady Z et al (2013) Cancer risk in 680,000 people exposed to computed tomography scans in childhood or adolescence: data linkage study of 11 million Australians. BMJ 346:f2360. https://doi.org/10.1136/bmj.f2360
Rehani MM (2015) Looking into future: challenges in radiation protection in medicine. Radiat Prot Dosimetry 165(1–4):3–6. https://doi.org/10.1093/rpd/ncv071
Canellas R, Ackman JB, Digumarthy SR et al (2018) Submillisievert chest dual energy computed tomography: a pilot study. Br J Radiol 91(1082):20170735. https://doi.org/10.1259/bjr.20170735
Rehani MM, Berris T (2012) International Atomic Energy Agency study with referring physicians on patient radiation exposure and its tracking: a prospective survey using a web-based questionnaire. BMJ Open 2(5). https://doi.org/10.1136/bmjopen-2012-001425
International Atomic Energy Agency (IAEA) (2012) Radiation Protection of Patients (RPOP), Bonn Call for Action platform (https://www.iaea.org/resources/rpop/resources/bonn-call-for-action-platform). Published 2012. Updated 2019. Accessed August 7, 2018
Sodickson A, Baeyens PF, Andriole KP et al (2009) Recurrent CT, cumulative radiation exposure, and associated radiation-induced cancer risks from CT of adults. Radiology 251(1):175–184. https://doi.org/10.1148/radiol.2511081296
Brenner DJ (2010) Medical imaging in the 21st century — getting the best bang for the rad. N Eng J Med 362(10):943–945. https://doi.org/10.1056/nejme1000802
Griffey RT, Sodickson A (2009) Cumulative radiation exposure and cancer risk estimates in emergency department patients undergoing repeat or multiple CT. AJR Am J Roentgenol 192(4):887–892. https://doi.org/10.2214/ajr.08.1351
Desmond AN, O'Regan K, Curran C et al (2008) Crohn’s disease: factors associated with exposure to high levels of diagnostic radiation. Gut 57(11):1524–1529. https://doi.org/10.1136/gut.2008.151415
Smith-Bindman R, Moghadassi M, Wilson N et al (2015) Radiation doses in consecutive CT examinations from five university of California Medical Centers. Radiology 77(1):134–141. https://doi.org/10.1148/radiol.2015142728
Fazel R, Krumholtz HM, Wang Y et al (2009) Exposure to low-dose ionizing radiation from medical imaging procedures. N Engl J Med 361(9):849–857
Chen J, Einstein AJ, Fazel R et al (2010) Cumulative exposure to ionizing radiation from diagnostic and therapeutic cardiac imaging procedures. A population-based analysis. J Am Coll Cardiol 56:702–711
Einstein AJ, Weiner SD, Berheim A et al (2010) Multiple testing, cumulative radiation dose, and clinical indications in patients undergoing myocardial perfusion imaging. JAMA 304:2137–2144
Hendee WR, Becker GJ, Borgstede JP et al (2010) Addressing overutilization in medical imaging. Radiology 257(1):240–245. https://doi.org/10.1148/radiol.10100063
Stein EG, Haramati LB, Bellin E et al (2010) Radiation exposure form medical imaging in patients with chronic and recurrent conditions. J Am Coll Radiol 7:351–359. https://doi.org/10.1016/j.jacr.2009.12.015
De Mauri A, Brambilla M, Chiarinotti D, Matheoud R, Carriero A, De Leo M (2011) Estimated radiation exposure from medical imaging in hemodialysis patients. J Am Soc Nephrol 22:571–578. https://doi.org/10.1681/ASN.2010070784
(2007) The 2007 Recommendations of the International Commission on Radiological Protection. ICRP Publication 103. Ann ICRP 37(2–4):1–332. https://doi.org/10.1016/j.icrp.2007.10.003
United Nations Scientific Committee on the Effects of Atomic Radiation (2018) Sources, effects and risks of ionizing radiation UNSCEAR 2017 Report New York, NY: UNSCEAR http://wwwunscearorg/docs/publications/2017/UNSCEAR_2017_Annex-Bpdf Published March 2018. Accessed 10 February 2019
National Council of Radiation Protection and Measurements (2018) NCRP Commentary No. 27: Implications of recent epidemiologic studies for the linear-non threshold model and radiation protection. Bethesda, Maryland. Accessed August 7, 2018
National Research Council (2006) Health risks from exposure to low levels of ionizing radiation: BEIR VII phase 2. The National Academies Press, Washington, DC. https://doi.org/10.17226/11340
European Commission (2008) European guidance on estimating population doses from medical X-ray procedures. Radiation protection No 154. EC Brussels. Accessed August 7, 2018
