Abstract
Hormones are substances that serve as chemical communication between cells. They are unique biological molecules that affect multiple organ systems and play a key role in maintaining homoeostasis. In this role, they are usually produced from a single organ and have defined target organs. However, hormones can affect non-target organs as well. As such, biochemical and hormonal abnormalities can be associated with anatomic changes in multiple target as well as non-target organs. Hormone-related changes may take the form of an organ parenchymal abnormality, benign neoplasm, or even malignancy. Given the multifocal action of hormones, the observed imaging findings may be remote from the site of production, and may actually be multi-organ in nature. Anatomic findings related to hormone level abnormalities and/or laboratory biomarker changes may be identified with imaging. The purpose of this image-rich review is to sensitize radiologists to imaging findings in the abdomen and pelvis that may occur in the context of hormone abnormalities, focusing primarily on sex hormones and their influence on these organs.



















Similar content being viewed by others
References
Conn P.M (2005). Introduction to Endocrinology. In: Melmed S., Conn P.M. (eds) Endocrinology. Humana Press: Totowa.
Hata S, Miki Y, Saito R, et al. (2013) Aromatase in human liver and its diseases. Cancer Medicine 2:305-315.
Yager JD, Davidson NE. (2006) Estrogen carcinogenesis in breast cancer. N Engl J Med; 354:270-282.
Onstad MA, Schmandt RE, Lu KH. (2016) Addressing the role of obesity in endometrial cancer risk, prevention, and treatment. J Clin Oncol; 34: 4225-4230
Harada N, Ota H, Yoshimura N, Katsuyama T, Takagi Y. (1998) Localized aberrant expression of cytochrome P450 aromatase in primary and metastatic malignant tumors of human liver. J Clin Endocrinol Metab; 83: 697-702.
Wenniger LM, Terpstra V, Beuers U. (2010) Focal nodular hyperplasia and hepatic adenoma: epidemiology and pathology. Dig Surg; 27:24-31.
Kaltenbach TE, Engler P, Kratzer W, et al. (2016) Prevalence of benign focal liver lesions: ultrasound investigation of 45,319 hospital patients. Abdom Radiol; 41:25-32.
Karhunen PJ. (1986) Benign hepatic tumours and tumour like conditions in men. J Clin Pathol; 39:183-188.
Venturi A, Piscaglia F, Vidili G, et al. (2007) Diagnosis ad management of hepatic focal nodular hyperplasia. J Ultrasound; 10:116-127.
Grazioli L, Abrosini R, Frittoli B, Grazioli M, Morone M. (2017) Primary benign liver lesions. Eur J Radiol; 95: 378-398.
Fodor M, Primavesi F, Braunwarth E, et al. (2018) Indications for liver surgery in benign tumours. Eur Surg; 50: 125-131.
Ringe KI, Husarik DB, Sirlin CB, Merkle EM. (2010) Gadoxetate disodium-enhanced MRI of the liver: part I, protocol optimization and lesion appearance in the noncirrhotic liver. Am J Roentgenol; 195:13-28.
Grazioli L, Bondioni MP, Haradome H, et al. (2012) Hepatocellular adenoma and focal nodular hyperplasia: value of gadoxetic acid-enhanced MR imaging in differential diagnosis. Radiology; 262: 520-529.
Casarella WJ, Knowles DM, Wolff M, Johnson PM. (1976) Focal nodular hyperplasia and liver cell adenoma: radiologic and pathologic differentiation. Am J Roentgenol; 131:393-402.
Venkatesh K. (2014) Liver masses: a clinical, radiological, and pathological perspective for: Perspectives in clinical gastroenterology and hepatology. Clin Gastroenterol Hepatol; 12: 1414-1429.
Virgilio E, Cavallini M. (2018) Managing focal nodular hyperplasia of the liver: surgery or minimally invasive approaches? A review of the preferable treatment options. Anticancer Res; 38: 33-36.
Kuo YH, Wang JH, Lu SN, et al. (2009) Natural course of hepatic focal nodular hyperplasia: a long-term follow-up study with sonography. J Clin Ultrasound; 37: 132-137.
Agrawal S, Agarwal S, Arnason T, et al. (2015) Management of hepatocellular adenoma: recent advances. Clin Gastroenterol Hepatol; 7:1221-1230
Stoot J, Coelen R, de Jong MC, Dejong C. (2010) Malignant transformation of hepatocellular adenomas into hepatocellular carcinomas: a systematic review including more than 1600 adenoma cases. HPB (Oxford); 12:509-522.
Grazioli L, Federle M, Brancatelli G, et al. (2001) Hepatic adenomas: imaging and pathologic findings. Radiographics; 21: 877-894.
Van Aalten SM, Thomeer MGJ, Terkivatan T, et al. (2011) Hepatocellular adenomas: correlation of MR imaging findings with pathologic subtype classifications. Radiology; 261:172-181.
Reizine E, Amaddeo G, Pigneur F, et al. (2018) Quantitative correlation between uptake of Gd-BOPTA on hepatobiliary phase and tumor molecular features in patients with benign hepatocellular lesions. Eur Radiol.https://doi.org/10.1007/s00330-018-5438-7
Guo Y, Li W, Xie Z, et al. (2017) Diagnostic value of Gd-EOB-DTPA-MRI for hepatocellular adenoma: a meta-analysis. J Cancer; 8:1301-1310.
Agarwal S, Fuentes-Orrego JM, Amason T, et al. (2014) Inflammatory hepatocellular adenomas can mimic focal nodular hyperplasia on gadoxetic acid-enhanced MRI. Am J Roentgenol; 203: W408-414.
Cobey FC, Salem RR. (2004) A review of liver masses in pregnancy and a proposed algorithm for their diagnosis and management. Am J Surg; 187: 181-191.
Thomeer MG, Broker M, Verheij J, et al. (2016) Hepatocellular adenoma: when and how to treat? Update of current evidence. Therap Adv Gastroenterol; 9: 898-912.
Almashhrawi AA, Ahmed KT, Rahman RN, Hammoud GM, Ibdah JA. (2013) Liver diseases in pregnancy: diseases not unique to pregnancy. World J Gastroenterol; 19: 7630-7638.
Bonnar J. (1987) Coagulation effects of oral contraception Am J Obstet Gynecol; 157:1042-1048.
Bissonnette J, Durand F, de Raucourt E, et al. (2015) Pregnancy and vascular liver disease. J Clin Exp Hepatol; 5:41-50.
Shin N, Kim YH, Xu H, et al. (2016) Redefining Budd-Chiari syndrome: a systematic review. World J Hepatol; 8: 691-702.
Dilawari J.B., Bambery P., Chawla Y. (1994) Hepatic outflow obstruction (Budd-Chiari syndrome). Experience with 177 patients and a review of the literature. Medicine (Baltimore);73:21–36.
Brancatelli G, Vilgrain V, Federle MP, et al. (2007) Budd-Chiari syndrome: spectrum of imaging findings. Am J Roentgenol; 188: W168-W176.
Ferra H, Behrens G, Lopera J. (2012) Budd-Chiari syndrome. Am J Roentgenol; 199: 737-745.
Vilgrain V, Lewin M, Vons C, et al. (1999) Hepatic nodules in Budd-Chiari syndrome: imaging features. Radiology; 210:443–450
Brancatelli G, Federle MP, Grazioli L, Golfieri R, Lencioni R. (2002) Large regenerative nodules in Budd- Chiari syndrome and other vascular disorders of the liver: CT and MR imaging findings with clinico- pathologic correlation. Am J Roentgenol; 178:877–883.
Ruh J, Malago M, Busch Y, et al. (2005) Management of Budd-Chiari syndrome. Dig Dis Sci; 50:540–546
Jha RC, Khera SS, Kalaria AD. (2018) Portal vein thrombosis: imaging the spectrum of diseases with an emphasis on MRI features. Am J Roentgenol; 211:14-24.
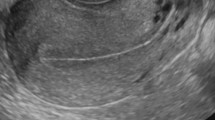
Davidson KG, Dubinsky TJ. (2003) Ultrasonographic evaluation of the endometrium in postmenopausal vaginal bleeding. Radiol Clin N Am; 41:769-780.
Smith-Bindman R, Kerlikowske K, Feldstein VA, et al. (1998) Endovaginal ultrasound to exclude endometrial cancer and other endometrial abnormalities. JAMA; 280:1510-1517.
Chandra V, Kim JJ, Benbrook DM, Dwivedi A, Rai R. (2016) Therapeutic options for management of endometrial hyperplasia. J Gynecol Oncol; 27:e8.
Freeman SJ, Aly AM, Kataoka MY, et al. (2012) The revised FIGO staging system for uterine malignancies: implications for MR imaging. Radiographics; 32:1805-1827.
Achiron R, Grisaru D, Golan-Porat N, Lipitz S. (1996) Tamoxifen and the uterus: an old drug tested by new modalities. Ultrasound Obstet Gynecol; 7:374-378.
Nougaret S, Horta M, Sala E, et al. (2018) Endometrial cancer MRI stating: updated guidelines of the European Society of Urogenital Radiology. Eur Radiol. https://doi.org/10.1007/s00330-018-5515-y
Huo D, Anderson D, Palmer JR, Herbst AL. (2017) Incidence rates and risks of diethylstilbestrol-related clear-cell adenocarcinoma of the vagina and cervix: update after 40-year follow up. Gynecologic Oncology; 146:566-571.
Gilles R, Michel G, Chancelier MD, Vanel D, Masselot J. (1993) Case report: clear cell adenocarcinoma of the vagina: MR features. Br J Radiol;66:168-70.
Parikh JH, Barton DPJ, Ind TEJ, Sohaib SA. (2008) MR imaging features of vaginal malignancies. Radiographics; 28:49-63.