American Association of Physicists in Medicine (AAPM) (2008) Task Group 23 on the Diagnostic Imaging Council CT Committee. The Measurement, Reporting, and Management of Radiation Dose in CT. AAPM Report No. 96. Maryland: AAPM [cited 2019 Mar 16]. https://www.aapm.org/pubs/reports/RPT_96.pdf
Brambilla M, Vassileva J, Kuchcinskac A, Rehani MM (2019) Multinational data on cumulative radiation exposure of patients from recurrent radiological procedures: call for action. Eur Radiol. https://doi.org/10.1007/s00330-019-06528-7
OECD Organization for Economic Co-operation and Development(2017) Health at a glance 2017: OECD indicators. OECD Publishing, Paris. https://doi.org/10.1787/health_glance-2017-en
Rosenthal DI, Weilburg JB, Schultz T et al (2006) Radiology order entry with decision support: initial clinical experience. J Am Coll Radiol 3:799–806
Sistrom CL, Dreyer KJ, Dang PP et al (2009) Recommendations for additional imaging in radiology reports: multifactorial analysis of 5.9 million examinations. Radiology 253(2):453–461. https://doi.org/10.1148/radiol.2532090200
Weilburg JB, Sistrom CL, Rosenthal DI et al (2017) Utilization management of high-cost imaging in an outpatient setting in a large stable patient and provider cohort over 7 years. Radiology 284(3):766–776. https://doi.org/10.1148/radiol.2017160968
Rehani MM, Melick ER, Alvi RM et al (2019) Patients undergoing recurrent CT exams: Assessment of patients with non-malignant diseases, reasons for imaging and imaging appropriateness. Eur Radiol. https://doi.org/10.1007/s00330-019-06551-8
Rehani M, Frush D (2010) Tracking radiation exposure of patients. Lancet 376(9743):754–755. https://doi.org/10.1016/S0140-6736(10)60657-5
Seuri R, Rehani MM, Kortesniemi M (2013) How tracking radiologic procedures and dose helps: experience from Finland. AJR Am J Roentgenol 200(4):771–775. https://doi.org/10.2214/AJR.12.10112
Rehani MM, Berris T (2014) Templates and existing elements and models for implementation of patient exposure tracking. Radiat Prot Dosimetry 158(1):36–42. https://doi.org/10.1093/rpd/nct185
Akagi M, Nakamura Y, Higaki T et al (2019) Deep learning reconstruction improves image quality of abdominal ultra-high-resolution CT. Eur Radiol. https://doi.org/10.1007/s00330-019-06170-3
American Association of Physicists in Medicine (AAPM) (2019) Estimating patient organ dose with computed tomography: a review of present methodology and required DICOM information: a Joint Report of AAPM Task Group 246 and the European Federation of Organizations for Medical Physics (EFOMP). https://www.aapm.org/pubs/reports/RPT_246.pdf
Guberina N, Suntharalingam S, Naßenstein K et al (2018) Verification of organ doses calculated by a dose monitoring software tool based on Monte Carlo simulation in thoracic CT protocols. Acta Radiol 59(3):322–326. https://doi.org/10.1177/0284185117716199
Guberina N, Forsting M, Suntharalingam S et al (2017) Radiation dose monitoring in the clinical routine. Rofo 189(4):356–360. https://doi.org/10.1055/s-0042-116684
Iriuchijima A, Fukushima Y, Ogura A (2018) Comparison of organ dose calculation using Monte Carlo simulation and in-phantom dosimetry in CT examination. Nihon Hoshasen Gijutsu Gakkai Zasshi 74(2):166–171. https://doi.org/10.6009/jjrt.2018_JSRT_74.2.16
Acknowledgements
The authors sincerely acknowledge the subject matter expertise provided by Prof. Fred Mettler (Emeritus Professor, University of New Mexico) and statistical assistance by Dr. Hui Zheng of MGH, and of Matthew Hough, at AdventHealth, for his aid in determining typical institutional radiation doses.
Funding
The authors declare that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Madan Rehani.
Conflict of interest
The authors declare that they have no conflict of interest.
Statistics and biometry
Dr. Hui Zheng, statistician, kindly provided statistical advice for this manuscript. He has been acknowledged.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained wherever IRB was available.
Institutional Review Board approval was not required at some as indicated in the manuscript.
Methodology
• Retrospective
• Observational
• Multicenter study
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rehani, M.M., Yang, K., Melick, E.R. et al. Patients undergoing recurrent CT scans: assessing the magnitude. Eur Radiol 30, 1828–1836 (2020). https://doi.org/10.1007/s00330-019-06523-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-06523-y