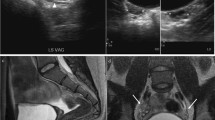
Williams T, Mortada R, Porter S. (2016) Diagnosis and treatment of polycystic ovary syndrome. Am Fam Phys; 94:106-113.
Lee TT, Rausch ME. (2012) Polycystic ovarian syndrome: role of imaging in diagnosis. Radiographics; 32: 1643-1657.
Lujan ME, Chizen DR, Pierson RA. (2008) Diagnostic criteria for polycystic ovary syndrome: pitfalls and controversies. J Obstet Gynaecol Can; 30: 671-679.
Teede HJ, Misso ML, Costelo MF, et al. (2018) International PCOS Network. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Clin Endocrinol. https://doi.org/10.1111/cen.13795
Fitzgerald S, Divasta A, Gooding H. (2018) An update on PCOS in adolescents. Curr Opin Pediatr; 30:459-465.
Babagbemi KT, Arleo EK, Asrani AV, Troiano RN. (2013) Emergent complications of assisted reproduction: expecting the unexpected. Radiographics; 33:229-244.
Lurain JR. (2010) Gestational trophoblastic disease I: epidemiology, pathology, clinical presentation, and diagnosis of gestational trophoblastic disease, and management of hydatidiform mole. Am J Obstet Gynecol; 203: 531-539.
Lurain JR. (2011) Gestational trophopblastic disease II: classification and management of gestational trophoblastic neoplasia. Am J Obstet Gynecol; 204: 11-18.
Shaaban AM, Rezvani M, Haroun RR, et al. (2017) Gestational trophoblastic disease: clinical and imaging features. Radiographics; 37: 681-700.
Stenman UH, Alfthan H, Hotakainen K. (2004) Human chorionic gonadotropin in cancer. Clin Biochem; 37:549-561.
Hotakainen K. (2002) The free beta-subunit of human chorionic gonadotropin as a prognostic factor in renal cell carcinoma. Br J Cancer; 86:185-189.
Shimomura T. (2005) Sarcomatoid renal cell carcinoma with a chromophobe component producing beta-human chorionic gonadotropin. Int J Urol; 12: 835-837.
Rukundo J, Ntasumbumuyange D, Small M, Rulisa S, Bazzett-Matabele L. (2017) Theca lutein cysts in the setting of primary hypothyroidism. Ultrasound in Obstetrics and Gynecology; 50: EP25.13.
Jung BG, Kim H. (2001) Severe spontaneous ovarian hyperstimulation syndrome with MR findings. J Comput Assist Tomogr; 25: 215-217.
Woodward PJ, Sohaey R, Mezzetti TP. (2001) Endometriosis: radiologic-pathologic correlation. Radiographics; 21: 193-216.
Glastonbury CM. (2002) The shading sign. Radiology; 224:199-201.
Corwin MT, Gerscovich EO, Lamba R, Wilson M, McGahan JP. (2013) Differentiation of ovarian endometriomas from hemorrhagic cysts at MR imaging: utility of the T2 dark spot sign. Radiology; 271:126-132.
McDermott S, Oei TN, Iyer VR, Lee SI. (2012) MR imaging of malignancies arising in endometriomas and extra-ovarian endometriosis. Radiographics; 32:845-863.
Levine D, Brown DL, Andreotti RF, et al. (2010) Management of asymptomatic ovarian and other adnexal cysts imaged at US: Society of Radiologists in Ultrasound consensus conference statement. Radiology; 256:943-954.
Outware EK, Wagner BJ, Mannion C, et al. (1998) Sex cord-stromal and steroid cell tumors of the ovary. Radiographics; 18: 1523-1546.
Jung SE, Rha SE, Lee JM, et al. (2005) CT and MRI findings of sex cord-stromal tumor of the ovary. Am J Roentgenol; 185:207-215.
Horta M, Cunha TM, Marques RC, Felix A. (2014) Ovarian Sertoli-Leydig cell tumor with heterologous elements of gastrointestinal type associated with elevated serum alpha-fetoprotein level: an unusual case and literature review. Radiology Case; 8:30-41.
McGill FM, Ritter DB, Rickard CS, et al. (1999) Krukenberg tumors: can management be improved? Gynecol Obstet Invest; 48:61-65.
Bacchus H. (ed) (1975) Amenorrhea. In: Essentials of Gynecologic and Obstetric Endocrinology. Springer: Dordrecht. https://doi.org/10.1007/978-94-011-9834-9_6.
Syed FA, Oursler MJ, Hefferanm TE, et al. (2008) Effects of estrogen therapy on bone marrow adipocytes in postmenopausal osteoporotic women. Osteoporos Int; 19:1323-1330.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kurzbard-Roach, N., Jha, P., Poder, L. et al. Abdominal and pelvic imaging findings associated with sex hormone abnormalities. Abdom Radiol 44, 1103–1119 (2019). https://doi.org/10.1007/s00261-018-1844-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-018-1844-1